Annals and Essences of Dentistry
Open Access
ISSN: 0975-8798, 0976-156X
ISSN: 0975-8798, 0976-156X
Research Article - (2021)Volume 13, Issue 6
Aims: The aim of this study was to compare the clinical results of conventional non-surgical periodontal therapy with or without adjunct PDT in patients of chronic periodontitis.
Materials and methods: 20 patients with chronic untreated periodontitis, (8 female, 12 male, mean aged: 36.35 years, all non-smokers, systemic diseases, including anti-inflammatory, blood stimulants, or systemic antibiotics, within the last 6 months were exempted from the criteria, previously untreated chronic periodontitis; in any quadrant at least 1 premolar and 1 molar with at least 4 teeth each; in each quadrant at least 1 tooth with an attachment loss of >3 mm were included in the study. The periodontal status of each subject was evaluated at baseline and 6 weeks following periodontal therapy. PDs, Clinical Attachment Level (CAL) were assessed.
All patients received non-surgical periodontal treatment comprising a thorough scaling and root planing of all periodontally involved teeth using a split-mouth design, two quadrants were additionally treated with PDT, with a designated photosensitizer dye (methylene blue) and a diode laser (biolase 940 nm). Laser application at six locations per tooth was carried out circumferentially. The subjects were given thorough oral hygiene maintenance instructions and recalled after two weeks for a second round of PDT at the same sites. A total of two exposures for the photodynamic therapy group with a two week interval were done Probing depths and attachment levels were assessed after 6 weeks. Statistical analysis was done to compare intergroup using the paired t-test. Differences were considered as statistically significant at p<0.05.
Results: Baseline mean values for PD and CAL were significantly different in the test and control group. Values for CAL and PD decreased significantly 6 weeks after treatment in the control group, with a higher impact on the sites treated with adjunctive PDT
Conclusion: In patients with untreated chronic periodontitis, clinical outcomes of conventional non-surgical periodontal therapy can be improved by multiple PDT.
Diode laser; Photodynamic therapy; Non-surgical periodontal therapy
Periodontitis is caused by inflammation of the supporting teeth structure and by various periodontopathic bacteria in response to chronic infections, respectively. Current concepts are based on mechanical scaling and root planning to remove bacterial deposits, cementum contaminated with the bacteria and endotoxins in the treatment of periodontally involved teeth. However in sites where the mechanical scaling and root planning are difficult to access the removal of plaque and the reduction of the number of infectious cells. In cases which do not respond to conventional treatments, certain therapeutic alternatives, such as systemic and local antibiotics have been used [1]. Laser-assisted periodontal therapy has recently gained popularity as a possible replacement or complement to traditional mechanical debridement. CO2 laser, Neodymium Doped: Yttrium- Aluminium-Garnet (Nd:YAG) laser, and diode and Erbium- Doped: Yttrium-aluminium-Garnet (ER:YAG) laser (Er:YAG) Laser have been used in periodontal pocket therapy for both hard and soft tissue treatment.
During irradiation, some of the laser energy scatters and penetrates into periodontal pockets. The low-energy attenuated laser can then stimulate the cells of the surrounding tissue, reducing inflammatory conditions in cell proliferation and increasing lymph flow, improving periodontal tissue attachment and probably reducing postoperative pain. The wavelength of a diode laser is 810 nm or 910-980 nm, which has no effect on dental hard tissues. As a result, the laser is an ideal soft tissue surgical laser that can be used to cut and coagulate gingiva and oral mucosa, as well as for soft tissue curettage and sulcular debridement [2]. It has a bactericidal effect as well. PDT is the light energy process used to activate a photo sensitizer in the presence of oxygen. The principle of operation is that the photosensitizer undergoes a transition to a higher energy condition that produces highly reactive oxygen conditions. This oxygen alone could cause microorganisms toxicity. A number of photo senses against target microorganisms have proved to be effective without damaging the host tissues [3].
PDT can be effective in killing bacteria like Porphyromonas gingivalis or Fusobacterium nucleatum in vitro which are periodontopathogens. The photo sensitization of P. gingivalis was demonstrated by using an animal model in vivo, which resulted in a decrease in bone loss. In a model of the Beagle dog, inflammatory signs were positive and P. gingivalis could be suppressed. Similar clinical results have been shown in the evaluation of PDT's impact on the treatment of human aggressive periodontitis, photosensitisation and SRP. The comparison of conventional debridement with or without the additional use of PDT in chronic periodontitis showed improved clinical parameter improvement in the PDT group [4]. This study was intended to compare the clinical results of conventional non-surgical periodontal therapy with or without adjunct PDT in patients of chronic periodontitis by testing for non-surgical periodontal therapy hypothesizing that incorporating that PDT as an adjunct could improve clinical outcomes.
Patient selection
20 patients, each of whom presented chronic untreated periodontitis, were recruited from the outpatient Department of periodontics and oral implantology, Saveetha Institute of Medical and Technical Sciences, Chennai (8 female, 12 male, mean aged: 36.35 years, all non-smokers).
Exclusion criteria
Systemic diseases, including anti-inflammatory, blood stimulants, or systemic antibiotics, could influence periodontal therapy outcomes within the last 6 months were exempted from the criteria [5].
Inclusion criteria
The study included the following: Previously untreated chronic periodontitis; in any quadrant at least 1 premolar and 1 molar with at least 4 teeth each; in each quadrant at least 1 tooth with an attachment loss of >3 mm.
Informed consent
All patients were informed of the study and a written and video consent was taken prior to the trial in the period from December 2020 to February 2021, to participate in the study for 6 Weeks. The study was carried out in full conformity with the declared ethical principles approved by the Ethics Committee of the University.
Clinical parameters
The periodontal status of each subject was evaluated at baseline and 6 weeks following periodontal therapy. A blind examiner, who was not involved in the study of patients, documented the PDs, Relative Attachment Level (RAL), degree of tooth mobility, and furcation involvement. An experienced periodontal examiner conducted all measurements allowing intraexperimental value comparison. The upper and lower teeth have been recorded by taking impressions followed by the fabrication of personalised splints fitting with the teeth. These splits were used to provide both PD and relative attachment status with reproducible measurement points. Thus, the individual splints were produced by a vacuum-forming process for each subject. Only short of tooth emergence was trimmed. A groove was created in the splint for each studied site and a line for the calibrating pressure periodontal probe was formed to facilitate a reproducible sensor position during measurements [6].
Treatment procedure
All patients received non-surgical periodontal treatment comprising a thorough scaling and root planning of all periodontally involved teeth employing both hand instruments and a piezo-electric ultrasonic headpiece with a slim-line styled scaler tip (Woodpecker) by the same clinician. Using a splitmouth design, two quadrants (test group) were additionally treated with PDT. Therefore, after periodontal debridement, the quadrants were assigned to different groups according to a randomised lot picking technique. The sequence was concealed until interventions were assigned. In combination with a designated photosensitizer dye (methylene blue) the PDT was performed by a diode laser (biolase 940 nm). Periodontal pockets have been rinsed from the bottom of the pocket using the photosensitizer and the blunt cannula to complete the pocket filling and roots coating [7].
The pockets were rinsed with water for excess photosensitizer after 3 minutes of residence time. The remaining photo sensor was activated for 10 s per site using the laser probe. Laser application at six locations per tooth was carried out circumferentially. The subjects were given thorough oral hygiene maintenance instructions and recalled after two weeks for a second round of PDT at the same sites. A total of two exposures for the photodynamic therapy group with a two week interval were done Probing depths and attachment levels were assessed after 6 weeks [8].
Statistical analysis
For statistical analysis IBM SPSS version 23 (SPSS Inc., Chicago, IL, USA). Comparison within the groups with respect to the treatment intervals were performed using the paired t test. Differences were considered as statistically significant at p<0.05.
Probing depths
Baseline PDs of periodontally involved teeth were statistically significant in the test group and control group (p<0.05).
Six weeks after treatment, in both groups, a decrease in PDs could be found (p<0.05) with a higher impact in the test group than in the control, with a higher impact on the sites treated with adjunctive PDT (p<0.05) (Table 1).
| Mean | Significance | ||
|---|---|---|---|
| Group 1 | PD before | 6.70 ± 1.081 | 0 |
| PD after | 4.55 ± 1.146 | ||
| CAL before | 8.30 ± 1.218 | 0 | |
| CAL after | 6.65 ± 1.137 | ||
| Group 2 | PD before | 6.92 ± 1.112 | 0 |
| PD after | 5.95 ± 1.192 | ||
| CAL before | 9.12 ± 1.256 | 0 | |
| CAL after | 8.46 ± 1.127 |
Table 1: Depicts statistical analysis for pre and post intervention for adjunctive photodynamic therapy in both groups; with and without photodynamic therapy.
Clinical attachment level
The attachment levels of periodontally involved teeth did not differ significantly in the test group and control group at baseline (p<0.05).
After 6 weeks, a lower attachment gain could be observed in the control group than in the test group (p<0.05).
Comparing the differences in CAL, an attachment gain could be observed in both groups, with a higher impact on the sites treated with adjunctive PDT (p<0.05) (Figures 1 and 2).
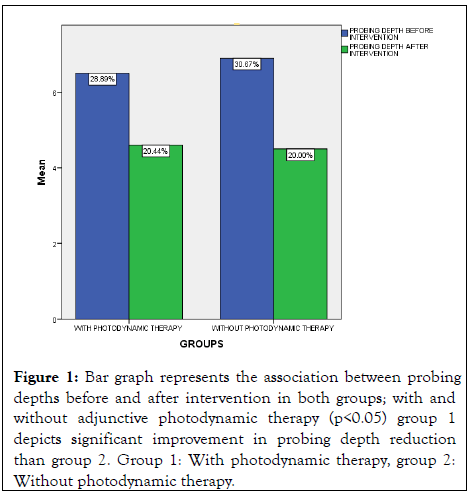
Figure 1: Bar graph represents the association between probing depths before and after intervention in both groups; with and without adjunctive photodynamic therapy (p<0.05) group 1 depicts significant improvement in probing depth reduction than group 2. Group 1: With photodynamic therapy, group 2: Without photodynamic therapy.
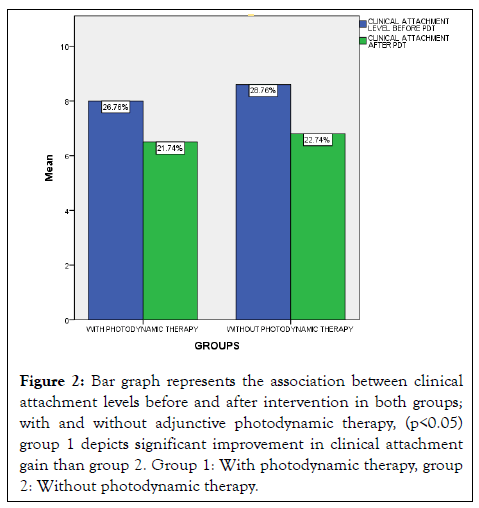
Figure 2: Bar graph represents the association between clinical attachment levels before and after intervention in both groups; with and without adjunctive photodynamic therapy, (p<0.05) group 1 depicts significant improvement in clinical attachment gain than group 2. Group 1: With photodynamic therapy, group 2: Without photodynamic therapy.
This study demonstrates that PDT procedures improved the clinical results for the non-surgical periodontal treatment of chronic periodontitis. The conventional mechanical device of the root is seen as a prerequisite for success in the long term. Studies could, however, indicate that an additional benefit in the treatment of chronic periodontitis may come from adjunctive treatment processes like minocycline or laser radiation. The Er:YAG laser is a new technique for sub gingival debridement [9]. The residual calculus after laser irradiation can be demonstrated to depend on the fluorescence threshold level, without removing a relevant quantity of the root cementum. As to the microbiological results, Er:YAG laser, curettes, sonic and ultrasonic scalers have the same effects in chronic periodontitis patients. Full mouth treatment concepts are another attempt at improved periodontal therapy to avoid early re-infection in untreated areas. Disputable data on microbiological effects of full mouth non-surgical periodontal therapy compared to the normal quadrant approach have been reported. A recent study has not confirmed any re-colonization differences after SRP for 24 hours compared to treatments during several sessions [10].
In current literature, only minor differences in treatment effects among these treatment strategies were observed among adults with chronic periodontitis. A systematic antibiotic constituent in the long-term management of periodontal diseases provides significant clinical benefits from the sub antimicrobial dose doxycycline therapy as an addition to SRP. However, the use of this therapy in addition to non-surgical periodontal debridement among smokers could not be demonstrated. In periodontal therapy systemic antimicrobials should be an adjunct to mechanical debridement. These results validate the search for new methods of treatment to improve conventional debridement. The limited access to plaque by topical agents and the development of antibiotic resistance make alternative strategies necessary in order to control the use of biofilms and treat periodontal diseases. PDT is mediated by singlet oxygen, which affects extracellular molecules directly [11].
Polysaccharides present also have photo damage potential within the extracellular matrix of the polymers in a bacterial biofilm. Such dual activity is not antibiotic-like and can have a major benefit from a PDT. Furthermore, it seems unlikely that singlet oxygen or free radicals will develop resistance to cytotoxic action. The PDT is equally effective against antibiotic, antibiotic, resistant and susceptible bacteria, and repeated photosensitization does not induce resistant strain selection. The PDT procedure involves the laser activation of photosensitizing dye. As laser light irradiated only the test quadrants, there were no effects on bacteria in the control quadrants [12]. The results of this study correspond to those of the study that evaluate the effect only and in combination with conventional SRP of photo disinfection. In the group treated with SRP alone after 12 weeks, the authors have assessed 33 patients with chronic periodontitis for a clinical attachment gain of 0.36 0.35 mm. For SRP with adjunctive PDT, a gain of 0.86 0.61 mm was observed. These values are within the same range as in this study; the control group has less RAL values than the adjunctive PDT values in the group. A greater reduction in the BOP in the test group was observed in both studies.
Although the values for SRP with adjunctive PDT were substantially different, the differences were minor. In a 6-month follow-up, however, the effects of local drug delivery on the SRP were evaluated, PD differences were observed from 0.1 to almost 0.5 mm and smaller effects for attachment gains, although statistically different differences could be observed. A study assessing the effect of a chlorhexidine subgingival chip could detect a 0.5 mm difference in clinical attachment gain in favour of chlorhexidine after six months. However, it remains a question whether these improvements are clinically significant. The additional PDT application to SRP of one exposure did not lead to further improvements in pocket depth reduction and attachment gain, when evaluating patients who received supportive periodontal therapy, but it led to significantly higher BOP scores than SRP alone.
In patients with aggressive periodontitis, SRP was also compared to PDT alone. In a split mouth design, ten patients were treated. In both groups after 3 months a significant reduction in BOPs was observed. PD values and clinical attachment levels have also reduced after 3 months. A positive effect on attachment gain reduced PD and reduced use of metronidazole plus amoxicillin as sole therapy for periodontal treatments with mechanical debridement have recently been shown. However, the clinician should expect remaining mineralized deposits on the root surface, irrespective of the use of antibiotics or a PDT as the sole treatment system. This residual sub gingival calculus may serve as a base for bacteria and help to develop pockets and to progress periodontal disease. Any viable bacteria on rough surfaces of residual calculus could serve as a source of periodontal lesion re-infection and cause periodontitis to progress. In this study, all of the patients obtained SRP periodontal therapy with both hand instruments (curettes) and a piezo-electric headpiece for all the teeth. No difference was found in the treatment of chronic periodontitis concerning clinical outcome between ultrasonic and manual debridement. In addition, each patient was treated with both debridement procedures so that quadrants treated with split mouth design could be compared intra-experimentally.
A gentle gingival sulcus probing was performed with a pressure sensitive probe, since the sampling force of 20 g was demonstrated to avoid trauma of periodontal tissues during sampling. The present study shows that the use of PDT in conjunction with non-surgical treatment results has a positive impact. Increasing the number of exposures to photodynamic therapy is a newer approach to treat non-surgically as it is inferred that this could affect the microbial count. Thus, it could be possible to improve non-surgical periodontal therapy by adding antimicrobial photodynamic treatment exposures to conventional non-surgical therapy approaches.
Furthermore, the microbiological effects behind the clinical benefits observed should be studied and the decrease in microbial load to repeated exposures must be observed. From the above study, it can be concluded that in patients with chronic periodontitis, multiple exposures of adjunctive photodynamic therapy after conventional non-surgical therapy, i.e. scaling and root planning improves clinical outcomes.
Citation: Pawane IR, Ramamurthy J (2022) Evaluation of Photodynamic Therapy in Comparison with Conventional Treatment for the Treatment of Periodontal Disease: A Clinical Trial. Ann Essence Dent. 13:209.
Received: 01-Dec-2021 Accepted: 15-Dec-2021 Published: 22-Dec-2021
Copyright: © 2021 Pawane IR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.