
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2023)Volume 10, Issue 4
Background: Optimizing management of Persistent Pulmonary Hypertension of Newborn (PPHN) continues following availability of oral and intravenous Phosphodiesterase-V inhibitors. Study queried whether High Frequency Oscillatory Ventilation (HFOV) coupled with pulmonary vasodilators improves outcomes in neonates with severe- PPHN.
Objective: To prospectively evaluate efficacy of inhaled Nitric Oxide (iNO) and intra Gastric Sildenafil (iGS) in neonates with severe-PPHN on HFOV and exogenous surfactant.
Methods: Eighty-four consecutive neonates with severe-PPHN on HFOV and exogenous surfactant were treated with iNO (n=40) or iGS (n=44). Primary (28 days) outcomes analysed were adverse events, failure rate and mortality. Secondary (24 months) outcomes were neurological impairment, sensorineural deafness and chronic lung disease. At age 2 years neurodevelopmental evaluation by Bayley Scales of Infant and Toddler Development (Bayley-IIIUK) was performed.
Results: Adverse events (44%) occurred in iNO-(30%) versus (57%)-iGS (p=0.030). Failure rate (14%) was seen in iNO-0% versus 27%-iGS (p=0.001). Mortality rate (4%) was iNO-8% versus 0%-iGS (p=0.001). Neurological impairment (19%) ensued in iNO-32% versus 7%-iGS (p=0.001). Sensorineural deafness (4%) happened in iNO- 5% versus 2%-iGS (p=0.04). Chronic lung disease (5%) was observed in iNO-8% versus 2%-iGS (p=0.02). Normal neurological outcome occurred in 81%, iNO-68% versus 93%-iGS (p=0.010). Bayley-IIIUK scores at age 2-years were normal (108-116) in 81%, mild impairment (71-75) ensued in 10% and moderate to severe delay (57-62) occurred in 9%.
Conclusion: Intra-gastric sildenafil was as efficacious as inhaled nitric oxide in treating severe-PPHN in neonates on HFOV and exogenous surfactant. In 81% of children at age 2-years normal neurodevelopment followed, irrespective of adjuvant treatment modalities.
Children; Inhaled nitric oxide; Neonates; Persistent pulmonary hypertension; Sildenafil
CMV: Conventional Mechanical Ventilation; CPAP: Continuous Positive Airway Pressure; FIO2: Fraction of Inspired Oxygen; HFOV: High Frequency Oscillatory Ventilation; iNO: Inhaled Nitric Oxide; iGS: Intragastric Sildenafil; NICU: Neonatal Intensive Care Unit; OSI: Oxygen Saturation Index; ppm: Parts per million; PPHN: Persistent Pulmonary Hypertension of Newborn; SPO2: Saturation of Peripheral Oxygen
Occurrence of Persistent Pulmonary Hypertension of Newborn (PPHN) in Neonatal Intensive Care Units (NICUs) is 1.9 per 1000 live births with an associated mortality rate of 10% [1]. Treatment of severe-PPHN should ensure maximum lung recruitment coupled with lowered vascular resistance by pulmonary vasodilatation, enabling improved oxygenation and oxygen delivery to tissues. Efficient alveolar recruitment by High Frequency Oscillatory Ventilation (HFOV) and exogenous surfactant are known to enhance performance of pulmonary vasodilators, diminishing need for extra corporeal membrane oxygenation [2,3]. Inhaled Nitric Oxide (iNO) is an established pulmonary vasodilator widely used in treating severe-PPHN with a failure rate of 30% to 40% [4,5]. High failure rate of iNO has led to use of alternative vascular smooth muscle relaxants, as Phosphodiesterase-V inhibitors (PDE-5).
Sildenafil (Pfizer. Inc) and Tadalafil (Eli Lilly and Co) are currently recommended for pulmonary hypertension, due to their clinical effectiveness, good tolerance profile and mild transient side effects in children and adults [3,6]. Oral sildenafil has been effective in treating neonates with PPHN [6]. In refractory persistent pulmonary hypertension cases, endothelin antagonists and prostacyclin analogues can be used in combination with sildenafil [3].
Purpose of our study was to evaluate efficacy of iNO and iGS in treating severe-PPHN in neonates on HFOV and exogenous surfactant. Studied primary (28 days) outcomes were adverse events, failure rate and mortality. Secondary (24 months) measures assessed were neurological impairment, sensorineural deafness and chronic lung disease. At age 2 years neurodevelopmental evaluation by Bayley Scales of Infant and Toddler Development (Bayley-IIIUK) was performed.
Study population
Prospective linear observational study of eighty-four consecutive neonates with severe-PPHN between September 2006 and December 2016. Study was conducted at two University Teaching Hospitals with tertiary level III-NICUs. Study was approved by internal scientific review boards and consent was obtained for treatment, follow-up and data collection from neonate’s parents/carer. Research and ethics committee (No.02-5250022: 04/2006), approved study protocol, which confirmed with provisions of Declaration of Helsinki 1995 (Revised Edinburgh 2000).
Study design
Study cohort comprised of near-term neonates, ≥ 35-week’s gestation. Severe-PPHN was diagnosed by:
1. Three-dimensional-echocardiogram indicating a mean pulmonary artery versus mean systemic artery pressure ratio of >1 (PA/SA RATIO>1)
2. Validated non-invasive Oxygenation Saturation Index (OSI) showing OSI>26 (26-38). Formula calculating OSI: Mean Airway Pressure (MAP: cmH2O) × Fraction of inspired oxygen (FiO2) × 100 ÷ SpO2 (continuous measurement of oxygen saturation by pulse oximeter)
3. Persistent hypoxia (SpO2<90%, preductal partial pressure of oxygen (PaO2) 6.6-7.8 kilopascals (kPa)/49.5-58.5 mmHg and partial arterial pressure of carbon dioxide (PaCO2) ≥ 6 kPa/ ≥ 45 mmHg) despite optimal Conventional Mechanical Ventilation (CMV).
Cranial ultrasound scan for significant intracranial bleeds was performed prior to or immediately after commencement of treatment. Neonates requiring extracorporeal membrane oxygenation, congenital heart disease and life threatening multiple congenital malformations were excluded.
Treatment
All 84-neonates were initially on CMV, before commencement on HFOV (SLE5000, GE.UK.). Indication for HFOV was OSI>26 and SpO2<90%, PaO2<100 mmHg and mean airway pressure 12 cm H2O. Exogenous-surfactant (Beractant, Survanta, Intratracheal suspension 25 mg/mL, Kilitch Drugs India, Ltd) 100 mg/Kg, doses 1 to 2, was administered to all 84-neonates.
Inhaled nitric oxide
Disease severity and clinician judgement defined utilization of adjuvant vasodilator inhaled Nitric Oxide (iNO=40). iNO (20 ppm) was commenced in 40-neonates, for maximum duration of 96-hours. Indication for initiation of iNO (0-hours) was OSI>26, SpO2<90%, PaO2<100 mm Hg and mean airway pressure 12 cm H2O. Response to treatment (30-minutes) was evaluated by increases in PaO2: ≥ 20 mmHg, fall in oxygen saturation index (OSI: ≤ 10) with a decreased inspired oxygenation concentration (FiO2). Following successful treatment, iNO was gradually weaned (Figure 1). Nitrogen Dioxide (NO2) and methaemoglobin levels were regularly assessed. Methaemoglobin level was measured prior to initiation of iNO and subsequently, 1-hour after commencement. Thereafter, methaemoglobin level was assessed daily.
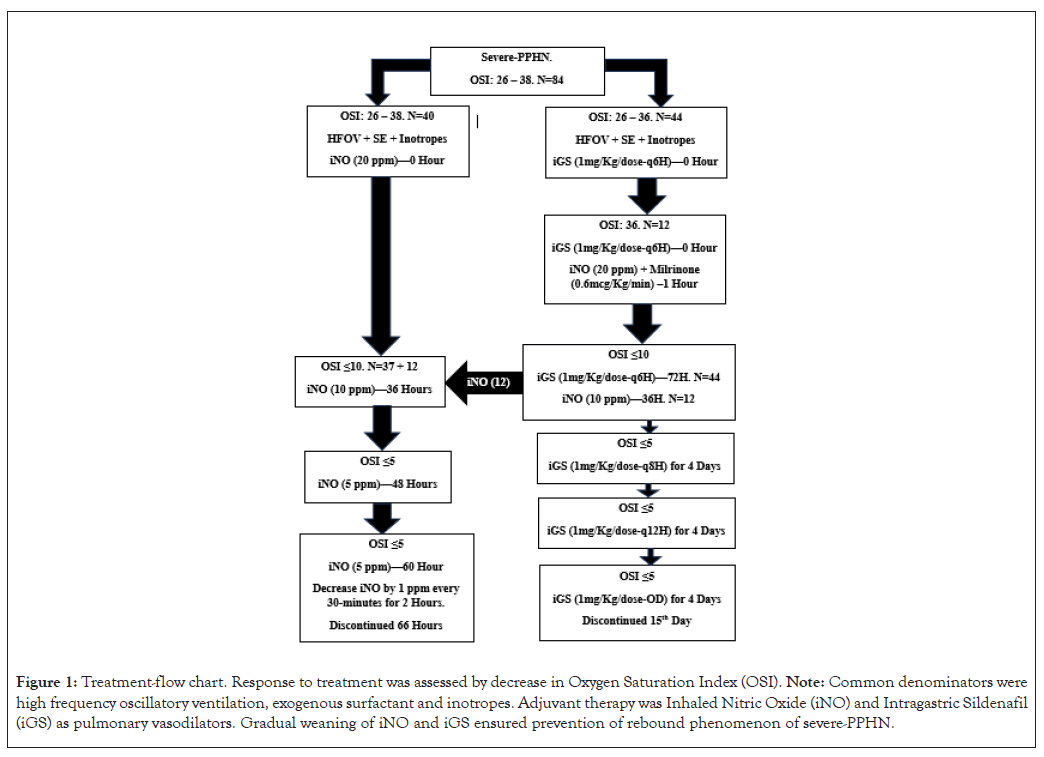
Figure 1: Treatment-flow chart. Response to treatment was assessed by decrease in Oxygen Saturation Index (OSI). Note: Common denominators were high frequency oscillatory ventilation, exogenous surfactant and inotropes. Adjuvant therapy was Inhaled Nitric Oxide (iNO) and Intragastric Sildenafil (iGS) as pulmonary vasodilators. Gradual weaning of iNO and iGS ensured prevention of rebound phenomenon of severe-PPHN.
Intra-gastric sildenafil
Clinician’s clinical opinion specified sildenafil (1 mg/Kg/dose, 6-hourly) usage in 44-newborns. Indication for commencement of Intra-Gastric Sildenafil (iGS=44) (0-hours) was OSI>26, SpO2<90%, PaO2<100 mmHg and mean airway pressure 12 cm H2O. Response (60-minutes) was evaluated by increases in PaO2: ≥ 20; fall in OSI: ≤ 10 and decrease in FiO2. Hospital pharmacy ensured accurate dilution and sterility of sildenafil citrate. Based on clinical response, therapy was continued for a total period of 72 hours (Figure 1). iGS was weaned over a period of 12-days (Figure 1).
Concomitant medication
Mean blood pressure ( ≥ 50th percentile) was maintained with dobutamine 10-20 mcg/kg/minute and dopamine 10 mcg/kg/ minute. Neonates were sedated with midazolam (60 mcg/kg/ hour) and fentanyl (1-5 mcg/kg/hour). Intravenous fluids and antibiotic therapy completed standardized care. Hydrocortisone (2 mg/kg/q6h) was administered to 41%; iNO-18% and 23%- iGS, neonates. Treatment protocols were in accordance with relevant NICU guidelines, regulations and product characteristic recommendations.
Stabilization
Following successful completion of treatment babies were transferred from HFOV to CMV. Infants were then weaned-off CMV to Continuous Positive Airway Pressure (CPAP). They were acclimatized to room air following a stabilization period on nasal cannula oxygen.
Evaluation
Tests performed at completion of treatment/discharge were: 1) Cranial ultrasound scan at discharge; 2) Three-dimensionalechocardiography prior to discharge; 3) Visual evoked potential test with electroencephalogram for optic nerve function within first 3 months; 4). Brainstem Auditory Evoked Response (BAER); 5). Magnetic resonance imaging of the brain at 2 years.
Bayley-IIIUK
To identify children with developmental deficits, polytomous ‘Bayley Scales of Infant and Toddler Development (Bayley-IIIUK)’ was used at age 24 months. Cognitive Index (Cognitive-language and Cognitive-language-motor), Language Index (receptive and expressive communication) and Motor Index (fine-motor and gross-motor skills) were measured. Bayley-III enabled comparison between child’s performance and same-age peers through normed scores (Index; M=100, SD=15). Standardized mean score is 100 (15), with scores <85 indicating mild impairment and <70 indicating moderate to severe impairment.
Statistics
Reported iNO failure rate of 40% and 20% for iGS was utilised for calculations. Standardized difference, p α (0.05) and power level, pꞵ (0.8) determined number required to power study (n=34). Null hypothesis clarified that to detect efficacy of iNO or iGS minimum of 68-patients (34 × 2) were required. To account for skewing of data due to inbuilt selection-bias and iNO crossover, identified population size was n=80 (40 × 2), which maintained 95% confidence interval and 95% z-scores (1.96). It was determined that numbers required at follow-up (age 24-months) were minimum (n=62) and maximum (n=66).
Univariate analysis was used to identify variables associated with outcomes and multivariate logistic regression analysis to determine independent associations of these variables with outcomes. Categorically variables were analysed by Chi square test with Yates correction. Student’s t test or Mann Whitney U test depending on distribution was used to compare continuous variables between iNO and iGS. Data is presented as mean (SD=Standard Deviation). P value <0.05 was considered statistically significant. 95% Confidence Intervals (CI) are shown to express true mean value (μ). Statistical analysis was performed using Statistical Package for Social Sciences software (SPSS 21 for Windows, SPSS Inc., Chicago, Ill., USA).
Demographics
Two thousand eight hundred and fifty-four neonates were admitted to NICUs. Eighty-four (2.9%) developed severe-PPHN (OSI: 26-38). In this cohort, risk of developing severe-PPHN was among male babies (69%) born by lower segment caesarean section (70%) (p=0.001) (Table 1). Table 1 outlines neonatal and maternal anthropometric data. Despite heterogeneity regarding primary pathology and maternal risk factors, variables were comparable between iNO and iGS cohorts (Table 1). Cytogenetic analysis indicated normal male or female karyotype in all 84-neonates.
| Characteristics | iNO (n=40) | iGS (n=44) | p value | 95% (CI) |
|---|---|---|---|---|
| Anthropometric attributes | ||||
| Gender-male 69% | 28 (70%) | 30 (68%) | 0.68 | 0.410-0.894 |
| Gestational age (weeks). mean (SD) | 35.8 (3) | 38.2 (1.5) | 0.762 | 0.512-0.981 |
| Birth weight (grams). mean (SD) | 3073.4 (489.4) | 3346 (387.4) | 0.644 | 0.522-0.876 |
| Birth weight Z-scores. mean (SD) | 0.17 (1.11) | 0.19 (1.02) | 0.512 | 0.311-0.721 |
| Head circumference (cm). mean (SD) | 32.5 (1.5) | 32.4 (1.4) | 0.766 | 0.276-0.882 |
| Primary pathology | ||||
| Meconium aspiration syndrome-37% | 15 (38%) | 16 (36%) | 0.892 | 0.751-0.938 |
| Pneumonia-sepsis-30% | 12 (30%) | 13 (30%) | 0.89 | 0.733-0.936 |
| Congenital diaphragmatic hernia - 33% | 13 (32%) | 15 (34%) | 0.763 | 0.621-0.814 |
| Maternal factors | ||||
| Maternal age (years). mean (SD) | 28.7 (3) | 27.5 (3) | 0.866 | 0.746-0.900 |
| Mode of delivery-LSCS (70%) | 27 (68%) | 32 (73%) | 0.08 | 0.010-0.210 |
| Maternal pre-pregnancy BMI>27 | 7 (18%) | 9 (21%) | 0.066 | 0.020-0.880 |
| Gestational diabetes | 8 (20%) | 6 (14%) | 0.844 | 0.660-0.930 |
| Hypertension | 5 (13%) | 7 (16%) | 0.846 | 0.056-0.982 |
| Preeclampsia | 6 (15%) | 5 (11%) | 0.988 | 0.770-0.990 |
| Maternofoetal rhesus incompatibility | 3 (8%) | 1 (2%) | 0.02 | 0.001-0.070 |
| Anaemia | 7 (18%) | 6 (14%) | 0.982 | 0.675-0.988 |
| Consanguinity first cousins. Inbreeding co-efficient of <0.0156 | 1 | 2 | 0.077 | 0.022-0.087 |
Note: BMI=Body Mass Index, LSCS=Lower Segment Caesarean Section.
Table 1: Maternal and neonatal characteristics.
Treatment response
Neonates (n=84) were severally ill with validated SNAPPE-II scores of 72 (6) and OSI 35 (4). Illness severity was comparable between groups, iNO versus iGS; SNAPPE-II: 72 (4) versus 68 (3), (p=0.658, 95% CI: 0.551-0.776) and OSI: 38 (5) versus 36 (3), (p=0.663, 95% CI: 0.549-0.754). Neonates were commenced on HFOV after having been on CMV for 4.3 (1.1)-hours (Table 2). In 12-newborns on iGS (27%), iNO (20 ppm) and milrinone (phosphodiesterase-III inhibitor) 0.6 mcg/kg/minute infusion, post loading dose of 50 mcg/kg was started due to persistent high OSI 36 (2).
| Ventilatory parameters | ||||
|---|---|---|---|---|
| Characteristics | iNO (n=40) | iGS (n=44) | p value | 95% (CI) |
| Mean (SD) duration: HFOV in hours | 68 (2) | 72 (2) | 0.822 | 0.614-0.960 |
| Mean (SD) duration: CMV post-HFOV in hours | 46 (1) | 42 (2) | 0.646 | 0.510-0.752 |
| Mean (SD) duration: CPAP | 54 (2) | 52 (3) | 0.801 | 0.614-0.884 |
| Mean (SD) duration: Pulmonary vasodilators | 66 (2) | 72 (0) | 0.622 | 0.701 - 0.740 |
| Length of hospital stay (mean) | ||||
| NICU days | 28 | 31 | 0.63 | 0.522-0.711 |
| Length of stay in days on NICU and SCBU | 48 | 52 | 0.661 | 0.520-0.712 |
| Outcomes | ||||
| Adverse events (44%) | (12/40) 30% | (25/44) 57% | 0.03 | 0.010-0.044 |
| Treatment failure rate (14%) | 0 | (12/44) 27% | 0.001 | -0.086 |
| Overall mortality rate (4%) | (3/40) 8% | 0% | 0.001 | -0.095 |
| Resolution of PPHN without sequela | (25/37) 68% | (41/44) 93% | 0.01 | 0.008-0.026 |
| Resolution with neurological sequela (n=15/81: 18.5%) | (12/37) 32% | (3/44) 7% | 0.001 | -0.085 |
Note: CMV=Conventional Mechanical Ventilation, CPAP=Continuous Positive Airway Pressure, HFOV=High Frequency Oscillatory Ventilation, NICU=Neonatal Intensive Care Unit, PPHN=Persistent Pulmonary Hypertension of the Newborn, SCBU=Special Care Baby Unit.
Table 2: Ventilatory features, hospital stay and outcome measures.
Response to treatment occurred at 4-hours, with a significant sustained decline in OSI by 53%, OSI: iNO-17 (2) versus 12 (1)- iGS, (p=0.066, 95% CI: 0.058-0.080). By 36 hours, 81-neonates had an OSI 7.4 (1.2). Three neonates on iNO (8%) with initial OSI (36) responded to therapy with a fall in OSI (22) at 2 hours. Rebound deterioration occurred at 4-hours, OSI (36). By 24-hours a positive response was noted with gradual reduction of OSI (20). Recurrence of rebound phenomenon at 36-hours, say an increase in OSI (36), which led to nonresponse to treatment and demise.
Fifty-two-neonates treated with iNO 20 ppm produced minimal levels of nitrogen dioxide 0.6 ppm and methaemoglobin 0.4%.
Primary outcomes
Table 2 summarises outcomes. Failure rate in iGS (27%) was significant necessitating commencement of iNO and milrinone in 12-newborns. iGS was not discontinued (Table 2 and Figure 1). Adverse events (44%) predominantly occurred in iGS-(57%) versus 30%-iNO (p=0.030), which were 1) Hypotension: iGS- 18% versus 5%-iNO (p=0.001), 2) Hypokalaemia: iGS-7% versus 3%-iNO (p=0.040) and 3) Pneumothorax: iGS-11% versus 5%- iNO (p=0.040). Other events encountered were 1) Anaemia: iGS-16% versus 15%-iNO (p=0.840) and 2) Bradycardia: iGS- 5% versus 3%-iNO (p=0.660). Drug withdrawal syndrome did not occur in either iNO or iGS treated neonates. At discharge, 3-dimensional-echocardiography was normal in all 81-neonates.
Secondary outcomes
Table 2 summarizes outcomes. Hypoxemic encephalopathy (3%) and cerebral palsy (8%) occurred in iNO (p=0.001, 95% CI: -0.088-0.002). Epilepsy needing treatment ensued in 6%, iNO- 11% versus 2%-iGS (p=0.020, 95% CI: 0.008-0.030). Hearing deficit requiring cochlear implants was necessary in 4%, iNO- 5% versus 2%-iGS (p=0.040, 95% CI: 0.001-0.051). Chronic lung disease was observed in 5%, iNO-8% versus 2%-iGS, (p=0.020, 95% CI: 0.010-0.002). In these children (5%), initial, grade 1 bronchopulmonary dysplasia was downgrade to grade 0 and none needed home oxygen therapy at discharge.
Intraventricular haemorrhage or leukomalacia was not noted on cranial ultrasonography prior to commencement of treatment and subsequently, at discharge. Four-children with neurological impairment, on magnetic resonance imaging, showed white matter damage in cortical and subcortical area of left temporal lobe (n=2), parietal-occipital lobes (n=1) and occipital cortex and left basal ganglia (n=1). Magnetic resonance imaging delineated delayed myelination on posterior limb of internal capsule and optic radiation without occipital or parietal atrophy, in two-children with normal development and visual acuity.
Neurodevelopmental outcomes
Maternal and birth-anthropometric data are summarized in Table 1. Parental ethnicity was Indians (60%), Arabs (19%), British Indians (15%) and Caucasians (6%). Parents were bilingual (100%) and affluent (61%) with a high educational level (82%). Majority were non-smokers (91%).
At age 2 years mean-weight was 12.9 (0.4) kg, mean-height was 83 (5.4) cm and mean-head circumference was 47 (1.3) cm. Anthropometric measurements were all age-appropriate (50th percentile).
Bayley-IIIUK scores were normal (108-116) in 81% of children (Tables 3 and 4). There was a good correlation between neonates studied in this cohort, who were neurologically normal (81%) and normative data for the four-developmental domains: Personal and Social: p=0.88, 95% CI: 0.79–0.93, Language: p=0.93, 95% CI: 0.89-0.96, Fine motor: p=0.89, 95% CI: 0.82- 0.94 and Gross motor: p=0.86, 95% CI: 0.77-0.92 (Table 3). Duration of nitric oxide and sildenafil therapy did not impact on neurodevelopmental outcomes (Table 2).
| Bayley IIIUK: Neurodevelopmentally normal children (81%) | |||
|---|---|---|---|
| Measurements | Composite score mean (95% CI) iNO (n=25) |
Composite score mean (95% CI) iGS (n=41) |
p value 95% CI |
| Cognitive index | 108 (102-118) | 111 (102-116) | 0.95 (0.88-0.98) |
| Language index | 111 (104-115) | 112 (103-116) | 0.99 (0.84-1.00) |
| Motor index | 112 (108-120) | 114 (107-122) | 0.98 (0.88-1.00) |
| Cognitive-language | 106 (104-108) | 109 (102-110) | 0.97 (0.89-1.00) |
| Cognitive-language-motor | 108 (103-110) | 110 (100-115) | 0.96 (0.87-0.99) |
Table 3: Bayley IIIUK neurodevelopmentally normal children at age 2 years.
| Bayley IIIUK: Neurodevelopmentally impaired children (19%) | ||
|---|---|---|
| Measurements | Composite score: Mean (95% CI) | Composite score: Mean (95% CI) |
| Mild impairment (10%) | Moderate/Severe delay (9%) | |
| Cognitive index | 71. 3 (70-75) | 57.2 (55-65) |
| Language index | 75 (70-80) | 58.1 (55-69) |
| Motor index | 73 (70-80) | 59.7 (55-66) |
| Cognitive-language | 74 (70-80) | 62.1 (55-68) |
| Cognitive-language-motor | 71.2 (70-75) | 59.4 (55-65) |
Table 4: Bayley IIIUK neurodevelopmentally impaired children at age 2-years.
Nineteen percent had neurodevelopmental delay (Tables 3 and 4). Mild impairment (71-75) occurred in 10%; iNO-47% versus 7% iGS (p=0.001) and moderate to severe delay (57-62) in 9%; iNO-33% versus 13%-iGS (p=0.030). Mean difference in developmental quotient of children neurologically impaired (19%), iNO-80% versus 20%-iGS, (p=0.001, 95% CI: -0.086- 0.004) was significant.
HFOV and exogenous surfactant achieved adequate alveolar recruitment and ventilation in studied cohort. Early commencement of inotropes and pulmonary vasodilators increased cardiac output, maintained adequate mean blood pressure and enhanced oxygen delivery to tissues. Although, studied population were sick with OSI ( ≥ 26), 53% responded in first 4-hours with decrease in OSI ( ≤ 17). Adopting dosage ranges, which had least side effects, iNO (20 ppm) and iGS (1 mg/ kg/dose) probably reduced adverse events during treatment. All complications, which occurred were minor and easily treatable. A wide variation in reported oral sildenafil dose (1 mg/kg/ dose to 2 mg/kg/dose and 3 mg/kg/dose) was seen since the preliminary report in 2006 [6-9]. Usage of iGS (1 mg/kg/dose) as an adjuvant pulmonary vasodilator in studied cohort was well tolerated. Hypotension (18%) and hypokalaemia (7%), which ensued was amicable to treatment without need for cessation of iGS. Anaemia, which occurred in iGS and iNO needed packed cell transfusion. Aetiology was probably multifactorial, with iatrogenic blood withdrawal for investigations being common.
Significant failure rate (27%) was observed in studied cohort, which compared to that reported by Sayed and Bisheer for oral sildenafil (22%) and intravenous sildenafil (28%) by Pierce [7,10]. This high failure rate could be related to severity of PPHN (OSI 36) in studied babies. iGS was not discontinued and iNO and milrinone (phosphodiesterase-III inhibitor) were added as adjuvants to these 12-neonates. Clinically they acted synergistically to improve OSI, as observed in reported intravenous sildenafil and iNO studies [10,11]. Sildenafil probably reduced degradation of cGMP produced by iNO, thereby, working synergistically to improve cardiac output, reducing pulmonary hypertension.
Reported high death rate (20% to 30%) in neonates with severe- PPHN did not occur in studied cohort (4%) [8,12,13]. Studied cohort mortality rate of 4% was comparable to recent literature (3% to 6%) on intravenous sildenafil/inhale nitric oxide and oral sildenafil monotherapy [7,9,10]. This may be due to improvements in medical technology, patient care and optimal management by inotropes and vasoactive agents.
Limiting factor of this study was physician assignment bias and absence of assessment of serum sildenafil levels during treatment. Cohort studied were ill (OSI: 26-38), illness severity and length of hospital stay were comparable between iNO and iGS treated babies. Response and recuperation with minor complications (44%) and low mortality (4%) highlights efficacy of treatment protocol. Impact of concomitant medications, inotropes, hydrocortisone and milrinone on treatment responses need to be further evaluated.
Eighty-one percent of children studied were medically and neurologically normal with complete resolution of disease processes without sequelae. Relatively high socioeconomic status and good parental education contributed positively towards language skills, cognitive index scores and normal neurodevelopment at 2-years (Bayley-IIIUK scores ≥ 85), with narrow 95% CI between studied children and normative data for all four-developmental domains. This was comparable between those treated by nitric oxide and/or sildenafil with no significant statistically difference between duration of either therapy.
Occurrence of impaired neurodevelopment was 19%, which predominantly was observed in those children treated with nitric oxide (15%). This incidence was comparable with that reported in literature 12.8% to 21.5%. Sensorineural loss necessitating cochlear implants occurred in 4% of children, which was within reported range for sensorineural and conductive hearing loss (10% to 12%) [12,13]. In children treated with sildenafil, incidence of neurological abnormalities was 4%. Impaired intellectual and cognitive function in children could be due to impairment of glutamate-nitric oxide-cGMP pathway. Increasing extracellular cGMP by sildenafil maybe a new therapeutic approach to improve cognitive and neurological function in neonates and children.
Effect of sildenafil in neonatal period was global leading to preserved intellectual, cognitive and neurological outcome, in later childhood. Inclusion of sildenafil in the armoury of drugs, which can be utilized in treating severe-PPHN has been reasonably justified.
This study evaluates the efficacy of inhaled Nitric Oxide (iNO) and intragastric Sildenafil (iGS) in neonates with severe Persistent Pulmonary Hypertension of Newborn (PPHN) undergoing High Frequency Oscillatory Ventilation (HFOV) and exogenous surfactant. The results demonstrated that iGS was as efficacious as iNO in treating severe PPHN in this specific population. The neurodevelopmental outcomes at age 2 years, assessed using Bayley Scales of Infant and Toddler Development (Bayley-IIIUK), revealed that 81% of children in the study had normal neurodevelopment, irrespective of the adjuvant treatment modalities. There was a higher incidence of neurodevelopmental delay in the iNO group, with mild impairment and moderate to severe delay occurring more frequently compared to the iGS group.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Parapurath R, Samuel M (2023) Efficacy of Inhaled Nitric Oxide and Intragastric Sildenafil in Treatment of Persistent Pulmonary Hypertension of Newborn (PPHN) on High Frequency Oscillatory Ventilation (HFOV). Adv Pediatr Res. 10:068.
Received: 07-Nov-2023, Manuscript No. LDAPR-23-27950; Editor assigned: 09-Nov-2023, Pre QC No. LDAPR-23-27950 (PQ); Reviewed: 23-Nov-2023, QC No. LDAPR-23-27950; Revised: 30-Nov-2023, Manuscript No. LDAPR-23-27950 (R); Published: 07-Dec-2023 , DOI: 10.35248/2385-4529.23.10.068
Copyright: © 2023 Parapurath R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.