Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2020)
A 23-year-old woman from Bangladesh presented with a 6-week history of spiking fevers, myalgias, arthralgias, pruritic rash, marked granulocytosis and lymphadenopathy. On presentation to the emergency department she had brown lichenified plaques on the upper chest and neck; her back had flagellate-like erythema. Hand exam revealed hyperpigmented papules over the metacarpophalangeal joints without periungual capillary loop dilatation. Labs were notable for: minimally positive ANA (1:40), mild transaminitis (AST 56, ALT 73), as well as elevated aldolase (13.8), LDH (1,368), sedimentation rate (>140), C reactive protein (7.5) and ferritin (10,248). She also had a negative Anti Jo1 antibody, rheumatoid factor, and CK (<20). An extensive infectious workup was negative. CT of the chest/ abdomen showed generalized lymphadenopathy with mild splenomegaly. Punch biopsies from the hands and back revealed multiple necrotic keratinocytes mainly in the upper epidermis and within parakeratotic stratum corneum, infiltration of lymphocytes and neutrophils in the papillary and mid dermis and numerous intradermal eosinophils without evidence of vasculitis. In the setting of meeting original Yamaguchi criteria for Adult Onset Still’s Disease (AOSD), negative infectious workup, constellation of lab and imaging findings and characteristic histopathologic findings, the patient was diagnosed with atypical AOSD. She was treated with systemic steroids and had resolution of her symptoms. Atypical presentations of AOSD clinically mimicking dermatomyositis show a distinguishing pattern on histology: dyskeratotic and necrotic keratinocytes in the upper layers of the epidermis, inflammatory infiltrate in the upper and mid dermis, and no evidence of vasculitis, as seen in this patient.
Atypical AOSD; Histopathology; Necrotic keratinocytes
Adult onset Still’s Disease (AOSD) is a rare, acute, systemic inflammatory disease, with unexplained cause, that is characterized by a set of symptoms, including high spiking fevers, typical evanescent rash, arthralgias and/or arthritis, sore throat, lymphadenopathy, abnormal liver functions, and splenomegaly [1]. AOSD is a part of a broad differential, and considered a diagnosis of exclusion, and should be made when causes such as infection, cancer, or other autoimmune diseases are ruled out [2]. Laboratory findings suggestive of AOSD include granulocytosis and hyperferritinemia, but dermatologists often look for a typical nonpruritic salmon pink-colored evanescent papules or macules when making a diagnosis. However, recent literature has reported several cases of AOSD presenting with unique cutaneous manifestations that with an already broad differential, make the diagnosis especially challenging. Here we will discuss our unique case presentation, and briefly review other atypical cutaneous manifestations that have previously been associated with AOSD and contributed to delayed diagnosis, together with histopathologic findings that aid in differentiating between the diagnosis.
A 23-year-old woman from Bangladesh presented with 6 weeks of spiking fevers, myalgias, arthralgias, pruritic rash, sore throat, marked granulocytosis, and lymphadenopathy. The rash was preceded by the symptoms of arthralgia and myalgia. She was previously seen by multiple providers and treated with a course of steroids and several different antibiotics that helped only temporarily.
Physical exam demonstrated neither upper nor lower extremity weakness. On skin examination she had brown lichenified plaques on the upper chest and neck (Figures 1 and 2); her back had flagellate-like erythema (Figure 3). On hand examination, she had hyperpigmented papules over the metacarpophalangeal joints (Figure 4) without periungual capillary loop dilatation. She had mild periorbital hyperpigmentation (Figure 5). The patient reported pruritus.
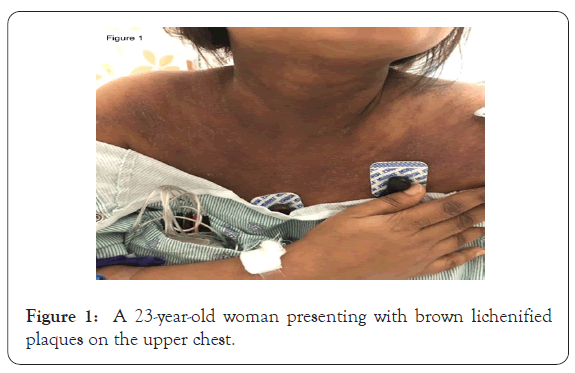
Figure 1: A 23-year-old woman presenting with brown lichenified
plaques on the upper chest.
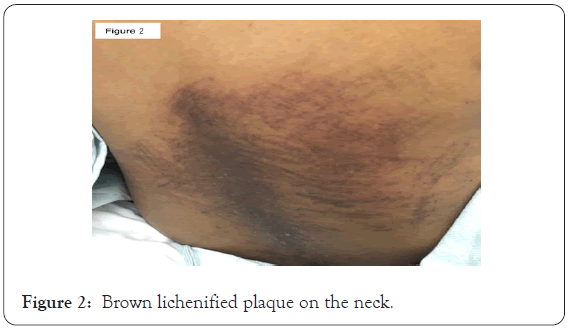
Figure 2: Brown lichenified plaque on the neck.

Figure 3: Flagellate-like erythema on the back.
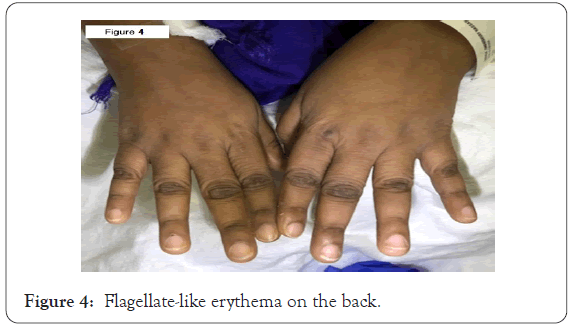
Figure 4: Flagellate-like erythema on the back.
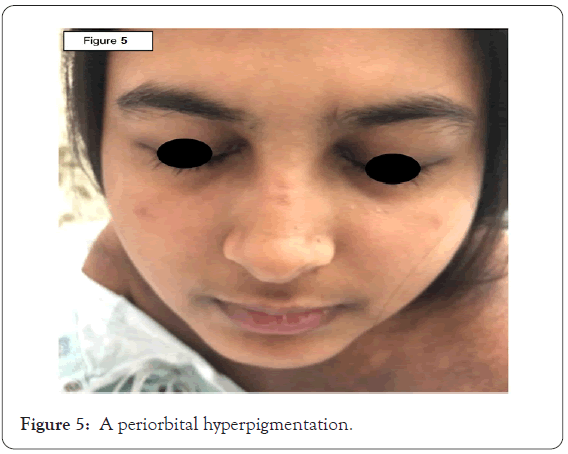
Figure 5: A periorbital hyperpigmentation.
Labs were notable for erythrocyte sedimentation rate of greater than 140 mm/h, elevated C-reactive protein of 7.5 mg/L, mild transaminitis of AST 56 unit/L and ALT 73 unit/L, elevated alkaline phosphatase of 211 unit/L, low hemoglobin of 5.9 g/dL, low hematocrit 18.4%, low MCV of 78.1 fL, white blood count of 10,400 cells/μL with bandemia of 6% and eosinophilia of 5%, elevated ferritin level of 10,248 ng/mL, mildly positive antinuclear antibody of 1:40 titer, elevated aldolase of 13.8 units/L, elevated LDH of 1,368 units/L, negative rheumatoid factor (RF), negative Anti Jo1 antibody, normal complement levels and normal CK of less than 20 units/L. We did not test for myositis-specific and associated antibodies against SRP, Mi2, PL7, PL12, EJ, OJ, Ro52, Ku, Pm-SCl 75, and PM-Scl 100. An extensive infectious workup including bacterial, viral and parasitic serology was broadly negative.
CT of the chest/abdomen showed hilar, subcarinal, and axillary lymphadenopathy with mild splenomegaly. MRI of the right femur revealed bilateral nonspecific inguinal lymph nodes but was negative for myopathy.
Initial differential diagnosis included dermatomyositis, AOSD, hemophagocytic syndrome, and lymphoma/paraneoplastic syndrome. Dermatomyositis was initially the favored diagnosis given the apparent shawl and V signs on the chest, heliotrope rash, and myalgias proximally greater than distally. However, the patient did not have other dermatomyositis features including capillary loop dilatation and an essentially negative rheumatologic work up. Hemophagocytic syndrome was considered in the setting of a rash, significant anemia, high alkaline phosphatase, and lymphadenopathy.
Punch biopsies from the hands and back revealed multiple necrotic keratinocytes mainly in the upper epidermis and within parakeratotic stratum corneum, infiltration of lymphocytes and neutrophils in the papillary and mid dermis and numerous intradermal eosinophils without evidence of vasculitis (Figures 6 and 7). Muscle biopsy was not performed and thus the European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) classification was not utilized to assess for adult and juvenile idiopathic inflammatory myopathies and their major subgroups [3].
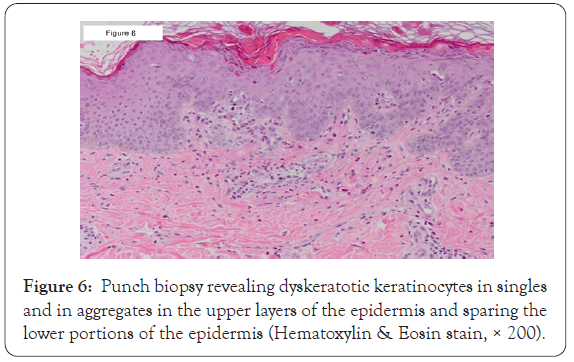
Figure 6: Punch biopsy revealing dyskeratotic keratinocytes in singles and in aggregates in the upper layers of the epidermis and sparing the lower portions of the epidermis (Hematoxylin & Eosin stain, × 200).
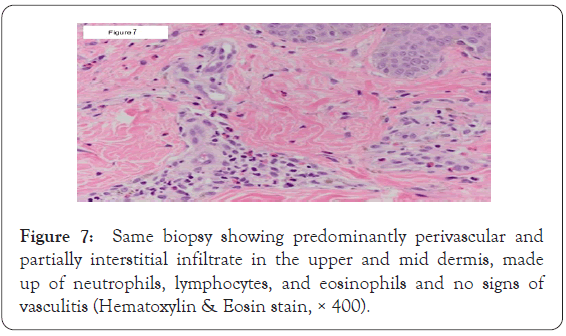
Figure 7: Same biopsy showing predominantly perivascular and partially interstitial infiltrate in the upper and mid dermis, made up of neutrophils, lymphocytes, and eosinophils and no signs of vasculitis (Hematoxylin & Eosin stain, × 400).
In the setting of a negative infectious workup, laboratory and imaging findings meeting original Yamaguchi criteria for adult onset Still’s disease (AOSD) [4], and a biopsy excluding dermatomyositis, as well as, characteristic for atypical AOSD, a diagnosis of atypical AOSD was made and the patient was treated with prednisone, 1 mg/kg/d, with resolution of her symptoms. She was subsequently continued on a daily prednisone 30 mg per rheumatology recommendations, and it was considered to start Anakinra for long term therapy. A lymph node biopsy and exclusion of a malignancy was planned by hematology/oncology; however, the patient was lost to followup. On follow-up with dermatology, her skin lesions resolved with only residual post-inflammatory pigmentary alterations. Originally planned direct immunofluorescence for ultimate dermatomyositis exclusion was aborted as skin lesions were no longer evident on the exam. At the time of submission of this manuscript months later, the patient continued regular follow-up with rheumatology and remained stable on a daily oral prednisone dose of 2.5 mg, with consideration given to initiate Anakinra.
A diagnosis of adult onset Still’s disease is made upon exclusion of all other potential diagnoses. The patient needs to meet a combination of the Yamaguchi criteria [4], particularly 5, with at least 2 being the major criteria. Major criteria are the following: fever for 1 week or longer, arthralgia for 2 weeks or longer, typical macular or papular nonpruritic salmon-pink evanescent rash, and granulocytic leukocytosis (≥ 10,000/μL). Minor criteria are the following: sore throat, hepatomegaly or splenomegaly, lymphadenopathy, liver function abnormalities, and negative RF and ANA.
Non-classical cutaneous findings are challenging to dermatologists and delay a correct diagnosis in a timely fashion. Recently, several reports have described such challenges revolving around atypical skin presentations, the most common ones being persistent papules and plaques [5,6]. Other less frequent presentations include lichenoid papules, dermatographism-like, lichen amyloidosislike, prurigo pigmentosa-like, urticarial eruptions, generalized nonpruritic erythema, and eyelid edema [7-9]. The non-classical cutaneous findings can be seen before, during, or after the typical evanescent rash, or could be the only finding on the skin exam [9]. The less frequent skin findings may present differently on histopathology, but the most common atypical cutaneous manifestation of persistent pruritic papules and plaques seems to have a consistent presentation - dyskeratosis localized to the upper layers of the epidermis and a scarce superficial dermal infiltrate including scattered neutrophils [10]. Lee et al. [11] described 9 patients presenting with the atypical presentation of AOSD in the form of persistent plaques and linear pigmentation with histopathologic findings consistent with previous observations – numerous individual necrotic keratinocytes in the upper epidermis and scattered neutrophilic infiltrate in the dermis. This histopathologic finding is not usually seen in AOSD mimickers including dermatomyositis. Typical skin biopsy in dermatomyositis demonstrates apoptosis of epidermal basal and suprabasal cells with epidermal atrophy, epidermal basal cell vacuolar degeneration, and increased mucin deposition in the dermis [12].
Our patient presented with a constellation of clinical findings consistent with inflammatory myositis, including the typical shawl and V signs, heliotrope rash, and myalgias predominantly affecting proximal upper and lower extremities, which initially raised our clinical suspicion for dermatomyositis or other connective tissue disease. However, other symptoms including spiking fevers, arthralgias, sore throat, marked granulocytosis and lymphadenopathy, as well as, absent capillary loop dilatation, and a negative laboratory and imaging work-up were in favor of AOSD. One of the distinctive features of AOSD-related arthritis is carpal ankylosis, which results in a limited range of motion in the carpal joints. Our patient suffered from arthralgia but exhibited no obvious arthritic deformities; obtaining and X-ray of the hands and wrists could have demonstrated the aforementioned findings.
Although our patient did not have a typical nonpruritic salmon-pink evanescent rash, several cases of atypical cutaneous manifestations of AOSD have recently been reported, including the pruritic persistent papules and plaques [9]. Further, our case showed histological features of Still’s disease such as dyskeratotic and necrotic keratinocytes in the upper layers of the epidermis, inflammatory infiltrate in the upper and mid dermis, and no evidence of vasculitis [9], as seen in this patient, which ultimately helped establish the diagnosis.
Atypical AOSD was previously regarded as a disease that could be associated with delayed malignancy [7] and certain viral infections including echovirus, rubella, and Epstein Barr virus [13]. Our patient had a negative viral work-up including the viruses mentioned above, and was planned for further evaluation with biopsy of the enlarged lymph nodes to exclude a paraneoplastic process due tos a potential underlying malignancy. She was lost to follow-up with hematology/oncology and lymph node and bone marrow biopsies were never performed. That said, the possibility of malignancy was not completely excluded. However, the patient continued to follow with her primary team (rheumatology) and dermatology, and remained stable and in good general health while on the same treatment regimen; this makes malignancy a less likely diagnosis. Further, non-classical lesions are most often present in persistent and more severe AOSD cases that are associated with several complications, including reactive hemophagocytic syndrome [9], which was observed in our patient.
As discussed previously, several cases of atypical cutaneous manifestations of AOSD have been reported in the literature but the data on atypical presentation of AOSD remains scarce. Our case is an addition to this recently expanding literature on atypical presentations of AOSD and further supports previous rare notions that in adults with Still’s disease, a typical nonpruritic evanescent rash may be absent, and persistent pruritic papules and plaques can be seen instead. Further, the current case emphasizes the importance of obtaining a biopsy of the skin lesions to distinguish between the overlapping diagnoses.
Conclusively, clinicians and dermatopathologists should be aware that dermatomyositis and other connective tissue disorders can clinically mimic AOSD especially in the absence of a typical rash, should remain highly suspicious for AOSD, and obtain biopsies in order to efficiently arrive at a correct diagnosis, as these cases usually require more aggressive treatment.
None to declare
None to declare
Citation: Egger A, Rosenberg M, Price A, Cho-Vega JH (2020) A Challenging Case of Atypical Adult Onset Still’s Disease Clinically Mimicking Dermatomyositis with Distinctive Histopathologic Findings. J Clin Exp Dermatol Res. 11:540.
Received: 30-Oct-2020 Accepted: 13-Nov-2020 Published: 20-Nov-2020
Copyright: © 2020 Egger A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.