Family Medicine & Medical Science Research
Open Access
ISSN: 2327-4972
ISSN: 2327-4972
Research Article - (2021)Volume 10, Issue 7
Background: Indigenous women residing in remote communities experience a disproportionately higher prevalence of nutrition-related chronic diseases. The development of evidence-based programs and policies to minimize these health disparities necessitates a comprehensive understanding of Indigenous women’s nutrition status and dietary intake patterns. However, a knowledge gap exists with respect to baseline maternal nutrition status and dietary intake information among First Nations women living on reserves. Objective: We aimed to systematically synthesize existing literature on maternal dietary information in Indigenous women residing on reserve lands and remote communities. Methodology: The articles that reported a singular nutrient status, multiple nutrients status, meal consumption pattern, and/ nutrition-related biomarkers in First Nations women during childbearing years, pregnancy, and lactation were synthesized for this review. Results: Major nutrient deficiencies identified were fiber, folate, vitamin A, D, and E, calcium, potassium, and magnesium; low consumption of vegetable and fruit, grain, and milk and alternative food groups was observed. A lack of information on maternal nutrient status in maternal, First Nations, on-reserve population obstructed nutrition status evidence appraisal. Conclusion: We recommend that a greater emphasis be placed on improved maternal nutrition surveillance systems, which are designed in partnership with the Indigenous organizations. Development of a sustainable community nutrition monitoring system will allow for the construction of the nutrition information capacity.
Dietary Patterns; First Nations; Indigenous; Maternal Nutrition; Nutrition Status
Maternal health defined as “health during pregnancy, childbirth and postpartum period” is the determinant of an infant’s health, which shapes developmental and growth trajectories throughout one’s life [1]. Maternal health of the First Nations status women is strikingly different from that of the general Canadian population as demonstrated by the maternal and infant mortality rates [2], which are two-fold higher for First Nations women and infants [3,4]. Health disparity among First Nations women is further marked by disproportionately higher rates of adverse nutritionrelated outcomes such as type 2 diabetes [5,6], gestational diabetes (GD) [5-7], obesity [7-9], low and high birthweight babies [6,7,9], stillbirth [10], and intrauterine growth restriction [10,11]. A Canadian study by Dyck et al. [5], found that rates of GD among First Nations women are nearly double that of non-Indigenous women (6.4% vs 3.7%, respectively). The age-adjusted prevalence of type 2 diabetes, which includes women of reproductive age, is 3 to 5 times greater among Indigenous individuals compared to their non-Indigenous counterparts; with the diagnosis occurring at a younger age, associated with a greater degree of complications and severity [7,9]. The prevalence of obesity and abdominal obesity has reached an astounding 65% and 81%, respectively, in select First Nations communities [7]. This is concerning as the relationship between maternal obesity, type 2 diabetes, GD, and poor prenatal and birth outcomes are well documented and result in significant costs to the healthcare system, the family, and the individual.
These maternal health issues in First Nations communities are rooted in a collection of political, historical, and social determinants. The legacy of colonization has elicited multiple jeopardies for Indigenous women. Destruction and appropriation of land, forced relocations [12], child apprehension through residential schooling system [13], and infringement upon autonomy and dignity through the assimilation policies [14] have resulted in tremendous intergenerational trauma to Indigenous communities [13,14]. These colonial infringements affected Indigenous societies and significantly shifted Indigenous women’s identities, autonomy, feminine capacity, and agency exposing women, children, and communities to a higher level of adverse consequences and negative health outcomes [15].
Various policies, federal and provincial programs (Canadian Prenatal Nutrition Program (CPNP), Head Start, Healthy Starts, and Strengthening Families) have sought out to minimize the above-mentioned maternal health disparities for First Nations women [10,16,17]. However, a large knowledge gap exists with respect to baseline maternal nutrition status and dietary intake among First Nations women living on reserves and in remote communities. Furthermore, the evaluation reports expressed that prior to the planning of maternal nutrition programming and health promotion policies for the women identified as being at risk for adverse maternal outcomes, an in-depth perspective on the baseline nutrition status needs to be established [16-18]. To fill this large knowledge gap, this review assessed the state of evidence on the maternal nutrition status information for First Nations women residing on-reserve lands and in remote communities.
This report summarizes the information pertaining specifically to the nutrition status and dietary intake information for First Nations women during pre-pregnancy, pregnancy, and the first year postpartum. This information can be utilized to inform nutrition and prenatal policy approaches, intervention programs, and public health strategies.
Design and Search Strategy
The driving research question for this review was: What is the state of evidence for the maternal nutrition status and dietary pattern information in Fist Nations women residing on reserve lands and in remote Canadian communities? To answer this question, a comprehensive review was performed on the research available on nutrition in pregnancy of Canadian Indigenous women up to the year 2021 without limit on the earliest publication date (Table 1). The review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for scoping reviews checklist (Figure 1) [19]. Databases searched included Embase, Medline, PubMed, Scopus, Science Direct, utilizing the terms “nutritional status” or “nutrition”, or “nutrient”; “Indigenous” or “Aboriginal” or “Tribal”; “pregnancy” or “pregnant” or “prenatal”, or “perinatal”; “food intake” or “meal consumption” or “dietary pattern”, and “deficiencies”. The same terms were also searched in the grey literature-any literature produced outside of scientific publishing channels-from 1980 to 2021, finding community and government reports available online in English. Additionally, a snow-ball method was applied to perform robust citation analysis and to further isolate appropriate and relevant reports.
| Authors | Location | Participants | Methods | Results | Limitations |
|---|---|---|---|---|---|
| Back et al., 2012 [21] | 3 rural FN† communities in Manitoba and urban Winnipeg and | n=41 pregnant FN women; n=22 pregnant CU†† women |
3-day food record | FN women had higher intake of daily cholesterol (325±186 vs 205±137 mg/day; p<0.05), lower intake of vegetable (0.64±0.98 vs 2.94±3.14 servings/day; p<0.01), and skim milk (0.12±0.43 vs 0.25±0.64 servings/day; p<0.01) compared to CU women. | Only 3-day food record, no biological findings; small sample size, limited range of nutrients studied. |
| Berti et al., 2008 [22] | Canadian Arctic Indigenous communities: FN, Dene, Métis, Yukon FN, Inuit. | n=1300 women of child-bearing age (<40yrs); n=74 pregnant; n=117 lactating | 24hr-food recall | Women in the study had varied prevalence of low nutrient intake depending on the community: Mg (10-92%) vitamin A (12-100%), vitamin C (0.4-93%), vitamin E (100%) of women in the study, and folate (22-97%). Infrequent use of nutritional supplement. | Only 24hr-food recall done, no biological findings; limited range of nutrients studied; outdated data collected between 1987 and 1999. |
| Chan, 2010 [23] | Manitoba FN communities | n=324 FN women of child-bearing age (19-50 yrs) |
24hr-food recall; FFQ††† |
Non-pregnant FN women of childbearing age had low median intakes of α-Linolenic acid (1.4 g/day), dietary fiber (12 g/day) vitamin A (305 RAE/day), folate (301 DFE††††/day), Ca (541 mg/day), and Fe (13.7 mg/day). | No results on pregnant and lactating FN women; lack of biological data; limited range of nutrients studied. |
| Delormier and Kuhnlein, 1998 [24] | Cree communities of Wemindji and Eastmain, Quebec | n=219 FN women of three age groups 20–40; 41–60; and above 60 yrs | 24hr-food recall; FFQ |
44% of the women reported low calcium intakes (50% of the DRI††††† intake). Mean total fat intake was greater than 30% of total energy. 94% of the women exceeded the DRI for protein, and 80% exceeded the DRI for iron. | No results on pregnant and lactating FN women; lack of clinical data, limited range of nutrients studied. |
| First Nations Food, Nutrition and Environment Study [25] | 92 FN communities across Canada | n=2661 FN women of childbearing age (19-50 yrs) | 24 hr-food recall | Moderate prevalence (11%-50%) of inadequate intake was observed for vitamin C, folate, vitamin B6; high prevalence (over 50%) of inadequate intake was observed for vitamin A, D, Ca, Mg. Mean energy intakes were 1,864 kcal/day among women of aged 19-50. | No results on pregnant and lactating Indigenous women; no sub-analysis on women of childbearing of childbearing age; lack of biological data, limited range of nutrients studied. |
| Johnson-Dawn and Egeland, 2013 [26] | 7 Cree communities in Northern Quebec | n=375 FN women of child-bearing age (19-50 yrs) | 24 hr-food recall; FFQ |
Non-pregnant FN women of child-bearing age were below AMDR/EAR/AI††††† for fiber (12.3±7.3 g/day), vitamin A (554±535 RAE/day), D (6.74±10.4 μg/day), Ca (662±10.4mg/day), Mg (267±111 mg/day). Did not meet recommended Health Canada servings for Vegetable and Fruit (>90%), Grain (>70%), and Milk and Alternatives (>90%) groups. | No results on pregnant and lactating FN women; lack of biological data, limited range of nutrients studied. |
| Wahi et al., 2013 [27] | FN community in Ontario | n=300 FN pregnant women | FFQ; Clinical assessment |
No results published to date | Only analyzing blood for hemoglobin, diabetes biomarkers, and lipid profile. No micronutrient analysis of blood in protocol. |
| Waiters et al., 1998 [28] | Inuik and FN communities in NWT | n=51 Inuit, n=37 FN; n=33 CU women during pre- and post-natal periods. |
Clinical assessment of plasma 25-(OH)-D | Indigenous women had lower dietary vitamin D intake compared to non-Indigenous women (3.4±2.5 vs 5.6±4.3 μg/day; p<0.01). At the point of delivery, Indigenous women and their offspring had lower mean plasma levels of 25-(OH)-D than the non-Indigenous women (mother, 50.1±19.3 vs 59.8±29.4 nmol/L (p<0.01); offspring, 34.2±13.1 vs 41.4±23.5 nmol/L, (p<0.01)) |
Vitamin D status not representative of total nutrition status; limited range of nutrients studied; outdated report. |
| Weiler et al., 2007 [29] | Manitoba | n=183 urban Indigenous women n=26 rural Indigenous women; n=146 urban CU women. |
FFQ; Clinical assessment of serum 25-(OH)-D |
Rural and urban Indigenous women had lower serum 25(OH)D than urban white women. 32% of rural Indigenous, 30.4% of urban Indigenous, and 18.6% of urban white women were vitamin D deficient. | Pregnancy and lactation, not the focus of the study. Limited range of nutrients; clinical data only on Vitamin D. |
Table 1: Nutrition status, meal consumption and dietary patterns among Indigenous women during pre-, peri-, and post-natal periods. Studies characteristics and limitations.
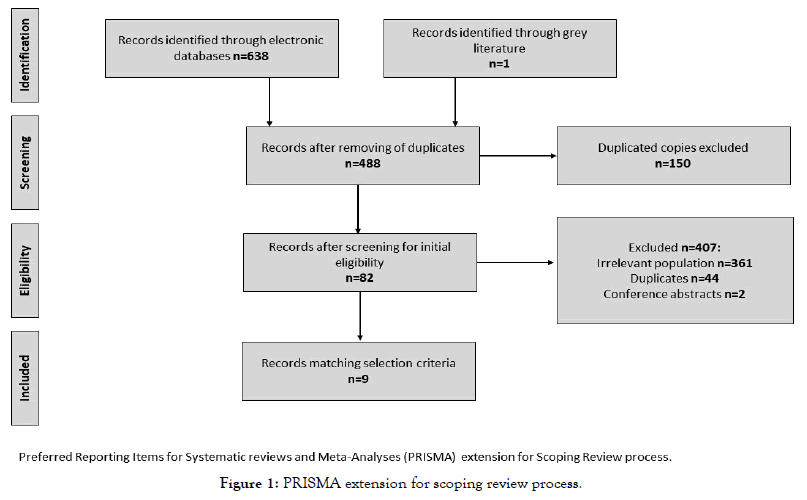
Figure 1. PRISMA extension for scoping review process.
Inclusion Criteria
All studies that had investigated a singular nutrient status, multiple nutrients status, meal consumption pattern, food group intake, and nutrition-related biomarkers with respect to First Nations women during childbearing years, pregnancy or lactation were included. No limits were placed on the demographic characteristics (income, employment status, education) of the First Nations women, pregnancy variables (gravidity and parity), and age. The limit was placed on the population, only First Nations groups (out of the three constitutionally recognized groups) were included in the review. As for the location of residence, all the studies which at-least in-part, reported on the rural and on-reserve First Nations maternal dietary information were included. Furthermore, to expand strict inclusion criteria, no restrictions were applied to whether the Indigenous communities had settled final and self-government agreements. Studies of all quantitative designs were selected for this report, encompassing epidemiological, experimental, and clinical studies.
Exclusion Criteria
Studies that focused solely on body mass index (BMI), weight, and body composition were not included in this report, as these variables do not accurately reflect the nutrient status and associated maternal morbidity. Studies that reflected only dietary attitudes, health behaviors, physical activity levels, food security status and studies on health attitudes toward body size were also excluded. All qualitative studies were also not the subject of this report. Studies that examined dietary intakes for First Nations population but did not make a specific reference or sub-analysis of prenatal or childbearing age nutrition information were excluded. The reports that investigated the nutrition status of only Metis or Inuit populations and did not focus on First Nations women were also excluded.
Data Synthesis
The titles and the abstracts for all reports were screened and reviewed by the first author followed by the senior author to determine whether the reports meet the inclusion criteria. All duplicates, irrelevant reports, and reports that did not have full-texts available were removed and only full-text reports with identified objectives, methods, and results were enlisted in this scoping review. To organize the selected reports based on the inclusion and exclusion criteria, the first reviewer created a data extraction table in Microsoft Excel. The table comprised of the information on the date of publication, authors, titles, population, methodological approaches, findings, and limitations. The extracted information in the table included details specific to this scoping review's question and objectives. The table was reviewed by the second reviewer to verify the accuracy, relevance, and any missing details.
Our search of the Canadian literature located 638 potentially relevant articles. After the examination of titles, abstracts, and reports’ bodies a total of 82 reports were isolated. Upon full examination of these reports, dismissal of duplicates, and snowballing method only 9 studies were identified that collected nutrition status information with a focus on pregnancy, childbearing age, and post-natal period of Indigenous women. Out of 9 reports introduced in this review, four reports presented data on nutritional aspects during prenatal and/or immediate postnatal periods [20-22]; four reports presented on nutrition during child-bearing age [23-25]; and one government report by the Assembly of First Nations, University of Montreal, and University of Ottawa addressed the knowledge gaps in general dietary trends in Indigenous health and environmental contaminants, including women of child-bearing age (Table 1) [25].
All of the identified studies were based in Canada and published between 1998 and 2020 [21-29], with the study by Wahi et al. [10] still expected to be published. The most prevalent methods for data collection were the 24-hour dietary recall, food frequency questionnaire (FFQ), and biological samples. Biological sampling was employed by three studies [27,28,29], of which only two had the protocol available in full text (Table 1) [28,29]. The biological sampling was performed to clinically assess only vitamin D status and did not include a full range of nutrients in the assessment. Sample sizes of participating First Nations women varied from 26 rural First Nations women in the study by Weiler et al. [29] to 2661 women residing on reserves in the First Nations Food, Nutrition, and Environment Study (FNFNES) [25,29]. While the large majority of the articles did not report data on nutritional status, some did point out the necessity of including nutritional information as an important factor in improving prenatal health of Indigenous women [23].
Nutrition Status during Childbearing Age
In total five independent studies and one government report examined nutrient intake and dietary adequacy of Indigenous women during childbearing age. Three out of these studies had a particular focus on nutrition during childbearing years [22,23,26]. The other two studies [24,29] and the report [25] included women of childbearing age in their samples, however, their objectives were not centered around prenatal nutrition. The assessments of dietary and nutrient intake were performed using 24-hour dietary recall and FFQ. One study utilized clinical assessment, however, it was only for one nutrient-vitamin D. Although, the studies were conducted in various geographic locations, similar findings were observed. They included inadequate intakes of fiber, vitamin A, vitamin D, vitamin E, folate, calcium, magnesium, and potassium [21-25]. Johnson-Dawn and Egeland [26] also reported that women were not reaching former Canada’s Food Guide (CFG) recommendations for vegetable and fruit, grain, and milk and alternative food groups. The clinical study on vitamin D demonstrated a greater prevalence of serum vitamin D deficiency among Indigenous urban and rural women (32% and 30.4% respectively) compared to urban white women (18.6%, P < 0.0004) [29].
Nutrition Status During Pregnancy and Lactation
Four studies assessed dietary intake of pregnant Indigenous women and one out of these also included cohorts with immediate postnatal periods and lactation [23,27-29]. Less uniformity was observed among prenatal reports compared to reports focused on childbearing age. One population-based, cross-sectional study collected data between 1987 and 1999 in 47 Canadian Arctic communities [23]. Assessment of nutritional “adequacy” was determined using software for comparison with average North American dietary intakes. Authors reported low intake levels of magnesium, calcium, vitamin A, C, E, and folate as well as infrequent and inconsistent maternal supplement usage. They recommended the employment of clinical dietary assessments in conjunction with dietary intake data for a more accurate depiction of the dietary status of pregnant women [21]. Although this is one of the most comprehensive studies to date, it is based on information collected 15-27 years ago, thus updates are required. A recent cross-sectional case-control study, aimed at understanding lifestyle factors that contribute to pregnancy outcomes of First Nations and Caucasian women living in rural and urban communities, found that First Nations women had a higher intake of daily cholesterol (p<0.05), a lower intake of vegetable (p<0.01), and skim milk (p<0.01) compared to Caucasian counterparts [27].
An independent Canadian study by Waiters et al. [28] reported a prevalence of vitamin D deficiency with a range of 48.4-88.6% among Aboriginal women and 15.1-63.5% among non-Aboriginal women living in the Inuvik zone of the former Northwest Territories, Canada. The study had a single-nutrient focus and did not provide a complete picture of nutritional status. Lastly, the most recent prospective study, which proposed to identify nutritional determinants of adiposity, type 2 diabetes, and related cardio-metabolic factors in Indigenous pregnant women, has not yet published their results [29].
While providing information on the aspects of nutrition status, the above studies did not address colonial contexts within which First Nations women live their daily lives. Several studies [22,24,26] and one report [25] introduced how colonial policies have changed the landscape of economic, political, and social structures of Indigenous ways of communal agriculture, tampered with roles of women in the community and dietary arrangements, however, this information was largely missing from the majority of the listed reports. Overall, the evidence of colonial impacts on maternal dietary intake is weak due to the lack of studies performed under this specific objective.
Lack of Nutrition Information
The identification of accurate nutrition status and dietary patterns for Canadian Indigenous women is impeded by the scarcity of accurate, available, and accessible information with respect to First Nations, Inuit, and Métis women. This scoping review identified only ten articles from scientific and grey literature sources that reported information on aspects of nutrition information. The majority of available studies did not focus on nutrition during pregnancy; furthermore, the range of nutrients and dietary factors explored in the few available studies was narrow and fragmented. Thus, this scoping review of the existing literature on nutrition status and dietary consumption patterns among Indigenous women residing on reserves with the focus on pregnancy and childbearing periods was limited by the insufficiency of research articles and governmental publications. Consequently, there is an urgent demand for more academic and non-academic research work, including the work with a standardized approach to the data collection of Indigenous peoples’ prenatal data in the provinces and territories. Furthermore, there is a need to build nutritionrelated information within the context of colonial history, which could have impacted the present day’s dietary patterns for First Nations pregnant women.
An additional challenge is to address the significant knowledge gaps in the national health surveys. The Canadian 2006 Maternity Experiences Survey discovered factors related to weight gain during pregnancy [30]. There was no nutritional status data obtained. Height and weight were recorded to calculate BMI [30,31]. The Canadian Community Health Survey (CCHS), a large crosssectional national survey, excluded all on-reserve Indigenous people [32]. Not only did this exclude nearly half of the overall Canadian First Nation population, but it also excluded all Indigenous peoples living in a very particular geographic, socio-economic and political Canadian reality [32]. CCHS data collected includes a 24-hour recall and some questions on vitamin and mineral supplement use. The only published results available from CCHS exclude pregnant and lactating women in the analysis [32]. Likewise, the Canadawide FNFNES, which includes First Nation peoples from 92 communities across Canada also excluded pregnant women from the project [25]. Thus, serious gaps regarding nutrition information of pregnant Indigenous women remain.
Major deficits also exist in the quality of prenatal nutrition information for First Nations, Inuit, and Métis in Canada. The most common methods for nutrition data collection presented in this review include dietary intake data through FFQ, food records, and 24-hour food recalls. While multiple recalls or food records are considered the “gold standard” for determining intake, the high cost and time required are barriers to data collection [33,34]. These methods also rely on self-reporting, which has limitations including both under and over-reporting. Evidence shows that 21.5-67.0% of participants underreport their intake while 1.0-6.0% over-report [34]. Other limitations to these methods include literacy skills, time, and the motivation required for accurate completion and lack of precision, even with the validation of self-reports [33,34]. Additionally, in Indigenous populations, the cultural aspects of food and mealtime may affect the relevancy of using a Western research tool. Therefore, nutritional biomarkers can be useful in determining a more reflective nutritional status [34]. Although, biomarkers also have their limitations due to measurement errors and the variability in biomarker levels due to genetics, metabolism, and disease status, in conjunction with intake assessments it may provide a more accurate picture of nutritional status [35].
Similar informational insufficiencies persist between maternal data in Canadian Indigenous women when compared to other Indigenous women in Australia, New Zealand, and the United States. National health surveys in New Zealand (2008) and Australian Health Surveys (2011-2013) excluded pregnant Indigenous women from their reports [36,37]. Furthermore, one of the most comprehensive national nutritional surveys in the United States –National Health and Nutrition Examination Survey (NHANES) which uses biological data to determine population nutritional status limits the option to identify ethnicity since Indigenous Americans are included under the “non-Hispanic white” or “other” categories38. This precludes the specificity of the findings as they relate to Indigenous peoples. NHANES also discontinued a supplementary sample of pregnant women after its 1999-2006 run of the survey, leaving little data regarding the nutritional status of pregnant women in the United States at al. [38].
Colonial Impacts
Prenatal nutrition presents a particular challenge in the Canadian North and in the isolated, and often impoverished communities. Although the information on remote on-reserve nutrition is scarce food security reports indicate that on-reserve households across Canada experience food insecurity at a rate more than quadruple all other Canadian households (45-100%) [39]. The relationship between maternal nutrition, health, and food security is not straightforward in the Indigenous context. Canadian colonization policies and practices have impacted maternal and child health nutrition and resulted in various kinds of nutrition-related chronic illness [40]. The policies of assimilation, colonization, residential school systems, land appropriation, language and culture loss have contributed to intergenerational trauma, and to high rates of low socio-economic status for many Indigenous peoples [13,14,15]. The colonialist policies directly resulted in impoverished foodscapes of Indigenous communities, traditional knowledge, cultural skills, including food acquisition and culinary skills limited traditional food practices [40,41]. In addition, a communication gap between Aboriginal elders and youth due to the loss of language and culture reinforced the inability to re-teach traditional skills and values, subsequently strengthening food and nutrition insecurity [40,41]. Much of the chronic disease profile with a nutritional basis – myocardial infarction mortality, obesity, type 2 diabetes, metabolic syndrome, gestational diabetes, and reduced ability to learn and other mental health problems are attributed to “a nutrition transition”, the result of moving away from nutrient-rich landbased foods to processed market foods [13,14,15,40-42].
Medicalization is another process that has greatly affected nutrition health in pregnancy as well as other matters of women’s health [43]. Medicalization regards a systematization of health knowledge, an appropriation of women’s traditional knowledge by medical experts, that is, a replacement of one set of knowledge principles, which are accessible by self-governing agents in everyday life, into the hands of an expert, professional class of individuals. Besides a change in the knowledge expertise, medicalization involves a physical relocation of pregnant women away from their homes to the southern medical catchment areas [43]. This is done without the involvement of Indigenous women and communities in the health systems planning and services implementation. These political forces re-shaped identities, re-designed women’s bodies from those thriving in ecologies to one’s in deficit [41,43].
Befitting with the clearly stated Indigenous policies and initiatives regarding the necessity of Indigenous authority in the governance and directorship of Indigenous health information, improving Indigenous maternal nutritional health requires an evolving collaboration between Indigenous and non-Indigenous governmental organizations. Furthermore, respectful partnerships with the stakeholders and public health units at the national, provincial, and territorial levels need to be built to address maternal and child health nutrition issues faced by Indigenous women [41]. Such collaboration initiatives are critical to the development of standardized assessment strategies and effective, evidence-based policy and programming to attenuate maternal nutrition-related chronic ailments for First Nations women. Based on the finding of this scoping review the recommendations for further action include:
o In partnership with regional, provincial, national, and Indigenous public health units and organizations develop standardized maternal nutrition surveillance systems that accurately identify nutrition information for all Indigenous groups.
o Develop policies and programs that deliver the concentrate on the tailored prevention of nutrition-related chronic diseases during pre-, peri-, and post-natal periods of women’s lives;
o Enhancements of prenatal nutrition research by collecting thorough information employing a variety of available methods including biological sampling to produce the utmost accurate results;
o Research on nutritional status must not only focus on nutrition from the biological perspective, but also from the health promotion and social justice perspective, taking into account the historical context and social determinants of health of Indigenous peoples. This should be done ethically and through participatory health research with Indigenous communities.
o Assess other Indigenous groups (Metis and Inuit) to synthesize and identify the state of evidence pertaining to maternal nutritional health.
o Assess nutritional status of First Nations women in the context of colonial landscape and its economic, political and social impacts, which transformed the traditional ways of dietary habits for Indigenous population.
A major strength of this review was the use of a clear and rigorous systematic review protocol (PRISMA) to identify all relevant articles in regard to Indigenous maternal nutrition status and dietary patterns. This protocol helps to improve methodological transparency and allows for succeeding replication. Another significant strength of this review was the establishment of an objective baseline regarding Indigenous maternal nutrition. This information is particularly advantageous for developing maternal programs as well as when evaluating the research contribution and program success over time.
This comprehensive review retained a strict focus on the maternal nutrition for First Nations groups residing on the reserves and remote communities. There is a clear propensity of Indigenous health literature to focus on the broad population groups such as pan-Indigenous, Canadian Arctic, and Canadian northern populations [30,33,42,44]. These approaches do take into account distinct jurisdictional and health policy mechanisms, off- and onreserve locations, various Indigenous world views and languages. Consequently, maternal nutrition status and dietary habits for individual Indigenous groups remain largely unknown. This review aimed to, in-part, cover this gap, by focusing on one of the Indigenous groups. Furthermore, this review built on the synthesized evidence and generated practical and evidence-based policy recommendations to improve maternal nutritional health for First Nations women in Canada
There were a number of limitations that emerged as a result of a lack of available reports on Indigenous maternal nutrition. Due to a remarkable lack of information, we were not able to comprehensively and comparably synthesize the evidence on maternal nutritional status and dietary intake for First Nations women residing on reserves and in remote communities.
Another limitation of this review is the diversity in methodological approaches to measuring nutrient status. The methodological approaches such as research tools, sampling methods, inclusion and exclusion criteria, and analysis methods were dissimilar between the reports (Table 1). The range of methodological inconsistency hinders the ability to perform a rigorous meta-analysis and arrive at significant and meaningful interpretations. In addition, lack of biological data analysis leads to an inability to objectively state present nutrient status.
Another potential limitation of this review is the lack of focus on other constitutionally recognized Indigenous groups such as Metis and Inuit. These groups were excluded to preserve the homogeneity of the population selected for this review and deliver a clear appraisal of the evidence available for First Nations populations
This systemic review summarized the limited data available on parental nutrition information for Indigenous women residing on reserves. Major gaps in prenatal nutrition information exist, as research studies are fragmented, focused on a limited amount of nutrients, and lack relevant novel information. Furthermore, nutrition research often excludes pregnant Indigenous women, as most nutrition studies do not include both objective data (biological) and food intake patterns. These research gaps must be filled for nutritional interventions and prenatal health programs and policies to be sufficiently informed and effective. Ultimately, improving nutritional status information will contribute to improving maternal and child health for Indigenous women in Canada. The information acquired from this scoping literature review should be employed in the development and facilitation of community nutrition research, which will allow for future construction of the nutrition information capacity. Additionally, in-light of Indigenous lead health transformation and self-determination initiatives the information in this review may be utilized as a strategic mechanism for equitable maternal and child health services planning in First Nations communities.
None of the authors have any conflict of interest to declare
Citation: Kloss O, Dyck K, Giesbrecht H, Eni R, Eskin MNA, et al. (2021) A Scoping Literature Review of the Nutrition Status Among Canadian First Nations Women During Pregnancy: What Does the Evidence Reveal?. Fam Med Med Sci Res.10:286. doi:10.35248/2327- 4972.21.10.286.
Received: 18-May-2021 Accepted: 19-Jul-2021 Published: 26-Jul-2021 , DOI: 10.35248/2327-4972.21.10.286
Copyright: © 2021 Kloss O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.