Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2023)Volume 14, Issue 6
An 18-year-old female presented with 2-year history of intermittent worsening of vision and floaters in her left eye. Complete ophthalmological examination was performed. The Best Corrected Visual Acuity (BCVA) was 1.25 in both eyes. Cells in anterior chamber and vitreous humor were present in the left eye and the posterior segment examination revealed a localized area with dilated retinal vessels and massive white masses in the vitreous humor in the same eye. Examination revealed normal findings in the right eye. A broad investigation disclosed positive Epstein-Barr virus Immunoglobulin M (IgM), borderline high levels of Toxocara canis antigen and normal levels of eosinophils. The clinical findings were not concurrent with a typical uveitis. Therefore, atypical intraocular lymphoma, retinoblastoma and infectious etiologies were suspected. After informed consent and following negative cerebral and orbital magnetic resonance imaging findings, a Fine Needle Aspiration Biopsy (FNAB) from the left vitreous humor masses was performed. The vitreous sample revealed malign small cell tumor with necrosis, hyperchromatic nuclei and high nucleus-to-cytoplasm ratio most likely compatible with retinoblastoma. Ocular salvage treatment modalities with chemotherapy, plaque brachytherapy and external radiation granted BCVA of 0.5 without tumor recurrence over 25 years’ follow-up. The reduction in visual acuity was related to posterior capsular opacification of the lens secondary to radiation.
Visual acuity; Retinoblastoma; Vitreous humor; Ocular salvage
Retinoblastoma, the most common intraocular malignant tumor of infancy and childhood, develops from immature retinal cells. The mutational inactivation of both alleles of the retinoblastoma (Rb1) gene on chromosome 13q results in development of retinoblastoma [1]. It is commonly detected before the age of 3. The detection of retinoblastoma in patients older than 4 years is considered uncommon [2]. A multicenter study including 40 European countries demonstrated a live birth incidence rate of 1 in 13. The combined age cohort incidence rate illustrated 14.1 and 4.6 per 1 million children younger than 5 and between 5 to 15 years, respectively [3]. The statistics depicts the age distribution of retinoblastoma in the USA. About 95.7% (630 cases) fell under the age of 4 and 4.3% (28 cases) into age between 5 and 9 [4]. For first time, Maghy [5] described bilateral retinoblastoma in an adult, a 20-year-old female. Retinoblastoma is rare in adults and presents commonly at advanced stage that may necessitate enucleation. In an adult patient with suspected intraocular malignancy where enucleation is not the obvious treatment, the clinician should strive for a diagnosis based on biopsy [6].
In this case report, we describe a cytological verified adult-onset retinoblastoma treated with vision salvage therapy including chemotherapy, brachytherapy and external radiation with 25-year follow-up without recurrence.
A previously healthy female presented at the age of 18 with 2-year history of intermittent worsening of vision and floaters in her left eye, perceived as a pars planitis unresponsive to steroid treatment. Her BCVA was 1.25 in both eyes and the intraocular pressure was normal. The ophthalmological examination revealed no precipitates, but cells in the anterior chamber and vitreous humor, pathologically dilated retinal vessels at 7, 9 and 10 o’clock positions peripherally and dense white masses localized from 4 to 11 o’clock positions and small clumps of white masses located pre- retinally at 1 and 9 o’clock positions as shown in Figures 1A-1F. A clinical diagnosis of atypical uveitis was made, and investigations with blood tests and imaging were conducted. The blood tests revealed positive Epstein-Barr virus IgM and borderline high levels of Toxocara canis antigen. Microbiology report did not reveal other viruses (hepatitis A and B, HIV, parvovirus 19, rubella, varicella zoster, herpes simplex and cytomegalovirus), bacteria (no bacteria, particularly negative for Chlamydia and Borrelia) or parasite (particularly Toxoplasma gondii and Yersinia entrocolitica). The cerebral magnetic resonance imaging including the orbit did not reveal any pathological findings. A localized calcification was seen on ultrasound B-scan at 9 o’clock positions on the surface of the retina as shown in Figure 1E. Computerized Tomography (CT) scan detected a grain calcification in the same position. The retina was attached and no iris or anterior chamber angle neovascularization was observed. Due to possibilities of atypical lymphoma, retinoblastoma, vascularized tumor, sarcoidosis or infectious etiologies, a diagnostic FNAB from vitreous mass was performed with a 23-gauge needle via pars plana and a 25-gauge from the anterior chamber for microbiological and cytological examinations. A total number of two samples were taken. The pathologist was present under the surgical procedure and confirmed adequate aspiration samples. A pre-planned diagnostic vitrectomy was promptly cancelled. The samples revealed malign small cell tumor with necrosis, hyperchromatic nuclei and high nucleus-to-cytoplasm ratio that was compatible with retinoblastoma. Some nests of viable tumor cells were seen as shown in Figure 2. The results did not reveal lymphoma (negative Leucocyte Common Antigen (LCA), CD3, CD20), but also markers for retinoblastoma (chromogranin and CD56 (immune cell marker)) were negative. Her second cousin had presented with unilateral retinoblastoma at birth (her paternal grandmother and his paternal grandfather were siblings). The gene testing did not reveal any mutation in retinoblastoma (Rb1) gene. She did not share a common retinoblastoma haplotype with her second cousin. Therefore, her case was considered sporadic (Figures 1A-1F and 2).
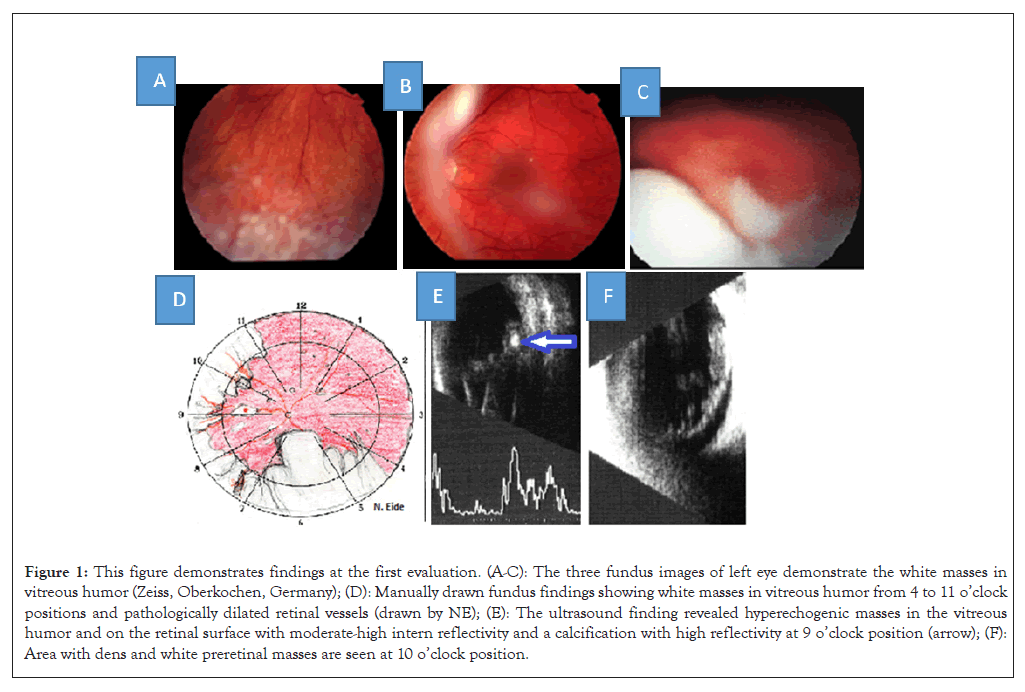
Figure 1: This figure demonstrates findings at the first evaluation. (A-C): The three fundus images of left eye demonstrate the white masses in vitreous humor (Zeiss, Oberkochen, Germany); (D): Manually drawn fundus findings showing white masses in vitreous humor from 4 to 11 o’clock positions and pathologically dilated retinal vessels (drawn by NE); (E): The ultrasound finding revealed hyperechogenic masses in the vitreous humor and on the retinal surface with moderate-high intern reflectivity and a calcification with high reflectivity at 9 o’clock position (arrow); (F): Area with dens and white preretinal masses are seen at 10 o’clock position.
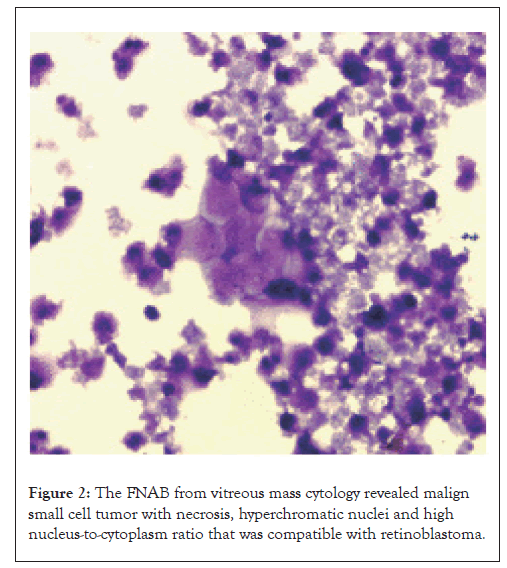
Figure 2: The FNAB from vitreous mass cytology revealed malign small cell tumor with necrosis, hyperchromatic nuclei and high nucleus-to-cytoplasm ratio that was compatible with retinoblastoma.
Her presentation as an adult-onset retinoblastoma was discussed with an expert in retinoblastoma abroad (Dr. J. Hungerford in England). To stage the retinoblastoma a bone marrow and a spinal fluid examination were performed. These investigations did not reveal metastases. He did not find any indication for enucleation at that point of time, but he recommended cryotherapy over the puncture site followed with chemotherapy, according to the retinoblastoma protocol used at St. Bartholomew Hospital. Cryotherapy was applied to break blood-retina barrier prior to chemotherapy. She was initially treated with chemotherapy (vincristine, carboplatin and etoposide) monthly for 4 months, and with the addition of cyclosporine for 3 months. Due to dissatisfying chemotherapy effect on the tumor masses, treatment with Ruthenium brachytherapy was performed 2 months after initiation of chemotherapy following diagnosis of retinoblastoma with (CIB 20 mm plaque, doses were calculated to 40 Gray (Gy) and dose rate to 0.76 Gy/hour). Treatment with extern radiation therapy (two-field, 46 Gy in 23 fractions over 4-week period) was given after completion of chemotherapy.
Approximately three years following the diagnosis of retinoblastoma her BCVA deteriorated to 0.7 in her left eye due to posterior capsular opacification of the lens secondary to external radiation.
In 2004, she experienced persistent fatigue, headache and dizziness. These symptoms most likely were related to long-term adverse effect of chemotherapy and radiation therapy [7]. To our delight, the symptoms of chronic fatigue disappeared almost spontaneously.
Approximately 2 decades following chemotherapy, brachytherapy and external radiation therapy, the BCVA remained 0.7 in her left eye with posterior capsular opacification of the lens. Twenty- five years following multi-modal vision salvage therapy, her BCVA had deteriorated to 0.5 due to increasing cataract. The Optical Coherence Tomography (OCT) images of the left macula demonstrated normal layers, but blurry images due to cataract. She is educated and works as a social worker, and has a healthy boy aged 14 years. Her health has been good otherwise. She described her social life as normal.
Generally, all treatment shall be based on a definite diagnosis based on clinical features and pathological verification if possible. This is mandatory especially if the process is an aggressive malignant disease. In our case the age, the long period with minor symptoms and the excellent visual acuity reduced the probability of a retinoblastoma. The ultrasound B-scan and CT scan both verified calcification. We considered the white mass to be debris from a neoplasm, but a retinoblastoma was not suspected as the most likely etiology. Nevertheless, an experienced cytopathologist was in the operating theatre to evaluate the quality and quantity of the harvested material. It was sufficient to establish a diagnosis without doubt. Therefore, a stepwise approach with a subsequent vitrectomy was avoided. The poorly cohesive tumor cells in retinoblastoma increases the risk for seeding.
Previously, intraocular operations are generally deferred due to the risk of reactivation of retinoblastoma. Especially intervention in posterior segment is considered risky, however, cataract surgery has been considered as safe and effective in most cases [8,9]. Although some small white opacities are still seen in the vitreous cavity, the risk is low for a reactivation with a follow-up period of 25 years. In this case, the other eye is completely normal. Her vision deteriorated to 0.5 in the treated eye due to posterior opacification in the lens secondary to radiation. We have not seen a need for cataract surgery yet, although cataract surgery is safe and effective. An expert in retinoblastoma treatment supports the low risk assessment [10].
The diagnosis of adult-onset retinoblastoma may be challenging especially if a diagnostic dilemma co-exists or if presentation could mimic other diagnosis such as inflammatory diseases, endophthalmitis, leukemia, lymphoma, melanoma, astrocytoma and metastasis. Adult-onset retinoblastoma may present atypically. In a review of 45 cases of adult-onset retinoblastoma, the majority of patients presented with dimness of vision and floaters [11]. Our patient presented with symptoms of uveitis with positive serology for Epstein-Barr virus IgM and borderline high levels of Toxocara canis antigen. The exudation was unresponsive to steroid medication. Due to diagnostic challenge, FNAB from vitreous mass was performed and the cytological diagnosis of retinoblastoma was made. In atypical cases, diagnostic samples from vitrectomy or fine needle aspiration may provide accurate diagnosis. Vitrectomy and FNAB cytology are considered controversial due to seeding of tumor cells. Karcioglu, et al. [12] reported surgical instruments even as a 25-gauge needle can seed tumor into the scleral wound and the orbit. Shields, et al. [13] reported management and prognosis following vitrectomy in 11 eyes with unsuspected retinoblastoma. The preoperative diagnosis included vitreous hemorrhage (64%), toxocariasis (18%), toxoplasmosis (9%) and endophthalmitis (9%). The mean age of patients at vitrectomy was 6 years. Retinoblastoma was suspected under vitrectomy in two patients (18%), on cytological examination of vitreous samples in 8 patients (73%) and at the examination at specialist ocular oncology hospital after vitrectomy at referral hospital in one patient (9%). Enucleation was performed in all 11 patients with adjuvant treatment in 10 patients (using radiotherapy in 9 patients and chemotherapy in 9 patients) and as a treatment of existing metastatic retinoblastoma in one patient. During the mean follow-up time of 7 years, none of the patients showed any sign of metastatic disease or local orbital recurrence except for the patient who was referred with existing metastasis who died 24 months later despite chemotherapy and radiotherapy.
Stevenson from Hungerford’s group reported three cases of retinoblastoma with orbital and local lymph node recurrence following vitrectomy for unsuspected retinoblastoma. All three patients were treated with enucleation, but without adjuvant chemotherapy or radiotherapy initially. The patients were treated with aggressive chemotherapy and radiotherapy at the tumor recurrence. The authors recommended referral of retinoblastoma patients for early adjuvant therapy due to poor prognosis in metastatic retinoblastoma [14]. In this context, it is very important to stress that a proper and complete work-up must be performed first. A biopsy must not be used as a shortcut to diagnosis. A uveitis masquerade syndrome can be a diffuse retinoblastoma in an older child. Calcification may be lacking and the intraocular pressure can be high [15]. In a retrospective study of a total number of retinoblastoma patients, 8 patients were biopsied through limbus and pars plana with 25 and 27- gauge needles for diagnostic purposes. In six of eight patients, retinoblastoma cells were shown and in other two biopsies, inflammatory cells and benign retinal cells were demonstrated. Five of the cytology verified retinoblastoma eyes underwent enucleation and one patient was treated with cryotherapy and brachytherapy. The average follow-up time for cytology verified retinoblastoma cases was 10.8 years with no recurrent disease [16]. In similarity to the patient who did not undergo enucleation in this retrospective study, our patient did not either undergo enucleation, but was treated with chemotherapy, plaque brachytherapy and external radiotherapy and followed-up for 25 years without recurrence. However, her mental and physical capacity make extraordinary demands challenging for her. This may be due to fatigue and a consequence of the intensive cytostatic treatment that she received 25 years ago.
In conclusion, we report a unique case of cytological confirmed retinoblastoma without tumor recurrence during a follow-up time of 25 years. An adult presentation of retinoblastoma is rare. The current ocular oncology practice rarely requires FNAB for diagnosis of retinoblastoma. However, invasive procedures may be necessary in order to acquire accurate diagnosis in atypical cases, especially if the intention is to retain the eye with useful vision.
Our sincere thanks to Dr. Lisa Walaas (pathologist), Dr. Randi S. Tranheim (ophthalmologist, ocular oncologist) and Dr. Johan E. Tausjo (oncologist) who provided health care for this patient.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Eide NA, Navaratnam J (2023) A Unilateral Adult-Onset Retinoblastoma Treated with Ocular Salvage Treatment Modalities without Recurrence over 25 Years Follow-up Period. J Clin Exp Ophthalmol. 14:962
Received: 27-Oct-2023, Manuscript No. JCEO-23-26118; Editor assigned: 30-Oct-2023, Pre QC No. JCEO-23-26118 (PQ); Reviewed: 13-Nov-2023, QC No. JCEO-23-26118; Revised: 20-Nov-2023, Manuscript No. JCEO-23-26118 (R); Published: 28-Nov-2023 , DOI: 10.35248/2155-9570.23.14.962
Copyright: © 2023 Eide NA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.