Poultry, Fisheries & Wildlife Sciences
Open Access
ISSN: 2375-446X
ISSN: 2375-446X
Research Article - (2019)Volume 7, Issue 2
Anthrax (Bacillus anthracis) is a zoonotic disease endemic to environments worldwide. Spores, the dormant form of the bacteria, can survive for decades in nature’s harshest environments and maintain their viability to cause disease. Outbreaks are common in free-ranging livestock and wildlife, thus making anthrax an economically and ecologically important disease. The currently available vaccine to protect livestock is a suspension of B. anthracis Sterne Strain 34F2 spores in saponin (Sterne vaccine). However, it is only available as a subcutaneous injection which is an impractical method of prevention for wildlife. Oral vaccination is the ideal method for free-ranging wildlife, but the Sterne vaccine has never been thoroughly evaluated for oral administration. The current study evaluated the antibody titers induced in mice by subcutaneous or oral vaccination with three different doses of the Sterne vaccine. Results described here show a gradual increase in antibody titers at each time point following subcutaneous vaccination with all vaccine doses. In contrast, no antibody response was detected from any dose or any time point after oral vaccination. Taken together, these results suggest that the Sterne vaccine is only effective as a subcutaneous injection and that an alternate oral anthrax vaccine formulation must be developed to allow for efficient vaccination of free-ranging livestock and wildlife.
Anthrax; Antibody; Oral; Sterne strain; Subcutaneous; Vaccine; Wildlife
Anthrax is an ancient, zoonotic disease caused by the spore forming bacterium, Bacillus anthracis. It gained public attention as a potential bioweapon because in its dormant spore form it is uniquely suited to survive for decades in nature’s harshest environments but the importance of anthrax as a zoonosis has been undervalued [1,2]. Since its first documented outbreak over three millennia ago, anthrax has utilized livestock and human hosts to spread all over the world while proving itself to be an economically important disease by causing large scale mortalities, with one outbreak resulting in the deaths of up to 60,000 animals [3]. Luckily, the discovery of the pXO2 negative strain in 1937 resulted in the live attenuated, noncapsulated strain, B. anthracis Sterne strain 34F2 (Sterne spores) [4]. Shortly thereafter, the Sterne vaccine was developed by suspending Sterne spores in saponin and routine parenteral vaccination of domesticated livestock with the Sterne vaccine ever since has prevented additional livestock mortalities of this scale [5].
Unfortunately, the same cannot be said for free-ranging wildlife where large outbreaks still occur. In the last 82 years since the Sterne strain was discovered, national parks and wildlife reserves have become more popular, more widespread and more valuable to locals and tourists worldwide [6,7]; however, anthrax prevalence is undetermined in these areas so it is probable that additional smaller outbreaks occur more frequently without proper documentation [8]. For example, specifically in the United States, the Edwards Plateau region of Texas spans more than 1.5 million acres and experiences yearly outbreaks that can be exacerbated by cool, wet weather followed by hot, dry conditions [9]. This same region of Texas also happens to include upwards of 68% of the state’s nearly 500 exotic animal reserves that are important economic and conservation resources, according to a 1992 report by Texas Parks and Wildlife Department [10]. While environmental conditions may help predict anthrax epizootics, the predictability isn’t beneficial if the only method of anthrax prevention is to individually inject thousands of animals ranging freely over thousands of acres [11].
The resilience of the anthrax spore ensures that there will always be sporadic large-scale outbreaks in wildlife along with more common small-scale losses, and currently management options are limited. While surrounding livestock can be quarantined and vaccinated by subcutaneous injection with the commercially available formulations of the Sterne vaccine, this is impossible with free-ranging wildlife. Also, animal carcasses need proper disposal to prevent further spread of infection [12]. The best method of disposal is incineration on site but this requires a great amount of fuel, is expensive and time consuming, and may not be tolerated when the risk for wildfire is high, as it often is when outbreaks occur [13]. The inability to vaccinate animals coupled with poor outbreak management and documentation practices can result in spore-laden carcass piles that further exacerbate the risk of infection (Figure 1).
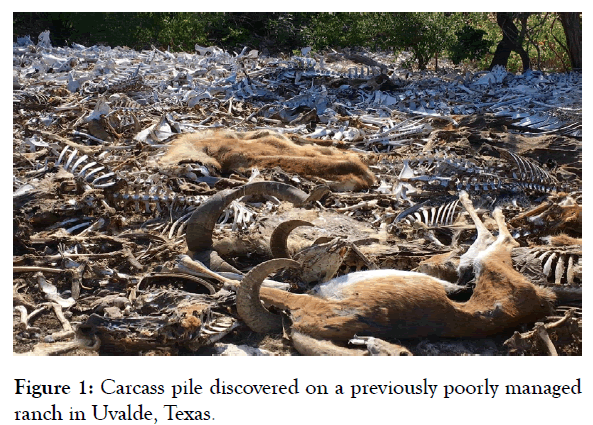
Figure 1: Carcass pile discovered on a previously poorly managed ranch in Uvalde, Texas.
Ranch is now under new management and carcass pile has been disposed of properly. Photo courtesy of G. Staack.
The most common method of anthrax prevention is to prophylactically administer wildlife feed laced an antibiotic, such as chlortetracycline [8]. The long-term effectiveness of this strategy is unconfirmed, and investigations suggest it is significantly less effective than adequately timed vaccination [13,14]. Furthermore, this practice is illegal and recently under more scrutiny with implementation of the Veterinary Feed Directive which prohibits the off-label use of antibiotics in feed [15]. In an effort to protect their herds from inevitable anthrax outbreaks, there are anecdotal accounts of wildlife and ranch managers resorting to pouring the commercial vaccine over feed with no solid scientific evidence to suggest it is truly an effective vaccination strategy (Davis 2019, personal communication), therefore the present study was designed to compare the immunogenicity of the Sterne vaccine at three doses following subcutaneous and oral vaccination.
Mice
A total of 64, four- to six-week-old female BALBc/J mice were purchased from The Jackson Laboratory (Bar Harbor, ME, USA). Upon arrival at the animal facility, mice were randomly distributed into eight groups (Table 1) and allowed to acclimate for at least a week prior to any manipulation. All animal care and experimental procedures were performed in compliance with the Texas A&M University Institutional Animal Care and Use Committee regulations.
Table 1: Vaccination groups used to evaluate the Sterne vaccine in BALBc/J mice.
Route |
Group (n=8) | Inoculation Volume | Spores/ml | Spores/Mouse | Blood Collection (days post-vaccination) |
|---|---|---|---|---|---|
| SC | Control | 0.2 ml | PBS | - | 0, 3, 8, 15, 22, 31, 43, 55 |
| Sterne Dose 1 | 0.2 ml | 5x104 | 1x104 | 0, 3, 8, 15, 22, 31, 43, 55 | |
| Sterne Dose 2 | 0.2 ml | 5x106 | 1x106 | 0, 3, 8, 15, 22, 31, 43, 55 | |
| Sterne Dose 3 | 0.2 ml | 5x108 | 1x108 | 0, 3, 8, 15, 22, 31, 43, 55 | |
| Oral | Control | 0.2 ml | PBS | - | 0, 3, 8, 15, 22, 31, 43, 55 |
| Sterne Dose 1 | 0.2 ml | 5x104 | 1x104 | 0, 3, 8, 15, 22, 31, 43, 55 | |
| Sterne Dose 2 | 0.2 ml | 5x106 | 1x106 | 0, 3, 8, 15, 22, 31, 43, 55 | |
| Sterne Dose 3 | 0.2 ml | 5x108 | 1x108 | 0, 3, 8, 15, 22, 31, 43, 55 |
Bacterial strains
All bacteria used in this experiment were live attenuated B. anthracis Sterne strain 34F2 spores (Sterne spores) that were cultured from a new vial of the Anthrax Spore Vaccine (ASV) from Colorado Serum Company (Denver, CO, USA), the commercial producer of the Sterne vaccine in North America. Sterne spores were prepared by inoculating 5 ml of LB broth with 200 μl of the ASV and cultured overnight at 37°C with shaking. The overnight growth was collected by centrifugation at 3800 rpm, resuspended in 1 ml of fresh LB broth, plated onto LB agar (100 μl per plate) and incubated at 37°C for 6 days to sporulate. Sterne spores were harvested from the plates and washed repeatedly with 25 ml of sterile water. The harvested Sterne spores were further purified by heating at 68°C for 1 hour and filtering through a 3.1 μm filter to kill and remove any remaining vegetative cells (Figure 2).
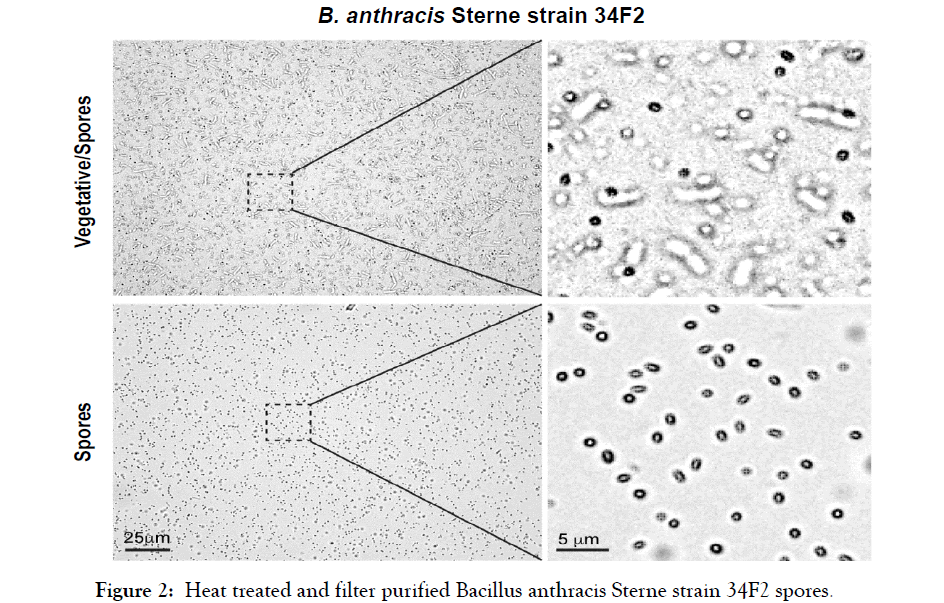
Figure 2: Heat treated and filter purified Bacillus anthracis Sterne strain 34F2 spores.
Representative bright field images in the top panel show a mixture of vegetative and sporulated B. anthracis Sterne strain 34F2. Images in the bottom panel show pure spores devoid of vegetative bacteria obtained after heating at 68°C and filtering through a 3.1 μm filter. The magnified images in the right panel correspond to the segmented square selections in the left panel.
Final Sterne spore concentrations were determined by serial dilutions and plating on LB agar and then final spore stocks were stored in sterile water.
Vaccine Preparation
The ASV is commercially distributed for use in cattle, sheep, goats, swine and horses with a recommended 1 ml dose of between 4 × 106 and 6 × 106 viable Sterne spores in saponin (Berrier 2016, personal communication). This experiment investigated the dose response to subcutaneous or oral vaccination with three doses of Sterne spores in saponin. The lowest dose was 5 × 104 spores/ ml, the middle dose was 5 × 106 spores/ml and the highest dose was 5 × 108 spores/ml. For the purposes of this experiment, the dose of the ASV was assumed to be 5 × 106 spores/ml and was used as the middle dose exactly as it was received from Colorado Serum Company. The lower and higher doses were made as similar as possible to the commercialized product to ensure that any variation in response was solely due to the different bacterial doses. Additional bottles of the ASV were centrifuged and filtered to remove all Sterne spores from the ASV, resulting in pure, commercial quality saponin. The purified saponin was plated on LB agar to confirm all commercial Sterne spores had been removed, and then it was used to resuspend lab-prepared Sterne spores at the target concentrations of 5 × 104 and 5 × 108 spores/ml.
Vaccination
Mice (n=8) were vaccinated subcutaneously or by oral gavage with 0.2 ml of sterile PBS or one of the following Sterne vaccine doses: 5 × 104 spores/ml, 5 × 106 spores/ml or 5 × 108 spores/ml (Table 1). Antibody responses were evaluated in blood samples that were collected three to seven days prior to vaccination, three to five days after vaccination and then every seven to ten days for eight weeks.
Detection of anthrax-specific antibody levels
Serum was isolated from collected blood samples and analyzed by ELISA to quantify the anthrax-specific IgG levels induced by each vaccine dose following subcutaneous or oral vaccination. Corning 96-well EIA/RIA high binding plates (Corning Inc., Corning, NY, USA) were coated with 100 ng per well of Anthrax Protective Antigen (List Biological Laboratories Inc., Campbell, CA, USA) in carbonate bicarbonate buffer, pH 9.6. Plates were incubated at 37°C for one hour, then overnight at 4°C and used within four days. All plates were washed three times with phosphate buffered saline containing 0.5% Tween 20 (PBST) and then blocked for one hour at 37°C with 100 μl per well of 1% Bovine Serum Albumin (w/v) in PBST (1% BSA). After blocking, plates were washed and incubated with 100 μl per well of diluted serum at 37°C for one hour. Serum samples were diluted in 1% BSA at 1:3,000 for subcutaneously immunized mice and 1:500 for orally immunized mice. Plates were washed with PBST, then incubated at 37°C for one hour with 100 μl per well of Anti-Mouse IgG (H+L) Antibody (SeraCare, Milford, MA, USA) diluted 1:5000 in 1% BSA according to the supplier’s recommendations. Plates were washed five times with PBST prior to application of 100 μl of TMB/E Substrate (Sigma-Aldrich, St. Louis, MO, USA). The reaction was stopped after 15 minutes by adding 100 μl of 0.5 M H2SO4. Optical density of each well was read at 450 nm using a Tecan Infinite F50 Plate Reader. Samples from each mouse, at each time point were run in duplicate. Absorbance values are reported as the average value for all duplicates in the vaccination group. Statistical analysis was performed using ANOVA followed by the Tukey-Kramer HSD test with p-values <0.05 considered significant (JMP Pro 14, Cary, NC, USA).
Anti-anthrax antibody response
The anti-anthrax specific antibody titers in response to subcutaneous or oral vaccination with three doses of the Sterne vaccine were measured by ELISA. The mean absorbance values for each subcutaneous vaccination group are illustrated in Figure 3.
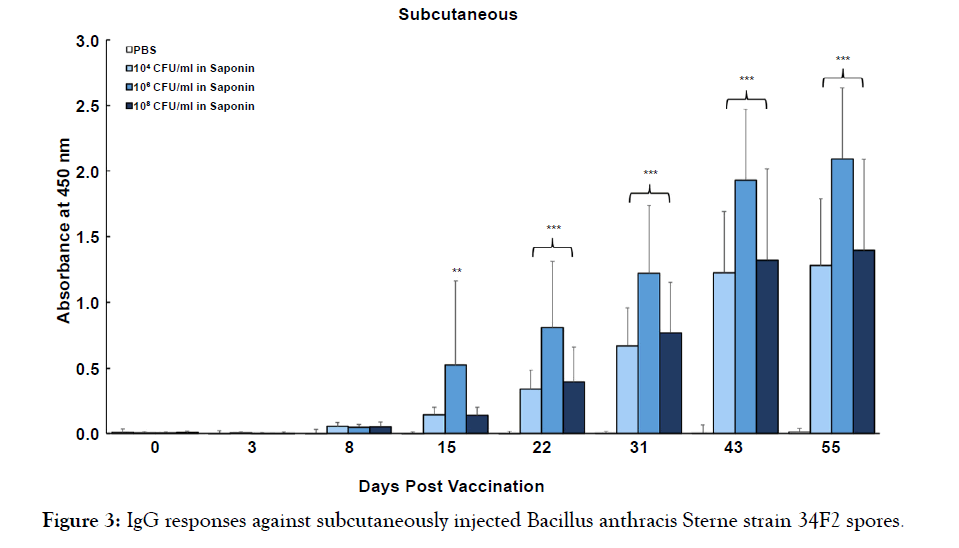
Figure 3: IgG responses against subcutaneously injected Bacillus anthracis Sterne strain 34F2 spores.
BALBc/J mice were inoculated with 0.2 ml of 5 × 104 spores/ml, 5 × 106 spores/ml or 5 × 108 spores/ml of B. anthracis Sterne strain 34F2 spores in saponin. Control mice received 0.2 ml of sterile PBS. Blood samples were collected three to seven days prior to vaccination, three to five days after vaccination and then every seven to ten days for eight weeks. Serum was isolated from all blood samples and the antibody titer was determined by ELISA at a dilution of 1:3,000. Results are shown as average absorbance values + the standard deviations at 450 nm (**p<0.01 and ***p<0.001)
All three vaccine doses stimulated a gradual increase in antibody levels with each time point and all measured antibody levels for the 5 × 104 spores/ml and 5 × 108 spores/ml groups are significantly different from control starting at 22 days post vaccination (p<0.001). A clear dose response can be observed when comparing the 5 × 104 spores/ml group with the 5 × 106 spores/ml and the 5 × 108 spores/ml groups separately. The 5 × 106 spores/ml group resulted in a faster antibody response that was significantly different from control starting at 15 days post vaccination, seven days earlier than the response from both the 5 × 104 spores/ml and the 5 × 108 spores/ml groups (p<0.01). The 5 × 106 spores/ml group also had significantly higher antibody titers than the 5 × 108 spores/ml group starting at 15 days post vaccination (p<0.01). In contrast, ELISA results from the oral vaccination groups did not reveal any antibody response following oral vaccination with any dose of the Sterne vaccine, despite using a dilution that was four times more concentrated than the subcutaneous serum (Figure 4).
BALBc/J mice were inoculated with 0.2 ml of 5 × 104 spores/ml, 5 × 106 spores/ml or 5 × 108 spores/ml of B. anthracis Sterne stable>train 34F2 spores in saponin. Control mice received 0.2 ml of sterile PBS. Blood samples were collected three to seven days prior to vaccination, three to five days after vaccination and then every seven to ten days for eight weeks. Serum was isolated from all blood samples and the antibody titer was determined by ELISA at a dilution of 1:500. Results are shown as average absorbance values + the standard deviations at 450 nm.
For over 80 years, the Sterne vaccine formulation of live attenuated B. anthracis Sterne strain 34F2 spores in saponin has been manufactured and distributed worldwide as a subcutaneous livestock vaccine. Results presented here confirm its ability to stimulate anthrax specific antibody production after subcutaneous injection with three different doses (Figure 3). Antibody titers from each of the three vaccine doses showed gradual increases over time as expected. Interestingly, the middle dose, 5 × 106 spores/ ml in saponin, induced a faster antibody response by seven days and a stronger antibody response when compared to the higher dose, 5 × 108 spores/ml in saponin. Normally a 100-fold increase in inoculated spores would be expected to induce the stronger antibody response, however the inoculant for the middle dose was used directly from a new ASV vial whereas the spores for the higher dose were prepared by culturing them out of an ASV vial. This discrepancy can likely be attributed to reduced immunogenicity on subculture of non-capsulated B. anthracis strains, such as the Sterne strain [5,12].
As evidenced by the antibody titers observed from the subcutaneously vaccinated mice, as well as decades of vaccination history, parenteral inoculation with Sterne spores can protect an animal from anthrax, however the Sterne vaccine has never been thoroughly evaluated as an oral vaccine [12,16,17]. Thus, the current study compared the antibody response of subcutaneously inoculated versus orally administered Sterne spores in mice. In contrast to the robust immune responses induced by the subcutaneous injections, no antibody response was detected in mice following oral administration in this study (Figure 4).Even inoculating mice with a lower or higher dose of Sterne spores failed to induce any antibody titer. A previous experiment with goats found a similar pattern when comparing subcutaneous injections and oral inoculation with Sterne spores mixed with scarifying agents. Upon secondary exposure to Sterne spores by subcutaneous injection, an antibody response was observed in the goats that were previously vaccinated orally [18] but it is likely this secondary response was due solely to the method of subcutaneous challenge.
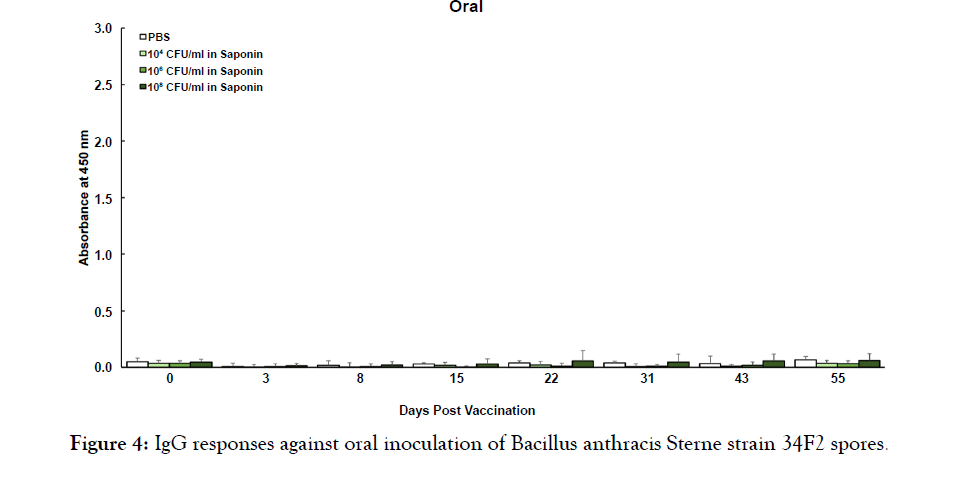
Figure 4: IgG responses against oral inoculation of Bacillus anthracis Sterne strain 34F2 spores.
All-encompassing data for anthrax infections in wildlife is essentially non-existent, but it is believed that anthrax is capable of affecting all mammals with varying degrees of morbidity and mortality (8). Infections have been reported in over 50 African wildlife species, including threatened and endangered species such as the black rhinoceros, African elephant, cheetah and wild dog, with dozens more known to be susceptible [8,19-22]. In North America, anthrax has been documented in white-tailed deer, elk, bison, bears, and other native and exotic species [23,25]. Inconvenient outbreaks in wildlife cause economic, ecological and conservational burdens worldwide [3,26]. Despite the availability of a safe and effective animal vaccine, a recently proposed model for the global distribution and suitability of anthrax found that most livestock and wildlife at risk of exposure are not vaccinated [26]. This may be due to the fact that most commercial animal vaccines use the same formulation developed by Max Sterne in 1939 which is outdated, can cause adverse reactions, requires yearly boosters and requires refrigerated storage [27,28]. The most prominent reason, however, is because the existing method of subcutaneous injection with the Sterne vaccine is not a feasible method of vaccination for free-ranging livestock and wildlife, so many anthrax vaccine reviews have called for a new anthrax vaccine, specifically an oral anthrax vaccine [8,12,27]. Sharing in that opinion are ranch managers in the Edwards Plateau region of Texas who cannot practically vaccinate all of their animals by injection, so some have improvised by pouring the Sterne vaccine over feed, even doing so every other week for the entire spring before the typical anthrax season by one account. While this specific narrative claims that this tedious vaccination strategy appeared to be effective (Davis 2019, personal communication), the results of the current study suggest it may have been circumstantial. Desperate attempts such as these to protect their herds, coupled with the absence of antibody titer following oral inoculation in this study, further emphasize the urgent need for an anthrax vaccine specifically formulated for oral use in wildlife [29-31].
In the time since the Sterne vaccine was discovered, the human population has nearly tripled and interactions with wildlife have drastically changed. Humans, domesticated livestock and wildlife have become more interconnected thus increasing the economic and intrinsic value of wildlife and overall wildlife health. Sensitive wildlife conservation efforts are in a constant state of worry because they frequently involve unvaccinated animals on anthrax prone landscapes. Furthermore, the success of wild animal reserves in these same areas can be limited by anthrax outbreaks since nonexistent vaccination policies are known to affect the epidemiology and rate of transmission to humans. Given the unsatisfactory performance of the orally administered Sterne vaccine in this study, future research efforts must focus their attention on developing a safe and effective oral anthrax vaccination protocol for use in wildlife as it will be the key to preventing anthrax epidemics in wildlife, as well as maintaining public and global wildlife health.
The authors thank Dr. Randall Berrier at Colorado Serum Company for generously providing multiple bottles of the Anthrax Spore Vaccine for use in this study. We would also like to thank Mr. Glenn Staack for sharing the photo in this article. This work was supported by a faculty start-up grant from Texas A&M University to W.C. as well as a Graduate Student Research Trainee Grant awarded to J.B.F. by Texas A&M University College of Veterinary Medicine and Biomedical Sciences.
Citation: Felix JB, Chaki SP, Ficht TA, Rice-Ficht AC, Cook W. (2019) Bacillus anthracis Sterne Strain 34f2 Vaccine Antibody Dose Response by Subcutaneous and Oral Administration. Poult Fish Wildl Sci 7:206. doi: 10.35248/2375-446X.19.7.206
Received: 19-Sep-2019 Accepted: 11-Oct-2019 Published: 17-Oct-2019 , DOI: 10.35248/2375-446X.19.7.206
Copyright: Copyright: © 2019 Felix JB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : This work was supported by a faculty start-up grant from Texas A&M University to W.C. as well as a Graduate Student Research Trainee Grant awarded to J.B.F. by Texas A&M University College of Veterinary Medicine and Biomedical Sciences.