Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research - (2022)Volume 13, Issue 1
Purpose: To analyze the demographic, clinical profile, etiology and management of uveitis related choroidal neovascularization seen at a tertiary center.
Method: Retrospective analysis of patients with a diagnosis of inflammatory choroidal neovascularization.
Results: Eleven eyes from 9 patients were included (5 female and 4 male). The mean age at presentation was 41.2 years. Four eyes (36.7%) had infective etiology and seven eyes (63.2%) had non-infective etiology. The most common location of the CNV was subfoveal in 6 eyes (36.7%). All patients were treated with corticosteroids, additional immunosuppressive were given in 4 eyes (34.6%) and anti-VEGF injections in 6 eyes (63%). Overall the visual outcome was favorable for 9 eyes (81.8%).
Conclusion: Inflammatory CNV can be successfully managed and vision can be improved or stabilized with combined approach of anti-VEGF agents and anti-inflammatory therapy. Besides effective eradication of inflammation in uveitis, the ideal therapeutic goal should include timely detection and treatment of inflammatory CNVM, as the ultimate visual outcome would depend on the control of both.
CNV; Anti-VEGF; Corticosteroids; Uveitis
Inflammations represent the third common cause of Choroidal Neovascularization (CNV) after Age Related Macular Degeneration (ARMD) and pathologic myopia [1-3]. They occur as a complication of various uveitis entities such as Multifocal Choroiditis (MFC), Serpiginous Choroiditis (SC), Vogt-Koyanagi- Harada Disease (VKH), Presumed Ocular Histoplasmosis (POHS), Punctate Inner Choroidopathy (PIC) and infectious uveitis. In contrast to CNV associated with ARMD which is type 1(located below RPE), inflammatory CNV is usually type 2 (located beneath the sensory retina, anterior to the RPE). The inflammatory CNV results either directly from an inflammatory-mediated angiogenic stimulus or secondary to degenerative disruption in the Bruch’s membrane-Retinal Pigment Epithelium (RPE) complex or both [4]. The diagnosis of CNV in uveitic conditions is challenging but prompt diagnosis and treatment will avoid rapid and irreversible visual loss. Fundus Fluorescein Angiography (FFA), Indocyanine Angiography (ICG) and Optical Coherence Tomography (OCT) have been used as crucial tool to ensure an accurate and early diagnosis and to monitor disease progression and treatment response. Newer imaging modalities like Optical Coherence Tomography Angiography (OCTA) provides a valuable tool in monitoring the progression of CNV and in conjunction with FA, OCT can help in improved detection of CNV lesions, especially in cases of inconclusive conventional imaging. The management options available include laser photocoagulation, local and systemic corticosteroids, immunomodulators and surgical removal. Treatment with intravitreal anti-Vascular Endothelial Growth Factor (anti-VEGF) injections is now the mainstream in the management. However all the treatment options have their limitations and the treatment guidelines are ambiguous. Although CNV associated with uveitis is rare, visual prognosis is poor if left untreated. The crucial aspect of management of i-CNV is control of the underlying primary uveitic conditions. The purpose of this study was to analyse the clinical profile, etiologies, management and outcomes. To the best of our knowledge, this is first such type of study from central India.
This retrospective study was conducted at a tertiary care center from central India. The medical records of 9 patients between October 2018 and august 2021 were reviewed. Consecutive eyes of patients who either presented with i-CNV secondary to uveitis or developed CNV during follow up were included. CNV related to high myopia, trauma, age related macular degeneration were excluded. All patients had complete ocular and medical history, Best-Corrected Visual Acuity (BCVA), slit-lamp biomicroscopy, Goldmann applanation tonometry and dilated fundoscopy, tailored laboratory test, optical coherence tomography. Fundus fluorescein angiography was done in selected cases whenever needed. Data including age, sex, laterality, SUN criteria [5] based uveitis diagnosis; management and outcome were collected retrospectively and analyzed. Systemic investigations done wherever required and included complete blood count, urine analysis, Mantaux test, QuantiFERON-TB gold test, serum ACE, RPR,TPHA, chest X-rays. HRCT (High Resolution Computed Tomography) of chest was done with high suspicion of tubercular or sarcoidosis etiology. The location of the CNV was defined according to the Macular Photocoagulation (MPS) Study [6] which included subfoveal, juxtafoveal (0-200 μ from center of fovea) or extrafoveal (>2000 μ from center of fovea). Peripapillary CNV were defined as those which were contiguous to the disc or seen within 1 disc diameter of the optic disc margins. Treatment included oral or intravenous corticosteroids, immunosuppressives, and intravitreal anti-VEGF agents or combination of the above mentioned therapies. Oral corticosteroids were advised for all patients showing evidence of disease activity. Systemic immunosuppressive therapy was given in patients with inadequate steroid response or primary disease itself requiring same. ATT was given to those patients who had positive mantoux test, QTB Gold test with ocular features suggestive of tubercular etiology. Intravitreal agents were used as per indication under topical anesthesia. Recurrence of the CNV was defined as an active CNV during the course of follow up after previous complete resolution. The visual acuity and central foveal thickness at time of CNV presentation and at final visit were noted. A gain of two or more lines was considered as improved, drop of two or more lines as worsened and drop or gain of one line as stable. All statistical analyses were performed with R version 4.0.5. A value of p<0.05 was considered to be statistically significant for all analyses.
General 11 eyes of 9 patients were included for analysis in this retrospective study out of which 4 patients were male and 5 patients were female. 7 patients had only one eye affected with CNV (77.7%) and 2 (22.2%) had both eyes affected. From those with unilateral involvement, 4 were on the right side and 3 on the left side. The mean age at initial presentation was 41.22 years (range 25-52 years). i-CNV had a symptomatic presentation in the majority of the affected eyes (72.7%). Most common symptoms were metamorphopsia (36.3%), vision loss (18.1%), and scotoma (18.1%) (Table 1).
| Symptoms | Number of eyes | Percentage of eyes |
|---|---|---|
| Metamorphopsia | 4 | 36.3 |
| Scotoma | 2 | 18.1 |
| Diminished vision | 2 | 18.1 |
| Diagnosed at routine examination | 3 | 27.2 |
Table 1: Presenting symptoms.
Of 11 eyes, 4 eyes had underlying infective etiology and 7 eyes had non-infective etiology. Amongst the 7 eyes with non-infective uveitis, diagnosis was MFC in 1 eye, SC in 2 eyes, VKH in 1 eye, intermediate uveitis in 1 eye, GHPC in 1 eye and SLC in 1 eye. Out of 4 eyes that had underlying infective etiology 3 had tuberculosis and 1 had toxoplasmosis. 8 eyes had i-CNV at the time of presentation and 3 eyes developed CNV during the course of follow up. 9 eyes were noted to have active uveitis at the time of developing i-CNV as detected by presence of vitreous cells, haze, and an active choroiditis on indirect ophthalmoscopy and confirmed by FFA whenever needed. Location of the CNV was subfoveal in 6 eyes, peripapillary in 3 eyes, juxtafoveal in 2 eyes. The mean follow-up time was 9.09 months (range 4-14 months) (Table 2).
| S. No. | Age/Sex | Eye | Etiology | Location | Uveitis activity at presentation |
|---|---|---|---|---|---|
| 1 | 39/M | L | MFC-TB | SF | Active |
| 2 | 47/F | R | SC | JF | Active |
| 3 | 32/F | R | GHPC | SF | Active |
| 4 | 52/M | L | TOXO | SF | Active |
| 5 | 43/F | L | VKH | PP | Active |
| 6 | 39/M | R | MFC-TB | SF | Inactive |
| 7 | 29/F | R | MFC | PP | Active |
| 8 | 50/F | R | IU | JF | Inactive |
| 9 | 33/M | L | SLC | PP | Active |
| 10 | 46/F | R | PU-TB | SF | Active |
| 11 | 35/M | L | SC | SF | Active |
Abbreviations: M:Male; F:Female; L:Left; R: Right; MFC: Multifocal Choroiditis; SC: Serpiginous Choroiditis; GHPC: Geographic Helicoid Peripapillary Choroidopathy; Toxo: Toxoplasmosis; VKH: Vogt Konayagi Harada Syndrome; IU: Intermediate Uveitis; SLC: Serpiginous Like Choroiditis; PU: Posterior Uveitis;
TB: Tuberculosis; SF: Subfoveal; JF: Juxtafoveal; PP: Peripapillary
Table 2: Demographic profile, etiology, location of CNV.
Oral corticosteroids were used for concomitant treatment for 9 eyes and IV-MP followed by oral steroid in 2 eyes. Immunosuppressives (azathioprine and methotrexate) was used in 4 eyes in additions to steroids. ATT was used in all 3 eyes with an underlying tubercular etiology and anti-toxoplasma medication for 1 eye with toxoplasmosis. Additional treatment in form of anti-VEGF was used in 6 eyes. Final anatomical outcome was scarring of CNV in 9 eyes and active CNV in 2 eyes (Table 3). Recurrence of CNV was noted in 2 eyes and was treated with anti-VEGF injections. Visual acuity at the final follow up had improved in 4 eyes, stable in 5 eyes and worsened in 2 eyes. The mean BCVA at the time of development of CNV was 1.06 log MAR and improved to 0.72 at final visit which was statistically insignificant (p value 0.10). The mean CFT at time of CNV was 320 μm and improved to 184 μm at final visit which was also statistically significant (p value 0.003). At final follow up, 10 eyes had inactive uveitis whereas 1 eye had active uveitis. Causes of poor visual outcome included macular scar and cataract.
| S. No. | Steroid therapy | IMT | Additional specific therapy | No. of Anti-VEGF injections | Visual outcome at last follow up | Anatomical outcome at last follow up | Disease activity at lastv follow up | Follow up ( in months) |
|---|---|---|---|---|---|---|---|---|
| 1 | Oral | AZA | ATT | 2 | Stable | Scarred | Quiet | 9 |
| 2 | Oral | 1 | Improved | Scarred | Quiet | 7 | ||
| 3 | Oral | AZA | Worsened | Scarred | Active | 10 | ||
| 4 | Oral | Anti toxo | 1 | Stable | Scarred | Quiet | 5 | |
| 5 | Pulse+Oral | AZA | 2 | Stable | Scarred | Quiet | 14 | |
| 6 | Oral | ATT | Improved | Scarred | Quiet | 11 | ||
| 7 | Oral | 2 | Improved | Scarred | Quiet | 6 | ||
| 8 | Oral | Stable | Scarred | Quiet | 13 | |||
| 9 | Pulse+Oral | MTX | Stable | Scarred | Quiet | 7 | ||
| 10 | Oral | ATT | 1 | Worsened | Active | Quiet | 14 | |
| 11 | Oral | Improved | Scarred | Quiet | 4 |
Note: AZA: Azathioprine; MTX: Methotrexate; ATT: Anti-Tubercular Therapy
Table 3: Treatment strategy.
| Author (year), country | Design, sample size | Mean no. of injections | Mean follow up | Efficacy outcomes |
|---|---|---|---|---|
| Roy et al. (2017); India [20] |
Retrospective; 30 eyes | 2.76; (bevacizumab, ranibizumab) | 17.93 ± 14.28 months | Improvement in visual acuity in 53.3%; stabilization in 26.6% |
| Ganesh et al. (2017); India [21] | Retrospective; 49 eyes | 2.9 | 46.9 months | Visual acuity improvement in 46.9% and stabilization in 28.6% |
| Parodi et al. (2014); Italy [22] | Prospective; 7 eyes | 1 injection in 12 months (bevacizumab) | 12 months | Visual acuity improvement in 52% and stabilization in 57% |
| Mansour et al. (2012); Lebanon [23] | Retrospective; 8 eyes | 1.375 (bevacizumab) | 5 years | Visual acuity improved (median gain of 3.8 lines) |
| Julian et al. (2011); France [24] | Retrospective; 15 eyes | 4.25 (in 12 eyes); 3 eyes received only 1 injection (bevacizumab) | 17.6 months | Visual acuity improved from 0.53 to 0.29 |
| Our study (2021), Central India | Retrospective; 11 eyes | 1.5 (bevacizumab, ranibizumab) | 9 months | Visual acuity improvement in 36.3% and stabilization in 45.4% |
Table 4: Different studies showing efficacy of Anti-VEGF in inflammatory CNVM.
To the best of our knowledge there are very few studies on inflammatory CNV from India and other country (Table 4). This is first kind of such studies from central India. Inflammatory choroidal neovascularization cause an acute and significant visual loss [7,8]. It represents a diagnostic and treatment challenge to uveitis specialist due to the heterogeneity in etiologies, presentations, disease courses and difficulty in differentiating between inflammatory lesions and neovascularization. While most of the studies report sub-foveal location as the commonest, peripapillary CNV were the most commonly noted in D’Souza et al. study (53.3%) [9-11]. Mansour et al. found that amongst 84 eyes, the most common locations for i-CNV was subfoveal and juxtafoveal [12]. However, in our study CNV was mainly subfoveal followed by peripapillary locations. Recently Mehta et al. propose that chronic disc edema in intermediate uveitis predisposes to formation of peripapillary CNV [13]. Due to the lack of randomized trials, there is no consensus on treatment algorithm. The majority of the affected eyes (72.7%) had a symptomatic presentation. Most common symptoms were metamorphopsia, vision loss and scotoma. Some studies have suggested the geographical variation in inflammatory conditions leading to i-CNV, especially in infectious causes [14-16]. Timely detection of CNV with concomitantly managing inflammation will stabilize or even improve visual acuity. The use of corticosteroids is well documented in various uveitic conditions and for i-CNV believing that persistent, low-grade inflammation in eyes with seemingly inactive clinical disease could lead to a vicious cycle of angiogenesis and scarring and used as first line treatment for i-CNV in non-infectious uveitis [17-19]. As with the majority of these treatment modalities, recurrence rate is high, anti-VEGF therapy is emerging as the primary treatment modality for i-CNV with favorable outcomes. In our study, anti-VEGF injections were used in 6 eyes and a favorable visual outcome was noted in 5 eyes (83.3%) (Figures 1a and 1b). The recurrence of the CNV after primary treatment was noted in 2 eyes (18.18%) in our study. They needed additional immunomodulatory therapy to control the inflammation with anti-VEGF. All eyes except one finally had anatomical regression of the recurrent CNV. Overall the visual outcome was favorable for 9 eyes (81.8%). The pattern of inflammatory CNV may not be entirely uniform throughout the world as observed by us. No prospective randomized studies exist to compare use of anti-VEGF with other modalities of therapy which could probably be due to the low incidence of inflammatory CNV.
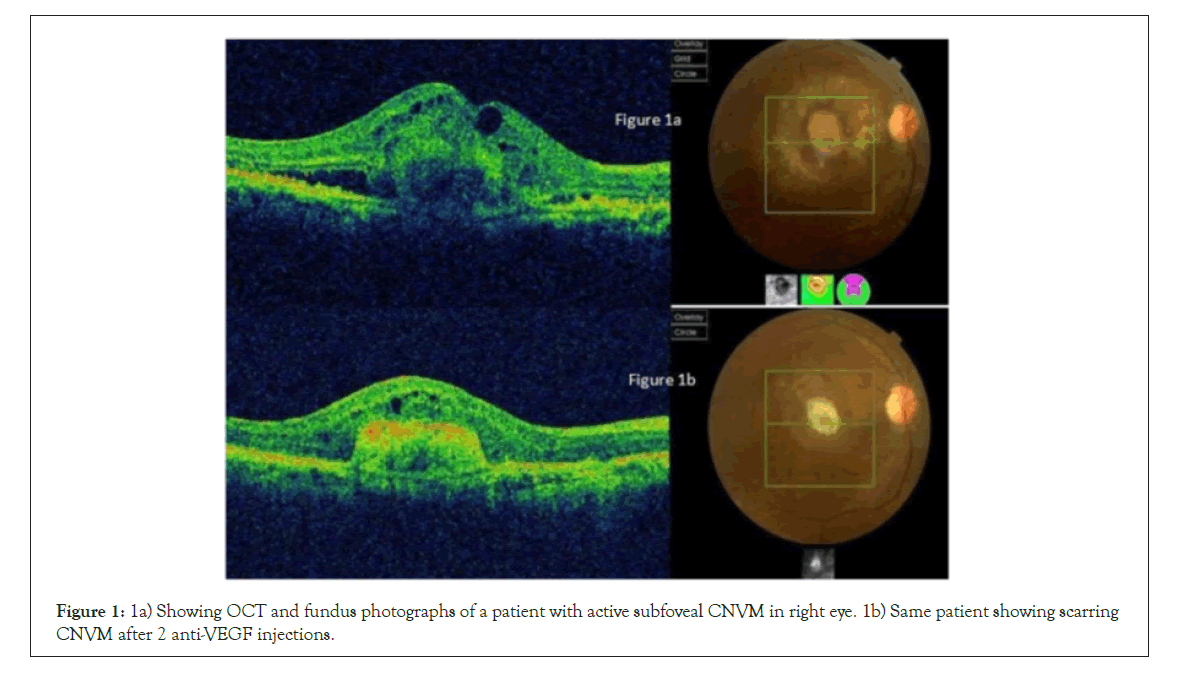
Figure 1: 1a) Showing OCT and fundus photographs of a patient with active subfoveal CNVM in right eye. 1b) Same patient showing scarring CNVM after 2 anti-VEGF injections.
Limitations of our study are being retrospective and small sample size. The detection of i-CNV is very challenging due to the difficulties of visualizing the lesion among inflammatory lesions, pigmentation, significant background fundus scarring, poorly dilating pupil, media haze due to vitritis. Our results showed that a combined approach with anti-VEGF agents and prompt, adequate anti-inflammatory therapy is effective in i-CNV treatment. As this is the first analysis of its kind from central India, longitudinal studies with large sample size would help in more understanding of inflammatory CNV in future.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Khan K, Priyanka, Kishnani M (2021) Analysis of Demographic Clinical Profile, Etiology and Management of Uveitis Related Choroidal Neovascularization Seen at Tertiary Care Centre. J Clin Exp Ophthalmol. 13:903
Received: 10-Dec-2021, Manuscript No. JCEO-21-14926; Editor assigned: 13-Dec-2021, Pre QC No. JCEO-21-14926 (PQ); Reviewed: 27-Dec-2021, QC No. JCEO-21-14926; Revised: 13-Jan-2022, Manuscript No. JCEO-21-14926 (R); Published: 10-Jan-2022 , DOI: 10.35248/2155-9570.22.13.903
Copyright: © 2021 Khan K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.