Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 2
Aim: To study change in ocular surface indices in low and high myopia patient’s undergoing Small Incision Lenticule Extraction (SMILE) surgery.
Materials and methods: This was a prospective interventional study. We included 100 myopia patients (50 low myopia <5.0 D and 50 high myopia ≥ 5.0 D). Ocular Surface Disease Index Score (OSDI), Schirmer I Test (SIT) and Tear Breakup Time (TBUT) and other parameters were noted one week before and one week, four weeks, three months’ post-surgery.
Results: Mean values of SIT (mm/5 min) (low myopia is preoperative one week 29.6, postoperative one week 27.64, four weeks 28.75, three months 29.8 and in high myopia is preoperative one week 30.39, postoperative one week 28.67, four weeks 28.85, three months 30.77) showed significant fall in post-operative one week with continuous improvement thereafter, leading to comparable values with baseline in both subgroups. Similar trends were seen with mean values of OSDI (low myopia is preoperative one week 5.21, postoperative one week 12.14, four weeks 9.33, three months 4.72 and in high myopia is preoperative one week 4.07, postoperative one week 13.38, four weeks 9.36, three months 5.24) in both the groups. Mean values of TBUT (secs) (low myopia I preoperative one week 10.6, postoperative one week 8.83, four weeks 9.44, three months 10.17 and in high myopia is preoperative one week 11.2, postoperative one week 8.19, four weeks 9.17, three months 10.48) also showed significant fall in values postoperatively and then normalising in both groups.
Conclusion: As a treatment option, SMILE offers excellent refraction correction, along with complete recovery for dry eye symptoms in both high and low myopia patients.
Dry eye; Ocular surface disease index score; Small incision lenticule extraction; Tear break up time
Small Incision Lenticule Extraction (SMILE) surgery is the most recent technique available for refractive error correction. The advancement which distinguishes it from conventional Femtosecond Laser-Assisted Laser In-situ Keratomileusis (FS- LASIK) is the better technique of minimal corneal incision to extract lenticule after its generation [1].
Correcting high myopia with SMILE is safe and effective in the long-term, but the procedure significantly increases corneal High Order Aberrations (HOA) [2]. HOA can adversely influence visual outcomes due to glare, halo and reduced contrast sensitivity and can also lead to increase duration of dry eyes symptoms.
SMILE has advantages of lesser dry eye symptoms and early recovery after procedure as it is less damaging to corneal tissue with minimal nerve disruption. The smaller incision maintains biomechanical stability and corneal strength [3]. But, the procedure is mainly applicable in myopia particularly high myopia, leaving behind the patients of far-sightedness and astigmatism, though, with time its treatment range is expanding [4].
The main disadvantage is its inapplicability in patients with higher-order aberrations and the hypermetropia patients. The surgeon needs to perform a requisite number of SMILE surgeries before producing perfect results with minimal complications [5].
Previous studies have shown that SMILE surgery has better corneal sensitivity, faster recovery and satisfactory results in cases of moderate myopia [6-8]. With the unfolding experience of this newer treatment option, its use and results in different groups of myopes are variable [9-12].
Overall, there is still a lesser number of studies in literature and there is scope for its further exploration. Thus we did this study to compare ocular surface indices among patients with low and high myopia who underwent SMILE surgery.
A prospective interventional study was done from 2018 to 2020 during which a total of 100 myopia patients, i.e., 200 eyes (50 patients with low myopia and 50 patients with high myopia) were included after obtaining written informed consent from all the patients. The study was approved by the Institutional Ethical Committee (IEC) and with complete adherence to principles of Declaration of Helsinki.
The sample size calculation was based on the study of Qiu, et al., [13] where changes in the Schirmer I test (SIT) values were taken into account following SMILE surgery. They observed that pre-operative Schirmer I test values were 16.44 ± 3.43 and post-operative 1 week were 14.38 ± 2.87. Considering these values for reference, the minimum required sample size for the present study with 99% study power and 1% level of significance, was 57 patients. Further, taking 20% as lost to follow up, the total sample size to be taken was 72 patients. To reduce the margin of error, the total sample size taken was 100 patients.
Myopia patients, age ≥ 21 years, with no previous refractive surgery were included in the study. Patients with known dry eye disease, ocular surface disorders and systemic diseases/comorbidities were excluded.
After satisfying the eligibility criteria; age, gender and profession of the patients were recorded. The near and distant vision of patients was recorded. Corrected Distance Visual Acuity (CDVA) was assessed. The onset of myopia and the duration of use of spectacles or contact lens were noted. Patients were advised to stop use of contact lens 4 weeks prior to surgery.
To assess dry eye symptoms, an Ocular Surface Disease Index (OSDI) questionnaire was given and enquired for any symptoms. The same person conducted Tear Breakup Time (TBUT) followed by Schirmer I test after ten mins gap, in a similar room with alike humid and light conditions, minimizing environmental and weather effect [14].
TBUT was calculated as time in seconds between the last blink and the appearance of the dry spot as shown in Figure 1a. On slit lamp, a wet fluorescein (1 mg/strip) impregnated strip was touched in the lower fornix and the patient was asked to blink a few times before examination. Measurement was taken as a mean of three successive blinks. Break-up time of ≤ 10 seconds was considered positive, indicative of dry eye.
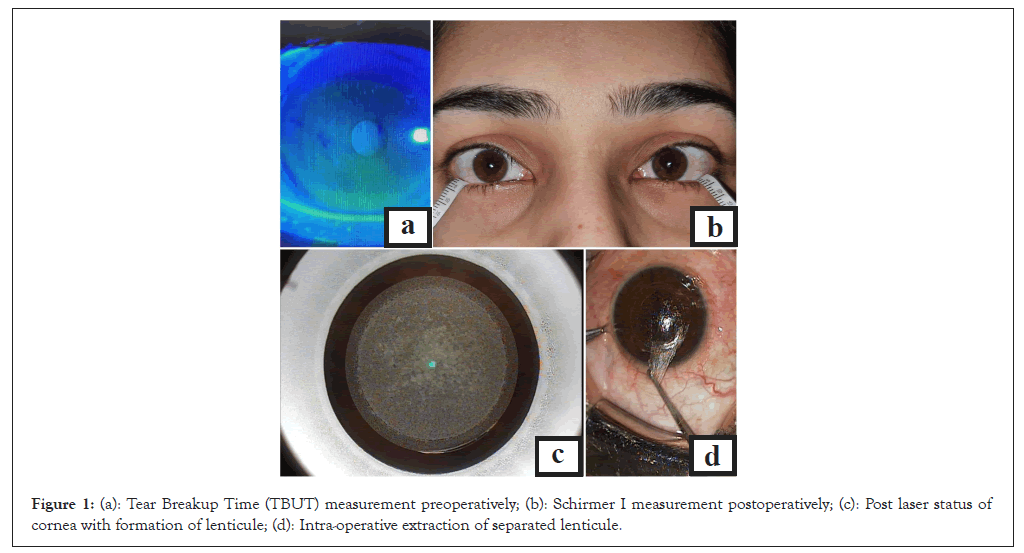
Figure 1: (a): Tear Breakup Time (TBUT) measurement preoperatively; (b): Schirmer I measurement postoperatively; (c): Post laser status of cornea with formation of lenticule; (d): Intra-operative extraction of separated lenticule.
Schirmer I test was done using 5 mm × 35 mm sterile strips of Whatman No.41 filter paper inserted in the lower cul-de-sac at the junction of medial two-third and lateral one-third of the lid as shown in Figure 1b. Adequate care was taken during the procedure to ensure that the paper did not touch the cornea, to avoid reflex tearing. At the end of five minutes, the strips were removed and the length of filter paper moistened was noted starting from the fold [15].
SMILE surgery
Patients underwent SMILE surgery of both eyes in the same sitting after thorough counseling. Topical proparacaine 0.5% was instilled preoperatively in both eyes. Infrared light was used after activation of suction to confirm the centration of docking.
A 500 kHz femtosecond laser was used to create the intrastromal lenticule as shown in Figure 1c. The optical zone was between 6.0 mm (194 eyes) and 6.5 mm (6 eyes) depending on pupil size. Cap thickness was from 110 microns to 120 microns. Energy offset was kept at 28. Rest standard parameters were used.
The refractive lenticule was separated from the surrounding stroma by blunt dissection via the small side-cut incision, first in the anterior plane followed by the posterior plane. The separated lenticule was extracted via the side-cut incision as shown in Figure 1d. The inbuilt slit-illumination laser system was used to assess the cap apposition. There were nil intra-operative complications (Figures 1a-1d).
Post-operative care
Steroid antibiotic combination was used in tapering doses for four weeks. Lubricating drops were advised for eight weeks and then as per need. One patient developed raised Intraocular Pressure (IOP) after 1 week, possibly due to topical steroid use and was managed by anti-glaucoma medications for 3 weeks and switching from steroid to loteprednol. The outcome measures were changes in ocular surface indices like OSDI, SIT and TBUT during the follow-up period of 12 weeks.
Statistical analysis
Wilcoxon signed-rank test was used for pre and post-procedure comparison. A statistically significant P value of <0.05 considered. Data were analyzed on Statistical Package for Social Sciences (SPSS) version 21.0.
A total of 50 patients with both low and high myopia were analyzed (100 eyes in each group). The mean age of the study population was 23.99 ± 3.49 years with 64% females and 36% males. Professionally, 68% of the population were students. It was noted that 26% of patients with low myopia and 38% of patients with high myopia were also using contact lens occasionally. Table 1 shows the comparative distribution of baseline characteristics of the study patients (Table 1).
| Socio-demographic characteristics | Low myopia (n=50) | High myopia (n=50) | Total | P-value |
|---|---|---|---|---|
| Age (years) | ||||
| Mean ± SD | 24.7 ± 4.27 | 23.28 ± 2.31 | 23.99 ± 3.49 | 0.109$ |
| Median (25th-75th percentile) | 24 (22-25) | 23 (21-25) | 24 (21.75-25) | |
| Range | 21-41 | 20-28 | 20-41 | |
| Gender | ||||
| Female | 35 (70%) | 29 (58%) | 64 (64%) | 0.211* |
| Male | 15 (30%) | 21 (42%) | 36 (36%) | |
| Onset of refractive error (years) | ||||
| Mean ± SD | 15.04 ± 3.24 | 12.55 ± 2.93 | 13.8 ± 3.32 | 0.0002$ |
| Median (25th-75th percentile) | 15 (13-17) | 13 (11-14) | 14 (12-15) | |
| Range | 7-23 | 6.5-22 | 6.5-23 | |
| Duration of spectacles (years) | ||||
| Mean ± SD | 8.93 ± 4.2 | 10.08 ± 3.28 | 9.5 ± 3.8 | 0.033$ |
| Median (25th-75th percentile) | 9 (6-10.875) | 11 (8-12) | 9 (7-12) | |
| Range | 2-25 | 2-15 | 2-25 | |
| Profession | ||||
| Banker | 1 (2%) | 2 (4%) | 3 (3%) | 0.188# |
| Doctor | 1 (2%) | 1 (2%) | 2 (2%) | |
| Fitness trainer | 0 (0%) | 2 (4%) | 2 (2%) | |
| Housewife | 9 (18%) | 2 (4%) | 11 (11%) | |
| Private job | 3 (6%) | 7 (14%) | 10 (10%) | |
| Student | 34 (68%) | 34 (68%) | 68 (68%) | |
| Teacher | 2 (4%) | 2 (4%) | 4 (4%) | |
Note: (*): Chi square test; (#): Fisher exact test; ($): Mann Whitney test; SD: Standard Deviation.
Table 1: Socio-demographic characteristics in low and high myopia groups.
Pre-operatively, all eyes had CDVA of 0.0 or better on logarithm of the Minimum Angle of Resolution (logMAR). After surgery on the post-operative one week, 93% of eyes in each group had unaided visual acuity of logMAR 0.0 or better which improved to 96.5% cumulative (94% in the high myopia group and 99% in the low myopia group) at three months. All 100% eyes had logMAR 0.0 or better corrected vision, showing a complete recovery in the CDVA within three months.
Dry eye symptoms were assessed objectively by SIT and TBUT. In the current study, the median pre-operative Schirmer I test values significantly decreased at post-operative one week (p=0.001) followed by an increase by four weeks and till three months (35 vs. 30 vs. 30 vs. 35) such that the final values at three months were comparable to the preoperative values (p>0.05) (Figure 2).
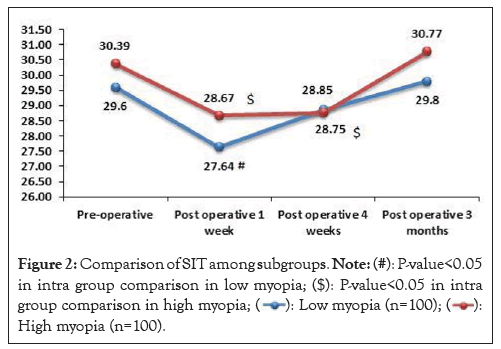
Figure 2: Comparison of SIT among subgroups. Note: (#): P-value<0.05
in intra group comparison in low myopia; ($): P-value<0.05 in intra
group comparison in high myopia;  High myopia (n=100).
High myopia (n=100).
A relatively similar trend was seen among high myopes as well. It was noted that the median pre-operative Schirmer test values showed a significant decrease at post-op one week (p=0.002), staying low till four weeks (p=0.004) and thereafter increasing at three months (35 vs. 30 vs. 30 vs. 35) such that the final values at 3 months were comparable to the preoperative values (p>0.05).
In comparison, among the two groups of low and high myopes, there was no significant difference in the Schirmer test values at various time intervals (p>0.05).
TBUT showed a significant fall in the values at post-operative one week, with values remaining significantly lower than the baseline at four weeks and three months. Amongst the two groups, there was no difference in the TBUT trends (p>0.05) (Figure 3).
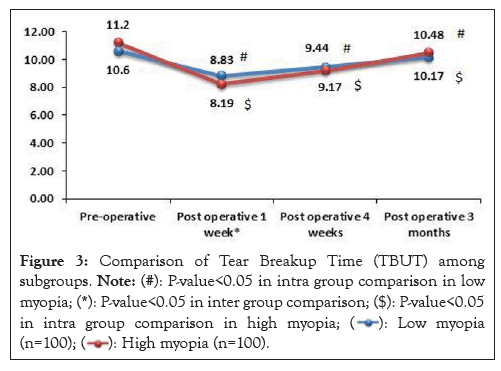
Figure 3: Comparison of Tear Breakup Time (TBUT) among
subgroups. Note: (#): P-value<0.05 in intra group comparison in low
myopia; (*): P-value<0.05 in inter group comparison; ($): P-value<0.05
in intra group comparison in high myopia; 

Dry eye symptoms were also assessed by OSDI scores which showed a significant rise at one week and four weeks as compared to the baseline with a fall at three months, resulting in comparable values to the baseline. Amongst the two groups, there was no difference in the OSDI score trends (p>0.05) (Figure 4).
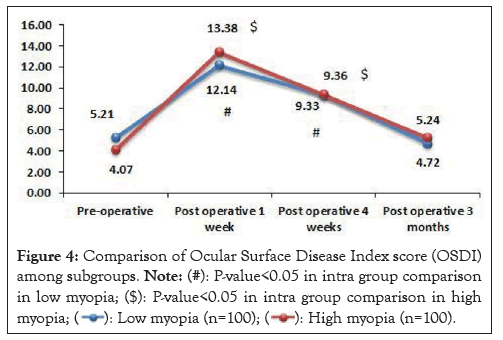
Figure 4: Comparison of Ocular Surface Disease Index score (OSDI)
among subgroups. Note: (#): P-value<0.05 in intra group comparison
in low myopia; ($): P-value<0.05 in intra group comparison in high myopia; 
No correlation between postoperative dry eyes and intraoperative optic zone was noted. Similarly, this study could not find any correlation with contact lens usage before surgery and postoperative recovery.
SMILE surgery is a conscious choice and not a necessary treatment for a refractive error like myopia, so a person who chooses the costly procedure, analyses all possible pros and cons of the intervention and all other treatment options available, like FS-LASIK and conventional Laser-Assisted In-situ Keratomileusis (LASIK) to choose the best suitable option.
Here comes the importance of reliable result outcome data from previous studies on different procedures, which is the only objective way to answer their queries and relieve them from procedure-related anxiety.
Previous studies, clearly show decreased corneal sensation and dry eye symptoms after refractive surgeries, the relevant question that needs to be answered is; how fast and complete the recovery is in different treatment options. So, we took up this study to keenly document post-procedure, chronological outcomes concerning dry eye symptoms and recovery quality [16-19].
The recovery rate after refractive surgeries depends on the severity of abrasion to anterior corneal nerves done while flapping creation. As compared to LASIK, SMILE involves a shorter circumferential corneal cut, maintaining corneal integrity, so less nerve damage (corneal sub-basal and stromal) with this flapless procedure results in much lower flap-related.
Complication rates and early recovery. Here in this study, we observed correction of CDVA in 100% cases after three months with all patients achieving 6/5 or 6/6 vision in both low and high myopes (no patient required spectacles).
As far as the dry eye symptoms post-surgery are concerned, SMILE surgery showed recovery of dry eye symptoms within 3 months of surgery. Though there was an initial increase in the dry eye symptoms (up to one week), it showed early recovery in the further follow-up.
The low cost and simplicity of the Schirmer test make it the most commonly used screening test for the assessment of tear production. As for Schirmer's test Qiu, et al., [13] observed that the values decreased at week one after surgery (all P<0.01, by t-test) among the myopes undergoing SMILE surgery which returned to the baseline values at four weeks and 3rd month after surgery (P=0.62, 0.89, respectively, by t-test). In another study by Denoyer, et al., [16] 30 subjects with spherical correction range, -1 to -8 diopters; cylinder range, 0 to -1.5 diopters scheduled for bilateral SMILE were included where Schirmer test values at 1 and 6 months after refractive surgery were found to be 13.2 mm/5 min and 17.3 mm/5 min, respectively. There was a decrease in values of Schirmer score at six months after surgery compared to one month. Similarly, Ganesh, et al., [17] evaluated 50 eyes (25 patients) who underwent SMILE for correction of myopia, myopic astigmatism and found that Schirmer I and II test decreased in the immediate postoperative period.
This trend has been observed in both LASIK and SMILE surgery as shown in the study by Li, et al., [18] (71 patients underwent SMILE or Femto-LASIK procedures for the treatment of myopia) who reported a significant decrease in the Schirmer test at postoperative one month (P=0.04) with an increase at three months (14.14) and six months (16.28) to reach comparable values with the baseline (14.63).
Tear quality changes and ocular surface damage often lead to a reduction in TBUT and increased corneal staining. Similar to the objective results and trends of Schirmer’s test, TBUT values fluctuated similarly but to a greater extent and failed to reach up to the baseline values. Similar in line with the present study, Qiu, et al., [13] observed that TBUT was significantly decreased at all postoperative time points (day one, week one, one month and 3rd month) compared with preoperative values (P<0.01).
In a study by Xia, et al., [19] (showing table also in link) (78 eyes) mean TBUT values at one month, three months, six months, one year, two years and three years were 8.56, 9.59, 10.01, 10.22, 10.38 and 10.44, respectively with TBUT returning comparable to the preoperative values at the third month postoperatively which was in slight contrast to the current study. Even Ganesh, et al., [17] reported that after SMILE, TBUT improved at 3 months post operatively compared to postoperative day 15.
With respect to the time of follow up, some studies followed the patients for a longer period of time and thus were able to exactly know the exact interval at which the TBUT was comparable to the normal preoperative values beyond three months. Denoyer, et al., [16] and Li, et al., [18] reported that TBUT normalized within six months. Though in our study, the post-operative values did not return to normal preoperative values, this can be due to the shorter time of follow up in the study.
The initial increase in dry eye symptoms as observed objectively in our study with lower Schirmer’s and TBUT may be due to immediate ceasing of corneal nerve sensations caused by laser ablation. Procedure affected corneal area shows signs and symptoms of mechanical damage like keratocytes, corneal epithelium, subbasal, stroma and nerve disruption and biochemical damage that is decreased secretion of Nerve Growth Factor (NGF) in tears.
In SMILE, the recovery is faster may be because of lesser mechanical and biochemical damage resulting in early restoration of keratocytes density and secretions. Early restored secretions like NGF, in turn further induces keratocytes migration, increasing their density and enhances healing. Studies have shown that concentrations of pro-inflammatory markers like cytokine interleukin-6 in tears may also promote cornea healing.
In conditions, where air pollution, heat and weather conditions are harsh, we need to inform patient to take specific, strict precautions in the follow up for a better recovery. Counselling and explaining the patient importance of post procedure care holds significance as complete recovery can take upto 12 weeks. Any breach of the precautions can cause permanent damage, impacting the procedure success adversely.
It can be concluded that SMILE is a feasible procedure for treatment of myopia which requires a period of around three months for adaptation and normalization of the tear film and corneal sensitivity after the surgery. The comparison of the results among the low and high myopes showed a similar trend of improvement, thereby showing the effectiveness of SMILE for low to high myopes. There was no control group of other refractive surgery procedure, so we could not compare dry eye symptoms and recovery chronographically between two procedures.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Yadav Y, Sharma VK, Gupta R, Singh PK, Mohapatra T, Kumar S (2024) Changes in Ocular Surface Indices in Myopia Patients Undergoing Small Incision Lenticule Extraction (SMILE) Surgery. J Clin Exp Ophthalmol. 15:974.
Received: 26-Feb-2024, Manuscript No. JCEO-24-30190; Editor assigned: 28-Feb-2024, Pre QC No. JCEO-24-30190 (PQ); Reviewed: 13-Mar-2024, QC No. JCEO-24-30190; Revised: 20-Mar-2024, Manuscript No. JCEO-24-30190 (R); Published: 28-Mar-2024 , DOI: 10.35248/2155-9570.24.15.974
Copyright: © 2024 Yadav Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.