
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2020)Volume 10, Issue 1
Background: Any treatment for unknown infertility is empiric by default, and the broad range of treatment, including expectant management, superovulation, IUI, IVF and IVF–intracytoplasmic sperm injection, reflects the uncertainty with this diagnosis. There are limited data to support the efficacy of many of these treatments, and no uniform protocol exists in clinical practice. Autologous platelet rich plasma (A-PRP) can be a novel technique which has never been explored before much in this field.
Objective: To compare autologous platelet rich plasma with expectant management in cases of unexplained infertility.
Materials and methods: All cases (50) of primary unexplained infertility were treated with either A-PRP or by expectant management on the basis of their endometrial thickness (7 mm). All cases of thin endometrium (<7 mm) were subjected to A-PRP (25 cases). Whereas rest of the cases (25 in number) was monitored as per expectant management protocol for a maximum of three cycles after which they were switched over to being treated with PRP. The main outcomes measured were number of follicles, endometrial thickness, pregnancy rate and miscarriage rates. The statistical analysis was evaluated with IBM SPSS Statistics for Windows, Version 24.0, IBM Corp, and Chicago, IL.
Results: Out of 46 patients, 25 patients (54.35%) got conceived with a single dose of intra-uterine autologous platelet rich plasma injection, which was found to be statistically highly significant. The correlation analysis with Spearman’s Rank correlation coefficient (rho ρ) was 0.891 which show highly positive correlation between intrauterine autologous platelet rich plasma injection and pregnancy rate and 0.247 which show weakly positive correlation between expectant management and pregnancy rate.
Conclusion: Autologous platelet rich plasma (A-PRP) is a novel technique than can treat unexplained infertility with favorable outcomes.
Unexplained infertility; Platelet rich plasma; Alpha granules; Expectant management
Unexplained or idiopathic infertility, constituting 30% of infertile couples worldwide, is defined as the lack of an obvious cause for a couple's infertility and the females’ inability to get pregnant after at least 12 cycles of unprotected intercourse or after six cycles in women above 35 years of age for whom all the standard evaluations are normal [1]. Any treatment for unknown infertility is empiric by default, and the broad range of treatment, including expectant management, superovulation, IUI, IVF and IVF–intracytoplasmic sperm injection, reflects the uncertainty with this diagnosis. Several key variables including age, infertility history, treatment history, costs, and risks should be considered in selection of the suitable treatment plan. However, there are limited data to support the efficacy of many of these treatments, and no uniform protocol exists in clinical practice [2,3].
The rate of spontaneous conception in these couples is more than the couples with defined causes of infertility and several studies have reported that the rate of spontaneous pregnancy was 13-15% during the first year of attempt which increased to 35% during the next two years. Moreover, the rate could reach 80% in younger couples during the following three years of unprotected intercourse without any adjuvant therapy. Thus, the best plan for them would be expectant management [1,4,5].
Factors including lack of strong clinical evidence, couple ’ s impatience for completion of standard protocols and dominance of ART treatment compared to other options lead to diversity of clinical practice regarding unexplained infertility. Often the clinicians offer additional expensive and experimental tests which waste the golden time of couples for pregnancy without any effective results.
Extensive research in reproductive biology and increasing our knowledge of gametogenesis, fertilization, embryo development, and endometrium-implantation and fetus-uterus crosstalk can provide more effective treatment options in future for infertile couples specially the ones with unexplained infertility.
Autologous platelet rich plasma (A-PRP) can also be referred as Regenerative Concentrate of Active Plasma (R-CAP), which is defined as the volume of plasma with an exponentially increased platelet concentration of 5-6 times above the baseline (106- 107/mL). Platelet contains alpha granules which provides various growth factors which stimulates biological healing, homeostasis and tissue rejuvenation by a supra-physiological release of biological micro molecules at the site of the injection [6]. It, being injected in the uterine cavity and its effects on endometrial receptivity, has been an upcoming topic of research dealt very little in the field of reproductive medicine [7,8] Hence, the need for this study.
To compare the autologous platelet rich plasma (A-PRP) with the expectant management in cases of unexplained infertility.
With level IV evidence, a prospective cohort study was performed from July 2017 to June 2019 in the department of Obstetrics and Gynaecology, JJM Medical College, Davangere, Karnataka, India. The patients for this study were recruited by convenient sampling technique. A total of 50 cases of primary unexplained infertility were taken who satisfied the inclusion and exclusion criteria of the study.
All cases of primary unexplained infertility, women in reproductive age (18-40 years) with normal ovulatory function and regular menstrual cycles, patients with bilateral fallopian tubes patent observed at laparoscopic chromopertubation, or hysterosalphingography or sonosalphingography and their spouse having male factor fertility confirmed by adequate seminal parameters according to latest WHO guidelines were included in the study. Patients with secondary infertility, irregular menstrual cycles, tubal blockage identified by above mentioned techniques, clinical evidence of hyperprolactinemia, hypercortisolism, or thyroid dysfunction, male infertility and patients who refused participation as per our protocol were excluded from the study.
After getting IEC clearance from the institute and informed written consent from the patients enrolled in our study, they were subjected for thorough examination for confirmation of diagnosis of unexplained infertility. Transvaginal ultrasound for endometrial thickness was done on day 14 - 16 of the cycle. Women with thin endometrium (<7 mm endometrial thickness) were included in the A-PRP group. Whereas, other participants were subjected to expectant management.
A-PRP group (Group A): An amount of 10 cm3 of the patient’s blood was drawn in a syringe containing sodium citrate anticoagulant. A-PRP was obtained using differential centrifugation (soft spin of 200 × g for 15 min followed by hard spin of 600 × g for 6 min). A volume of 1.0 to 1.5 ml of the A-PRP was thus obtained. It was infused intrauterine at the junction of endometrium and myometrium in a single sitting from 3-7th day of menstrual cycle using an IUI canula under ultrasound guidance following all aseptic precautions. This was followed by advice on timed intercourse (Figures 1 and 2).
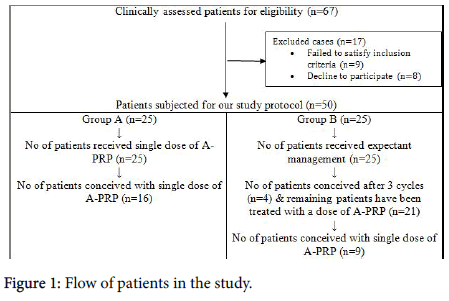
Figure 1. Flow of patients in the study.
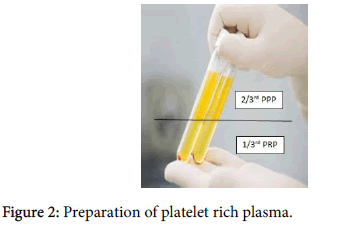
Figure 2. Preparation of platelet rich plasma.
Expectant management group (Group B): Couples were advised to be sexually active around the likely time of ovulation and provided with a diary to record the first day of each menstrual cycle and dates of sexual activity. Maximum of three cycles were tried, after which failed cases were transferred for A-PRP treatment.
The main outcomes measured were number of follicles, endometrial thickness, pregnancy rate and miscarriage rates. The statistical analysis was evaluated with IBM SPSS Statistics for Windows, Version 24.0, IBM Corp, Chicago, IL. Spearman’s Rank correlation coefficient (rho ρ) was used to correlate the pregnancy rate and the management used as per the study protocol (Figures 3 and 4).
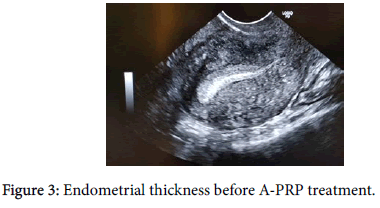
Figure 3. Endometrial thickness before A-PRP treatment.
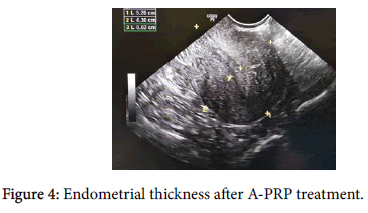
Figure 4. Endometrial thickness after A-PRP treatment.
After excluding 17 patients, a total of 50 patients entered our study and were treated with intrauterine autologous platelet rich plasma injection for group A patients and expectant management for group B patients as per our protocol as shown in the Tables 1 and 2 and Figures 5 and 6.
| Parameters | Group A | Group B | p value |
|---|---|---|---|
| Age (years) | 26.10 ± 3.39 | 27.55 ± 6.65 | 1.963 |
| No of years of infertility (years) | 2.19 ± 0.71 | 1.96 ± 0.99 | 0.709 |
| BMI (kg/m2) | 24.51 ± 3.62 | 25.41 ± 4.81 | 0.612 |
Table 1: Patient’s demography.
| Parameters | Before A-PRP treatment | After A-PRP treatment | p value |
|---|---|---|---|
| Average number of follicles | 3 | 11 | 0.001 |
| Endometrial thickness (mm) | 5 | 9.7 | 0.05 |
| Pregnancy rate | 0 | 25 | <0.0001 |
Table 2: Outcome parameters of A-PRP treatment in study population (n=46) (Group A n=25 and Group B n=21).
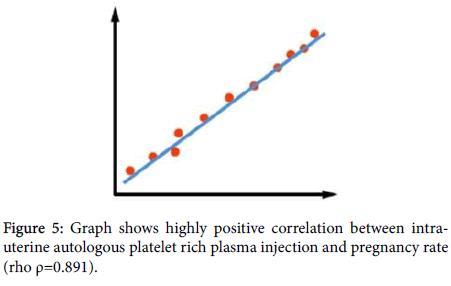
Figure 5. Graph shows highly positive correlation between intrauterine autologous platelet rich plasma injection and pregnancy rate (rho ρ=0.891).
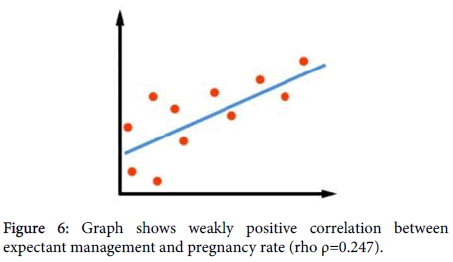
Figure 6. Graph shows weakly positive correlation between expectant management and pregnancy rate (rho ρ=0.247).
Age, number of years of infertility and BMI in both the study groups were similar. The mean age in group treated with A-PRP was 26.10 ± 3.39 years and in the expectant management group was 27.55 ± 6.65 years. Number of years of infertility in the study participants was in the range of 1.5 to 3 years. The mean in group A was 2.19 ± 0.71 years and in group B was 1.96 ± 0.99 years. All the participants were in the appropriate BMI mean values with 24.51 ± 3.62 kg/m2 in group A and 25.41 ± 4.81 kg/m2 in group B (as shown in Table 1).
After the institution of treatment, there was an increased number of follicles from 3 to 11 which was statistically significant (p=0.001). We observed that there was increased thickness of endometrium treated with autologous platelet rich plasma injection with no miscarriages. These results were statistically significant. Autologous platelet rich plasma has rejuvenated thin endometrium and poor ovarian reserve in patients with unexplained infertility.
A total of 16 (64.00%) patients in group A (n=25) conceived with a single dose of A-PRP while in group B (n=25) 4 (16.00%) patients got conceived with expectant management. The remaining patients (n=21) in group B were subjected for single dose of A-PRP after 3 cycles of expectant management. Out of 21 patients, 9 (42.85%) patients got conceived with single dose of intra-uterine A-PRP injection.
In our study, after excluding 4 (16.00%) patients who got conceived with 3 cycles of expectant management, remaining 46 patients received a single dose of intra-uterine autologous platelet rich plasma injection. Out of 46 patients, 25 patients (54.35%) got conceived with a single dose of intra-uterine autologous platelet rich plasma injection, which was found to be statistically highly significant. No side effects were noted in both the groups during our study interval.
The correlation analysis with Spearman ’ s Rank correlation coefficient (rho ρ) was 0.891 which show highly positive correlation between intra-uterine autologous platelet rich plasma injection and pregnancy rate and 0.247 which show weakly positive correlation between expectant management and pregnancy rate.
In the past researches, unexplained infertility has been better characterized as subfertility and a major proportion of the couples have achieved pregnancy by no intervention at all [1,4,5] Steures et al. [9] showed a blooming 27% ongoing pregnancy rate with expectant management. Expectant management for 2 years is the best choice for good prognosis when the woman’s age is less than 30. This requires the females to be aware of their ovulation time and the best period for unprotected intercourse. The main advantage of expectant management is avoiding multiple gestations with its accompanied obstetric, prenatal complications and postnatal disability.
Our inability to find the causes of couples’ infertility does not mean that there is no cause for the disorder. Extensive research should be conducted on other possible causes of failed conception such as ovarian and testicular dysfunctions, sperm and oocyte quality, fallopian transport defects, endometrial receptivity, implantation failures, and endometriosis.
Autologous platelet rich plasma (A-PRP), referred as Regenerative Concentrate of Active Plasma which is a regenerative growth factors of alpha granules and dense granules derived from the patient’s own platelets, to treat the reproductive health. It facilitates probability of pregnancy in ART/IVF treatments. Regenerative bioactive micro molecules, peptides and cytokines have no side effects, since the process only accelerate and stimulates the natural repair mechanisms of the human body [6,7].
In 2015, a study by Chang et al. [8] evaluated the role of A-PRP in thin endometrium in five patients undergoing frozen embryo transfer cycles. The endometrial thickness (ET) increased after PRP infusion in all the patients and reached >7 mm on the day of progesterone administration. All patients became pregnant. One of them had a missed abortion, whereas the other four had viable intrauterine pregnancies, followed up till the first trimester. In 2016, a review article by Garcia-Velasco et al. showed that autologous PRP was a potential method of improving ET in women with refractory endometrium [10].
In 2017, Tandulwadkar et al. [7] showed in a larger subset of population (68 cases) that both endometrial thickness and vascularity improved with intrauterine instillation of A-PRP. Also, positive β-hCG values were observed in 60.93% after frozen embryo transfer and the clinical pregnancy rate was 45.31%. Zadehmodarres et al. [11] found that endometrial thickness increased at 48 hours after the first PRP application and reached more than 7 mm after the second PRP application in all patients. Embryo transfer was then carried out in all patients. 50% patients became pregnant. Study by Colombo et al. [12] included 8 patients who underwent PRP treatment. The endometrial thickness was found to be satisfactory in 7 cases, positive test for β- hCG was found in 6 women. They concluded that the multiple implantation failures were caused by inefficient expression of adhesion molecules, which could potentially be improved by PRP application.
Our study, further adds to the line of research by showing that post A-PRP treated cases had improved number of ovarian follicles and endometrial thickness and a pregnancy rate of 54.35% in cases of unexplained infertility. Highly positive correlation was found between intra-uterine autologous platelet rich plasma injection and pregnancy rate. It could be explained by the release of cytokines and growth factors, including vascular endothelial growth factor (VEGF), transforming growth factor, platelet-derived growth factor, and epidermal growth factor which can regulate cell migration, attachment, proliferation and differentiation and promote extracellular matrix accumulation. Also, it is one of very first study which shows improvement in ovarian reserve when the method of instillation was far away from the ovary. Previous all studies [13,14] done on ovarian rejuvenation by A-PRP have been done by actively injecting it at the site of these follicle production.
Thus, autologous PRP is a safe, easily available, and inexpensive treatment modality for women with unexplained infertility. However, further research in the form of large scale randomized controlled trials is needed, which would help to strengthen our observations and enable practitioners to use this modality clinically to optimize their success rates.
Small sample size with single centric study.
Dose and place of infiltration of A-PRP has to be figured out.
A long learning curve is needed to identify the biology of A-PRP in unexplained infertility.
A long-term follow-up is required.
Thin endometrium and poor ovarian response could be the possible etiologies behind unexplained infertility. Autologous platelet rich plasma (A-PRP) is a novel technique than can treat unexplained infertility with favourable outcomes. Thus, this breakthrough in reproductive medicine can work miracles in reducing the tiresome burden of infertility globally.
Citation: Garg N (2020) Autologous Platelet Rich Plasma (A-PRP) in Unexplained Infertility: A Revolution in Reproductive Medicine. J Clin Trials 10: 394. doi: 10.35248/2167-0870.20.10.394
Received: 06-Jan-2020 Accepted: 21-Jan-2020 Published: 28-Jan-2020 , DOI: 10.35248/2167-0870.20.10.394
Copyright: © 2020 Garg N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.