Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 4
Aim: To study the presence of dry eye disease in patients on topical anti-glaucoma therapy.
Materials and methods: Prospective observational study done on patients presenting with glaucoma to Ophthalmology OPD from 1st November 2019 to 13th April 2021. Patients were examined and cases of glaucoma were identified, based on their history, signs and symptoms. Patients were then assessed for the presence of dry eye disease using schirmer’s test, Tear Break-up Time (TBUT), Ocular Surface Disease Index (OSDI) score, corneal and conjunctival staining. These tests were performed at the time of diagnosis to attain a baseline value which was then compared with another reading at 3 months and 6 months of using topical anti-glaucoma drugs, to assess the severity of dry eye disease.
Results: 276 eyes of 138 patients were evaluated, out of which 21 out of 55 patients instilling beta blocker, 1 out of 35 patients instilling Prostaglandin (PG) analogue, 1 of 13 patients instilling Rho-associated protein kinase (ROCK) inhibitors, 2 out of 6 patients instilling cholinergic drugs and 7 of 18 patients instilling alpha-2 agonists developed dry eye disease at the end of 6 months.
Conclusion: A close relationship was observed between prolonged use of topical anti-glaucoma drugs and dry eye disease. The degree of dry eye disease was correlated with type of anti-glaucoma medication used and also with the duration of use i.e., 6 months or more.
Dry eye; Anti-glaucoma; Schirmer’s test; Ocular surface disease index
Glaucoma is the second leading cause of vision loss worldwide after cataracts [1]. It is a chronic, progressive disease in which retinal ganglion cells degenerate, and subsequent, gradual reductions in the visual field ensues associated with increased Intraocular Pressure (IOP). It is characterised by progressive optic nerve damage and functional defects in the visual field which in the final stage can lead to blindness. Glaucoma is an increasingly common pathology. It is estimated that approximately 60.5 million people worldwide have glaucoma, and it is predicted that the number will escalate to 79.6 million by the year of 2020 mostly due to the rapidly aging population. Although several risk factors are associated with glaucoma onset and progression, the presence of high levels of IOP is the most important risk factor and the only one that can currently be changed [2]. Therefore lowering IOP is the most efficient and clinically accepted form of therapy used to avoid deterioration of the optic disc and progression of visual loss and thus preserve vision. There are five categories of topically administered medications available for the treatment of glaucoma namely, cholinergic agents, adrenergic agonists, carbonic anhydrase inhibitors, adrenoceptor antagonists, and Prostaglandin Analogs (PGAs) whose use has shown good efficacy and safety. Whilst topical medication treatment has undeniable advantages and benefits, it also has certain shortcomings particularly concerning its effect on the ocular surface [3,4].
These drugs along with treatment may also have some side effects like allergic reactions, Ocular Surface Disease (OSD), tear film abnormalities, corneal epitheliopathy, punctate epitheliopathy, medically resistant herpetic keratitis, chronic inflammation, impaired wound healing, squamous metaplasia with high prevalence rate in diabetic and hypertensive patients [5]. OSD and inflammation have been commonly seen with the long term utilization of IOP lowering medication. One of the major components of OSD is dry eye syndrome. Dry eye is a multifactorial disease of the tears and ocular surface that is related with distress, visual disturbance and tear film disturbance with potential to harm the ocular surface [6-8].
After obtaining approval and clearance from Institutional Ethical Committee (IEC), a prospective observational hospital based study was done to evaluate dry eye disease in patients on topical anti-glaucoma therapy in the department of Ophthalmology, SRMS Institute of Medical Sciences, Bareilly, U.P. from 1st November 2019 to 13th April 2021. A prospective observational hospital-based study was carried out from 1st November 2019 to 13th April 2021.
Participants were at least 20 years old who present with glaucoma was undergo dry eye evaluation between 1st November 2019 and 13th April 2021. Patients were examined and cases of glaucoma were identified, based on their history, signs and symptoms.
Patients were assessed for the presence of dry eye disease at the time of diagnosis to attain a baseline value which will then be compared with another reading at 3 months and 6 months of using topical anti-glaucoma drugs, to assess the severity of dry eye disease based on the duration of use of topical anti-glaucoma therapy. It was carried out in the department of Ophthalmology, SRMS Institute of Medical Sciences, Bareilly, Uttar Pradesh. 138 patients who diagnosed with glaucoma presenting to SRMS Ophthalmology department during the study period and patients >20 years old, diagnosed with glaucoma and patients consenting for the study. Also, patients with glaucoma on single topical anti- glaucoma drug were only included.
Demographic characteristics including age, gender, duration of therapy, and study parameters data were noted on a predesigned proforma. Comprehensive ocular examination, aided snellen’s visual acuity, intraocular pressure (Goldman applanation tonometry), ocular surface evaluation tests [Tear Break-up Time (TBUT), Schirmer’s I test, ocular surface staining score, Ocular Surface Disease Index (OSDI), central corneal sensation and in vivo scanning slit confocal microscopy of the central cornea], Dry Eye Workshop Severity (DEWS) classification and OSDI were done.
Tear break-up time
Fluorescein was applied to the ocular surface. The patient was asked to blink a few times before examination. Slit lamp bio- microscopy with a cobalt blue filter was used to investigate the tear film layer. Value of <10 s was considered as indicative of tear film instability.
Schirmer’s test
Whattman filter paper no.41 (measuring 5 mm × 35 mm) was placed in the lower fornix at the lateral one-third of the lower lid margin. The extent of wetting of the strip was measured after 5 min. less than 5.5 mm of wetting was diagnostic of severe dry eye.
Ocular surface staining
The Oxford grading scheme was developed to describe the ocular surface staining in dry eye patients and it has also been used in glaucoma patients with OSD, with the number of glaucoma drops used daily being reported as predictive of corneal staining severity. When using fluorescein under blue illumination, a complementary yellow filter should be used for a more accurate assessment of the conjunctival staining [9].
Assessment of symptoms
The OSDI questionnaire, designed for patients with dry eye [10], has been used to assess the symptoms related to OSD in glaucoma patients, showing higher scores in these patients (Supplementary Figure 1) [11,12].
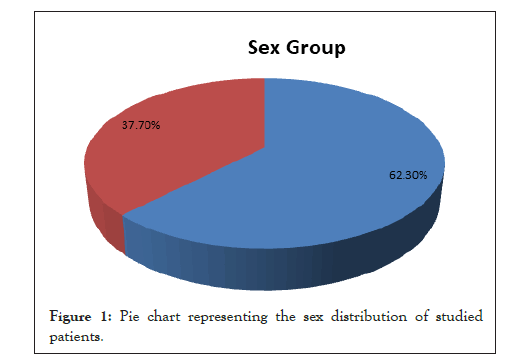
Figure 1: Pie chart representing the sex distribution of studied patients.
The 12 questions of the OSDI questionnaire were graded on a scale of 0-4 where, 0-None, 1-Some of the time, 2-Half of the time, 3-Most of the time, 4-All of the time.
The total OSDI score was then calculated on the basis of the following formula;
OSDI=(sum of all scores for all quest answered) × 100/[ (total number of questions answered ) × 4 ]
276 eyes of 138 patients were taken in the study that was on topical anti-glaucoma therapy for glaucoma was enrolled in our study.
Age group distribution of studied patients was indicated in the table which shows mean age was (Mean ± SD) 47.01 ± 11.43 years (Table 1). Sex group distribution of studied patients was shown (Figure 1). While male patients were 86(62.3%), female patients were only 52(37.7%) as stated in the table. Male to female ratio was 1.6:1 (Table 2).
| Age group (Years) | Frequency (n=138) | Percentage (%) |
|---|---|---|
| ≤ 30 | 15 | 10.90% |
| 31-40 | 27 | 19.60% |
| 41-50 | 44 | 31.90% |
| 51-60 | 34 | 24.60% |
| 61-70 | 18 | 13.00% |
| Mean ± SD (min to max) | 47.01 ± 11.43 (24-70) Years | |
Table 1: Age group distribution of studied patients.
| Anti-glaucoma drug prescribed | No of patients (n=138) | No. of eye (n=276) | Percentage (%) |
|---|---|---|---|
| Beta Blockers (Timolol) | 63 | 126 | 45.65% |
| PG Analogues (Travoprost) | 35 | 70 | 25.36% |
| RHO-Kinase (Netarsudil) | 13 | 26 | 9.42% |
| Cholinergic (Pilocarpine) | 6 | 12 | 4.35% |
| Alpha-2 Agonist (Brimonidine) | 21 | 42 | 15.22% |
Table 2: Distribution of anti-glaucoma drug prescribed in studied patients.
Table 2 depicts results of ocular surface evaluation tests analyzed by long term anti-glaucoma medication group. Anti- glaucoma medication group has carried out different tests like Mean OSDI, Schirmer’s I test, TBUT (s), and corneal staining score, and conjunctival for ocular surface evaluation at different time intervals. The P-values of the difference of results between the initial eye status and that after 6 months of treatment was P=<0.001 which implies that difference between the two was substantial or significant (Table 3).
| Dry eye after 1st month | Total no. of eye (%) | ||
|---|---|---|---|
| No | Yes | ||
| Beta blockers (Timolol) | 110 (87.3%) | 16 (12.7%) | 126 (45.65%) |
| PG analogues (Travoprost) | 70 (100.0%) | 0 (0.0%) | 70 (25.36%) |
| RHO-Kinase (Netarsudil) | 26 (100.0%) | 0 (0.0%) | 26 (9.42%) |
| Cholinergic (Pilocarpine) | 12 (100.0%) | 0 (0.0%) | 12 (4.35%) |
| Alpha-2Agonist (Brimonidine) | 36 (85.7%) | 6 (14.3%) | 42 (15.22%) |
| Total | 254 (90.0%) | 22 (8.0%) | 276 (100.0%) |
Table 3: Association among anti-glaucoma medication prescribed and dry eye after 1st month.
Table 3 shows association among anti-glaucoma medication prescribed and dry eye after 1st month. On perusal of the results it became evident that beta blockers and alpha-2 agonists, both of these are responsible for dry eye and such prescriptions should be made selectively although statistically insignificant (Table 4). Table 4 shows Ocular Surface Disease Index (OSDI), base line OSDI score has been increasing irrespective of the anti- glaucoma drugs prescribed or used. However, since the P-values of the difference in OSD score after 1 month and 6 months of usage of drugs was P=<0.001, the variation in OSD Score both in respect of time as well as in respect of drugs prescribed was significant (Table 5). Table 5 shows schirmer’s test distribution and anti-glaucoma drugs prescribed. We observed that P<0.001 after 6 months of usage of various anti-glaucoma drugs for dry eye treatment. This signifies that the difference in the variation in efficacy of each of these drugs was significant after 6 month of usage. However, in the 1st 30 days the effect was also significant as P-value=0.019 for beta-blockers and alpha-2 agonists (Table 6). Table 6 shows Tear break-up Time (TBUT) and anti-glaucoma drugs prescribed. For TBUT test also the P=0.006 after 6 months of usage of different drugs, which suggests that the variation in efficacy of different drugs utilized was significant after 6 months only. After 1 month of usage, however, the difference in effect was not significant as P=0.234 (Table 7). Table 7 shows corneal staining score distribution and anti-glaucoma drug prescribed. We observed that while P value of the corneal staining score after one month of medication was <0.001, it was 0.009 after 6 months of medication. This suggests that the variation in the efficacy of these anti-glaucoma drugs was significant after 1 month and significant after 6 months (Table 8). Table 8 shows conjunctival staining score distribution in anti-glaucoma drugs prescribed. We observed that while P-value of the conjunctival staining score after one month of medication was P=0.036, it was P=<0.001 after 6 months of medication. This suggests that the variation in the efficacy of these Anti-glaucoma drugs was highly significant after 6 month (Table 9). Table 9 shows association of dry eye with various classes of anti-glaucoma medication prescribed. We observe that P-value of dry eye after 6 months of glaucoma medication was <0.001. This suggests that the variation in the efficacy of these anti-glaucoma drugs was highly significant after 6 month of usage.
| OSD score at base line | OSD score after 1stmonth | OSD score after 6thmonth | |
|---|---|---|---|
| Beta blockers | 6.67 ± 1.54 | 9.98 ± 3.12 | 12.25 ± 3.32 |
| PG analogues | 6.37 ± 1.69 | 7.51 ± 1.66 | 9.54 ± 1.43 |
| RHO-Kinase | 6.38 ± 1.30 | 7.85 ± 1.54 | 10.12 ± 2.23 |
| Cholinergic | 6.50 ± 1.62 | 8.92 ± 1.88 | 12.00 ± 3.02 |
| Alpha-2 Agonist | 6.59 ± 1.55 | 9.74 ± 3.19 | 12.26 ± 2.77 |
| P-value | 0.728 | <0.001 | <0.001 |
Table 4: OSDI score distribution and anti-glaucoma drug prescribed.
| Schirmer's at base line | Schirmer's after 1stmonth | Schirmer's 6thmonth | |
|---|---|---|---|
| Beta blockers | 13.59 ± 1.98 | 12.20 ± 2.25 | 10.72 ± 2.81 |
| PG analogues | 13.67 ± 1.99 | 12.94 ± 1.43 | 12.83 ± 1.70 |
| RHO-Kinase | 13.73 ± 2.03 | 13.00 ± 1.47 | 12.62 ± 2.28 |
| Cholinergic | 13.67 ± 1.67 | 12.17 ± 1.03 | 11.08 ± 2.19 |
| Alpha-2 agonist | 13.67 ± 2.11 | 11.88 ± 2.31 | 10.62 ± 2.71 |
| P-value | 0.997 | 0.019 | <0.001 |
Table 5: Schirmer’s test distribution and anti-glaucoma drugs prescribed.
| TBUT at base line | TBUT after 1st month | TBUT 6th month | |
|---|---|---|---|
| Beta blockers | 12.17 ± 1.66 | 11.21 ± 1.87 | 10.25 ± 2.47 |
| PG analogues | 12.19 ± 1.90 | 11.21 ± 1.37 | 11.10 ± 1.58 |
| RHO-kinase | 12.27 ± 1.51 | 11.96 ± 1.54 | 11.73 ± 1.93 |
| Cholinergic | 12.00 ± 0.95 | 11.25 ± 1.14 | 10.25 ± 2.42 |
| Alpha-2 agonist | 12.17 ± 1.90 | 11.02 ± 1.67 | 10.31 ± 2.27 |
| P-value | 0.995 | 0.234 | 0.006 |
Table 6: Tear break-up time (TBUT) distribution and anti-glaucoma drugs prescribed.
| Corneal staining score base line | Corneal staining score after 1 month | Corneal staining score after 6th month | |
|---|---|---|---|
| Beta blockers | 0.77 ± 0.63 | 1.34 ± 0.54 | 2.39 ± 1.46 |
| PG analogues | 0.69 ± 0.67 | 1.56 ± 0.50 | 1.81 ± 0.79 |
| RHO-kinase | 0.77 ± 0.71 | 1.65 ± 0.48 | 1.96 ± 0.72 |
| Cholinergic | 0.83 ± 0.72 | 2.00 ± 0.00 | 2.58 ± 0.90 |
| Alpha-2 agonist | 0.67 ± 0.65 | 1.43 ± 0.63 | 2.55 ± 1.70 |
| P-value | 0.819 | <0.001 | 0.004 |
Table 7: Corneal staining score distribution in anti-glaucoma drug prescribed.
| Conjunctival staining score base line | Conjunctival staining score after 1 month | Conjunctival staining score after 6 month | |
|---|---|---|---|
| Beta blockers | 1.10 ± 0.59 | 1.52 ± 0.69 | 2.28 ± 1.55 |
| PG analogues | 1.11 ± 0.60 | 1.37 ± 0.49 | 1.41 ± 0.60 |
| RHO-kinase | 1.19 ± 0.57 | 1.50 ± 0.51 | 1.69 ± 0.97 |
| Cholinergic | 1.00 ± 0.60 | 1.58 ± 0.51 | 2.33 ± 1.15 |
| Alpha-2 agonist | 1.29 ± 0.55 | 1.74 ± 0.45 | 2.45 ± 1.19 |
| P-value | 0.394 | 0.036 | <0.001 |
Table 8: Conjunctival staining scores distribution and anti-glaucoma drugs prescribed.
| No of eye | Dry eye after 6 month | P value | ||
|---|---|---|---|---|
| No | Yes | |||
| Beta blockers | 110 | 68 (61.8%) | 42 (38.2%) | <0.001 |
| PG analogues | 70 | 68 (97.1%) | 2 (2.9%) | |
| RHO-kinase | 26 | 24 (92.3%) | 2 (7.7%) | |
| Cholinergic | 12 | 8 (66.7%) | 4 (33.3%) | |
| Alpha-2 Agonist | 35 | 21 (60.0%) | 14 (40.0%) | |
Table 9: Association of dry eye with various classes of anti-glaucoma medications.
Glaucoma is the second leading cause of visual impairment around the world [13]. It is a chronic disease that damages optic nerve and produces defects in the visual field which, in the last stage, can cause blindness. Treatment of glaucoma involves lifelong follow up.
For Primary Open-Angle Glaucoma (POAG) patients, first-line of treatment comprises of medical management. Topical anti- glaucoma drugs are the standard type of treatment, which are regularly utilized for longer duration in various dosing. These drugs along with treatment may also have some side effects like allergic reactions, OSD, tear film abnormalities, corneal epitheliopathy, punctate epitheliopathy, medically resistant herpetic keratitis, chronic inflammation, impaired wound healing, and squamous metaplasia with high prevalence rate in diabetic and hypertensive patients [14]. OSD may result in poor effectiveness of glaucoma treatment leading to irreversible damage to eyes. One of the major components of OSD is dry eye syndrome. Dry eye is a multi-factorial disease of the tears and ocular surface that is related with distress, visual disturbance and tear film disturbance with potential to harm the ocular surface. Mean age was (Mean ± SD) 47.01 ± 11.43 years. In a similar study Saini [14] reported the mean age of their study patients were 49.42 ± 16.98 (range, 22-75) years, and Zulfiqar [15] reported the mean age of the patients was 50.76 ± 15.67 years, while Kurna [16] reported the mean age of the patients was 58.33 ± 11.24 years and Sahlu, et al. [17] reported the mean ± SD age was 62.2 ± 11.58 (range, 41-87) years in the glaucoma patients in their respective study.
The present study demonstrated that the male patients were 86(62.3%) and female patients were only 52(37.7%) with male to female ratio was 1.6:1. Sahlu and Giorgis [7] reported the male to female ratio was 1.1:1. Nielsen and Eriksen [18] underlined how in 64 patients treated with timolol eye drops, seven patients developed transitory sensation of dry eyes. Two of these subjects also had xerostomia. In all these seven patients a reduction of Schirmer test and break-up time was noted. Our study showed TBUT test also the P=0.006 after 6 months of usage of different drugs, which suggests that the variation in efficacy of different drugs utilized was significant after 6 months only. After 1 month of usage, however, the difference in effect was not significant as P=0.234 [16] reported the There was no statistically significant difference in mean SCH I test results between the groups at any time of the study (P>0.05) (Table 1). There was no significant TBUT change in groups 1, 2, 3, and 6 before and after the treatment, while TBUT decreased significantly in group 4 at 1st week and 1st month controls (P=0.048, P=0.0019). They also reported that there was no significant difference in corneal and temporal conjunctival SS in the baseline (P=0.120; P>0.05).
Topical anti-glaucoma medications have various side effects such as dry eye, irritation, redness, burning, hyperpigmentation, lengthening of eyelashes. Dry eye is the commonest side effect, severity of which varies with type and duration of use of topical anti-glaucoma medication. Propensity of the disease could range from mild dry eye to ocular discomfort disrupting routine lifestyle; hence it is an important aspect which must be catered to. Long term preservative containing anti-glaucoma therapy was significantly correlated to ocular surface staining scores, TBUT, OSDI values and Schirmer’s test and needs further studies and evaluation. Concurrent topical lubricant and anti-inflammatory treatment may be considered in cases of chronic preservative containing anti-glaucoma therapy showing ocular surface changes.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Batra R, Mehrotra N, Singh S, Rizvi S (2022) An Evaluation of Dry Eye Disease in Patients on Topical Anti-Glaucoma Therapy. J Clin Exp Ophthalmol. 13:922.
Received: 22-Mar-2022, Manuscript No. JCEO-22-16357; Editor assigned: 24-Mar-2022, Pre QC No. JCEO-22-16357 (PQ); Reviewed: 07-Apr-2022, QC No. JCEO-22-16357; Revised: 12-Apr-2022, Manuscript No. JCEO-22-16357 (R); Published: 19-Apr-2022 , DOI: 10.35248/2155-9570.22.13.922
Copyright: © 2022 Batra R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.