Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2020)Volume 11, Issue 3
Aim: To report a clinical case of 15 years old girl, with low visual acuity in her left eye.
Methods: This case report is a retrospective and descriptive study. Data was gathered from patient clinical record file
that included anamnesis, examination and analysis of diagnostic tests.
Results: A 15 years old female complains of low visual acuity in her left eye (LE), for the last three weeks, before
consultation. Her father and grandmother had low visual acuity since young age not correctable with glasses. Best
corrected visual acuity was 6/6 in the right eye and 6/36 in the left. Both eyes anterior segment examination was
normal. Bilateral posterior segment exam revealed yellow colored material similar to yolk egg structure, on the
macula. The macula optical coherence tomography (OCT) reveled RE pigmentary epithelial detachment (PED) and
LE atrophic scar. Fluorescein Angiogram (FFA) showed active choroidal neovascular membrane (CNVM) in the LE.
For treatment of the CNVM in left eye it was given Intra vitreous Ranibizumab injection once. On the sixth and
twelfth months review the visual acuity, FFA and macula examination were stable. Routine blood investigation,
physician consultation not found any abnormality.
Conclusion: The family history, clinical findings, OCT and fluorescein angiogram features were characteristic of Best
Vitelliform Macular Dystrophy.
Bilateral posterior; Fluorescein Angiogram; Optical coherence tomography
To report a clinical case of 15 years old girl, with low visual acuity in her left eye.
This case report is a retrospective and descriptive study. Data was gathered from patient clinical record file that included questionnaire, examination and analysis of diagnostic tests.
Best disease, also termed vitelliform macular dystrophy, is typically an autossomal dominant disorder, which classically presents in childhood with the striking appearance of a yellow or orange yolk like lesion in the macula. Dr Franz Best, a German ophthalmologist, described the first pedigree in 1905 as a genetic form of macular degeneration. This condition affects either women or men.
Best vitelliform macular dystrophy is a rare disorder, with prevalence of about 1 in 10,000 individuals and slowly progressive. It usually occurs in both eyes but, it may not affect vision to the same extent in each of them. Though, sometimes it attacks one eye, only. This disorder strikes the retina, disrupting cells in the macula.
Best disease is inherited in an autosomal dominant pattern. In most cases, an affected person has one parent with the condition. It represents a genetic form of macular degeneration without specific treatment that occurs in about 1 in 10,000 individuals.
15 years old girl seen at Dr Agarwal Eye Hospital in Mozambique, Maputo in 2018 with low vision on LE thathad three weeks before the consultation. Family history father grandmother low vision since childhood not improving with glasses. No history of glasses general symptoms referred. The acuity test details are provided in Table 1.
| Eye | Not corrected vision | Corrected vision |
|---|---|---|
| Right | 43991 | -0.50/-0.50 × 90° =6/6 |
| Left | 13302 | Not improvement |
Table 1: Patient’s Snellen visual acuity test.
Slit lamp examination revealed unremarkable findings in the anterior segment of both eyes. Posterior segment exam, at the macula, showed a well circumscribed yellow material similar to the egg yolk structure, in both eyes (Figure 1). The optical coherence tomography (OCT) macula revealed pigmentary epithelial detachment (PED) and LE atrophic scar. Fluorescein Angiogram (FFA) showed an active choroid neovascular membrane (CNVM) on the LE, also. The systemic examination had no remarkable findings. The patient was diagnosed Best Vitelliform macular. For the treatment of the CNVM on left eye it was given Ranibizumab Intra vitreous injection once. Review of visual acuity was done on six and twelve months later review the visual acuity, and macula examination were stable.
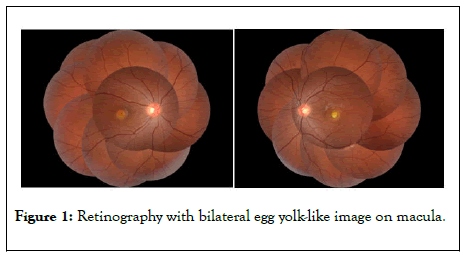
Figure 1: Retinography with bilateral egg yolk-like image on macula.
This might be the first case of Best disease described in Mozambique, to the best knowledge of the authors. The German Ophthalmologist Best, in 1905, first described this hereditary macular dystrophy [1]. It is rare, occurring in about 1 in 10,000 individuals. There has been one case described in Nigeria, Africa. Also, it has been found in African-Americans associated with sickle cell anemia trait [2]. Besides, it has been diagnosed in Caucasians and Asians, also [2].
The BVMD is an autosomal retinal dystrophy caused by heterozygous mutations of bestropin 1 gene [3]. The associated clinical macular changes usually begins in childhood before it gets clinically apparent. However, even during the earlier stages eye fundus examination evidence egg yolk like lesion [4] (Figure 1).
The diagnosis of Best vitelliform macular dystrophy is based on fundus appearance, electrooculogram (EOG), and family history. On the electro-oculogram (EOG) is always abnormal, showing a severe loss of the light response [5-8]. Tests like fluorescein angiogram and optical coherence tomography are also useful in the diagnosis revealing disturbance of Retinal Pigmentary Epithelium (Figures 2 and 3).
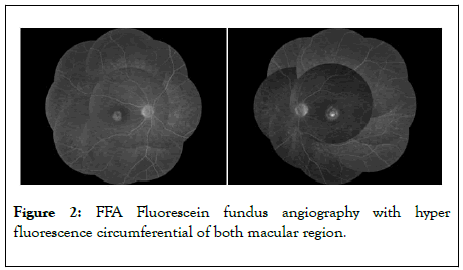
Figure 2: FFA Fluorescein fundus angiography with hyper fluorescence circumferential of both macular region.
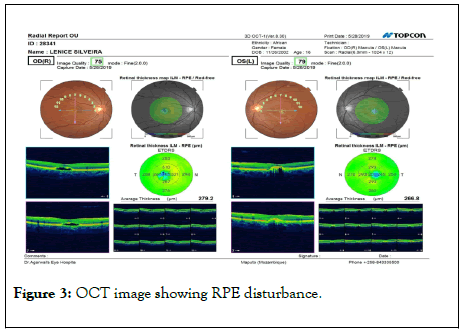
Figure 3: OCT image showing RPE disturbance.
The case report describes a patient bearing Best disease in Mozambique. Given the autosomal dominant hereditary pattern eye fundus exams to other family members were recommended.
Citation: Buquea A, Vankawalaa S, Hussaina R, Dudhatraa M, Manhicab G (2020) A Clinical Case Report: Best Vitelliform Macular Dystrophy Disease, Mozambique. J ClinExpOphthalmol. 11:839. DOI: 10.35248/2155-9570.20.11.839
Received: 27-Apr-2020 Accepted: 11-May-2020 Published: 18-May-2020 , DOI: 10.35248/2155-9570.20.11.839
Copyright: © 2020 Buquea A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.