Mycobacterial Diseases
Open Access
ISSN: 2161-1068
ISSN: 2161-1068
Case Report - (2022)Volume 12, Issue 7
Tuberculosis (TB) is one of the most dreaded infectious cause of death worldwide. Any organ can be involved, but cardiac involvement is extremely rare. Tuberculosis with myocardial involvement and severe systolic dysfunction is rarely reported. As this kind of presentation is rare in our country, we aim to report this rare case scenario. An 11- year-old female child who was diagnosed with Pulmonary tuberculosis involving Lung, and lymph nodes with cardiac symptoms of chest pain and shortness of breath with echo findings suggestive of dilated LA, LV/Moderate MR/ Moderate LV dysfunction with LVEF-35% with chest x-ray showing multiple diffuse patchy infiltrates in bilateral lungs with ECG features of sinus tachycardia with normal USG abdomen. The patient was on anti-tuberculosis therapy and congestive heart failure therapy like digoxin, diuretic (furosemide) and ace-inhibitor (enalapril) with supportive management and got discharged after 10 days of hospital stay. The patient has been advised for further regular follow-up visits to look for clinical improvement. The child's clinical status improved by adequate weight gain; her tachycardia has been reduced with improvement in cardiac activity.
Myocarditis; Tubercular myocarditis; Heart failure; Left Ventricular Dysfunction (LVD); Congestive Heart Failure (CHF)
Tuberculosis (TB) affecting myocardium is extremely rare, prevalence being in the range between 0.14% and 0.2%according to several studies [1,2]. Males are commonly affected than females, especially in immunocompetent. Often diagnosed postmortem with high mortality rate. Sudden cardiac deaths, constitute eighty-one (81%) which occur in the ‘young’ patients among the reported fatalities. Most of the times it is asymptomatic, but sometimes may present with Ventricular fibrillation, dilated cardiomyopathy, Congestive heart failure, long QT syndrome and even sudden cardiac arrest. Myocardial involvement can be of three types namely: nodular tubercles of myocardium (featured by central caseation); myocardial miliary tubercles; and rare diffuse infiltrative type associated with tuberculous pericarditis (featured microscopically by giant cells and lymphocytes) [3,4]. Myocardial involvement can be due to retrograde lymphatic spread from mediastinal lymph nodes or by direct invasion from pericardium [5,6]. If clinical findings and echocardiography findings are suggestive of myocardial tuberculosis then we may confirm the disease by myocardial biopsy. Tubercular myocarditis is commonly missed most of the times, due to insidious onset and progression along with low incidence rates.
There’s knowledge gap among treating doctors regarding the low incidence, late diagnosis and early initiation of treatment. This case report, therefore, aims at creating awareness among the practitioners, to help in diagnosing such rare scenarios and to initiate timely management of tuberculous myocarditis.
An 11-year-old female child of second birth order, born out of non-consanguineous marriage with a premorbid normal perinatal and developmental history was previously diagnosed as a case of pulmonary tuberculosis (microbiologically proven) and started on anti-tuberculosis therapy in november 2021, who was not compliant to anti-tuberculosis therapy presented to the pediatric emergency of All India Institute of Medical Sciences (Rishikesh, India) in February 2022 with shortness of breath, chest pain, loss of appetite and generalized weakness for 15 days duration. She developed shortness of breath at rest, Modified Medical Research Council (MMRC) grade 4 which was acute in onset, progressively increasing associated with chest pain. Chest pain was acute in onset, progressively increasing, associated with palpitations and anxiety, radiating to the epigastric region with cool extremities and aggravated by movement. The child had a loss of appetite and generalized weakness for 3-5 days before the episode. There was no history of any co morbidities (diabetes mellitus, hypertension, smoking, illicit drug abuse, or renal disease). Family history of tuberculosis (pulmonary TB) in the maternal uncle was evident 6 years back and completed a course of ATT.
On examination, the child was severely emaciated with short stature <-3 Standard deviations (SD) with pallor+, clubbing+ (Grade 1) with other general examination findings being normal.
Vitals
Pulse: 130/min; Respiratory rate: 26/min; Blood pressure: 60/35 mmHg; SpO2: 96% on Room air.
Systemic examination
There was a protrusion of ribs on the anterior chest with scattered fine crepitations in both lung fields and no other significant findings in other systems. Initial Laboratory workup revealed Hemoglobin 11.8 mg/dl, total leucocyte count-10310/ mm3, platelets 559000/mm3, Mean Corpuscular Volume (MCV) 87.5 fL, C-reactive protein 71 mg/dl. Renal function tests, liver function tests and serum electrolytes were normal. Given suspected cardiogenic shock child has been started with a low volume fluid bolus followed by inotropes in an emergency. Viral markers (hepatitis B virus, hepatitis C virus and Human Immunodeficiency Virus (HIV) were negative. Ultrasonographic findings of abdomen was normal. Cardiac biomarker creatine kinase-MB was slightly elevated. Electrocardiography (ECG) showed sinus tachycardia as shown in Figure 1. Chest radiography was done which revealed multiple diffuse patching infiltrates in bilateral lung fields as shown in Figure 2.
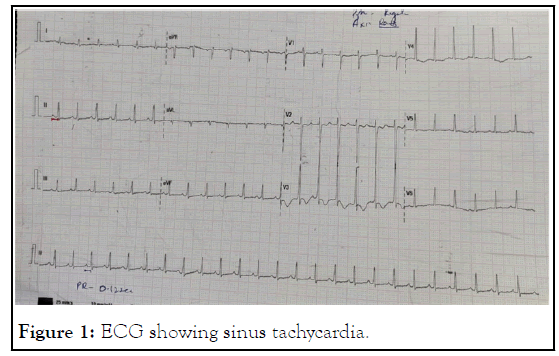
Figure 1: ECG showing sinus tachycardia.
Figure 2: Chest X-ray showing multiple diffuse patchy infiltrates of bilateral lungs.
Echocardiography showed-dilated Left Atria (LA), Left Ventricle (LV) in apical four-chamber view with moderate Mitral Regurgitation (MR), with moderate left ventricular dysfunction -35% as shown in Figure 3.
Figure 3: Echocardiography showing the above-mentioned features in the child.
The child was admitted and worked up for multi-drug resistanttuberculosis- as the child was not compliant to medication and presented with sudden onset of distress, but Cartridge Based Nucleic Acid Amplification Test (CBNAAT) report showed rifampicin sensitivity hence continued first line ATT (isoniazid, rifampicin, ethambutol) along with heart failure medication (diuretics, digoxin, Angiotensin-Converting Enzyme (ACE) inhibitors. The child was given supportive management with appropriate dietary advice and after 10 days of hospital admission, the child was clinically improving and symptoms were subsided and advised for further follow-up for cardiac screening and have been explained about the further prognosis of the child.
Despite the lack of myocardial biopsy for definitive diagnosis of myocardial involvement in our patient, the clinical presentation, investigations and dramatic response to anti-tuberculosis treatment were all in favour of myocardial dissemination.
Tubercular myocarditis is rare disease with only a few cases being reported in the literature. Approximately about 1% of all cases of tuberculosis have cardiac involvement [2]. Tuberculosis mostly affects the pericardium in endemic areas. Endomyocardial biopsy is not always feasible for accurate diagnosis of myocardial tuberculosis due to its limitations and associated complications.
However, diagnosis is usually made based on medical history, clinical presentation, laboratory findings and imaging studies. Myocarditis can be diagnosed clinically in the presence of elevated cardiac markers of injury (Cardiac troponin I or troponin T, and creatine kinase-Mb) with regional or globally depressed left ventricular function seen on echocardiography or cardiac magnetic resonance scan in the absence of coronary artery disease. In our case, the symptomatology, the presence of hypokinesis in left ventricular regional wall with depressed systolic function with slight elevation of cardiac injury marker (creatine kinase MB), with no other obvious cause of myocarditis strongly suggests myocarditis secondary to TB.
In our case, child was treated with anti-tuberculous therapy, digoxin, enalapril, lasix (Furosemide). We have advised the patient for regular follow-up visits to look for clinical improvement as well as improvement in her cardiac function through anti-tuberculous therapy.
Follow up echo
Mild Dilation of LA, LV with mild MR and LV function-45% by simpson's method as shown in Figure 4.
Figure 4: Follow-up echocardiography findings.
During follow-up, LV function is improved by 15% with ATT, diuretics and Angiotensinogen Converting Enzyme (ACE) inhibitors.
Her Anti-streptolysin O titres (ASO) (200 IU/ml) are also in decreasing trend without Rheumatic prophylaxis. There is good weight gain with 4 kgs from the day of discharge to follow-up.
To conclude this case report, pulmonary tuberculosis associated with myocarditis and left ventricular dysfunction has been rarely reported. Early diagnosis and management can bring the best outcome. Therefore, in tuberculosis endemic areas like India, it should be suspected in patients with unexplained left ventricular systolic dysfunction in the absence of coronary artery disease. Regular follow-up of the case is essential in looking for clinical improvement as well as a better prognosis.
Citation: Charan GK, Verma PK, Joshnaa M, Shrivastava Y (2022) Acute Myocarditis and Heart Failure due to Tuberculosis. Mycobact Dis. 12:305.
Received: 26-Sep-2022, Manuscript No. MDTL-22-18847; Editor assigned: 29-Sep-2022, Pre QC No. MDTL-22-18847 (PQ); Reviewed: 12-Oct-2022, QC No. MDTL-22-18847; Revised: 19-Oct-2022, Manuscript No. MDTL-22-18847 (R); Published: 28-Oct-2022 , DOI: 10.35248/2161-1068.22.12.305
Copyright: © 2022 Charan GK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.