
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Case Report - (2024)Volume 11, Issue 1
Nephronophthisis (NPHP) is an autosomal recessive cystic disease of the kidney that is identified based on its different forms of gene mutations. More than 10 percent of NPHP cases can manifest with extra-renal manifestations, including Senior-Loken Syndrome (SLSN), mental retardation, liver fibrosis, skeletal changes, etc., and their renal involvement will eventually lead to End-Stage Renal Failure (ESRD), requiring a kidney transplant. 150 cases of SLSN have been reported worldwide. Due to the rarity of this syndrome and the lack of reports of its identification in this region, we decided to report a case of SLSN in a 13-year-old boy who was referred to our clinic to find the cause of high creatinine. In the patient's history and subsequent investigations, there were symptoms of hypopituitarism, mild retinal dystrophy, severe osteopenia, mild liver fibrosis and NPHP.
Senior-loken syndrome; Hypopituitarism; Blindness; Kidney failure; Vision
Nephronophthisis (NPHP) is a disease that causes cystic kidneys or cystic dysplasia of the kidney. In the first two decades of a person's life, this hereditary condition is the most prevalent cause of chronic kidney disease. One of the extra renal companions of NPHP is retinal dystrophy. This disease appears as Leber Congenital Amaurosis (LCA) or Retinal Pigmentary Degeneration (RPD) with late-onset. This illness manifests in early infancy or adolescence and results in a visual impairment that may vary from night blindness to functional blindness [1]. Senior-Loken Syndrome (SLSN) is an autosomal recessive syndrome and a type of NPHP-related disorder that is associated with cystic kidney disease and retinal dystrophy, such as Retinitis Pigmentosa (RP) or LCA. It is a harmful disease that culminates in blindness and kidney failure. The visual prognosis is usually poor and definitive treatment is not available to date. However, kidney transplantation appears to be the best option for End- Stage Renal Failure (ESRD). The first mention of it was made in a family where six out of thirteen children had nephronophthisis with retinal band degeneration. In the same year, the same condition in two siblings elsewhere. Both siblings had blindness and severe renal failure and a kidney biopsy showed renal tubule atrophy and dilatation [2,3].
A 13-year-old boy was referred to our clinic to find out the cause of his high creatinine. The patient was the first child of the family, with related parents (cousin and cousin) and a healthy 6-year-old brother. The patient's problems, which started at the age of 7 with fever and chills, weakness and severe lethargy, polyuria and polydipsia, led to hospitalization. At that time, the liver, gall bladder, spleen and pancreas were normal. Although the shape and size of the kidneys were normal, a slight increase in parenchymal echogenicity of both kidneys with a simple cyst in the upper bridge of the left kidney was reported. The urinalysis was normal and there was no anemia. To find the cause of severe lethargy, thyroid tests were taken and due to low Thyroxine (T4) and normal Thyroid-Stimulating Hormone (TSH) in the tests, a thyroid scan was performed on the patient and a mild diffuse goiter was reported. With further investigation, a deficiency of Adrenocorticotropic Hormone (ACTH) and cortisol was observed and pituitary hypoplasia was reported during Magnetic Resonance Imaging (MRI) of the pituitary gland (Figure 1).
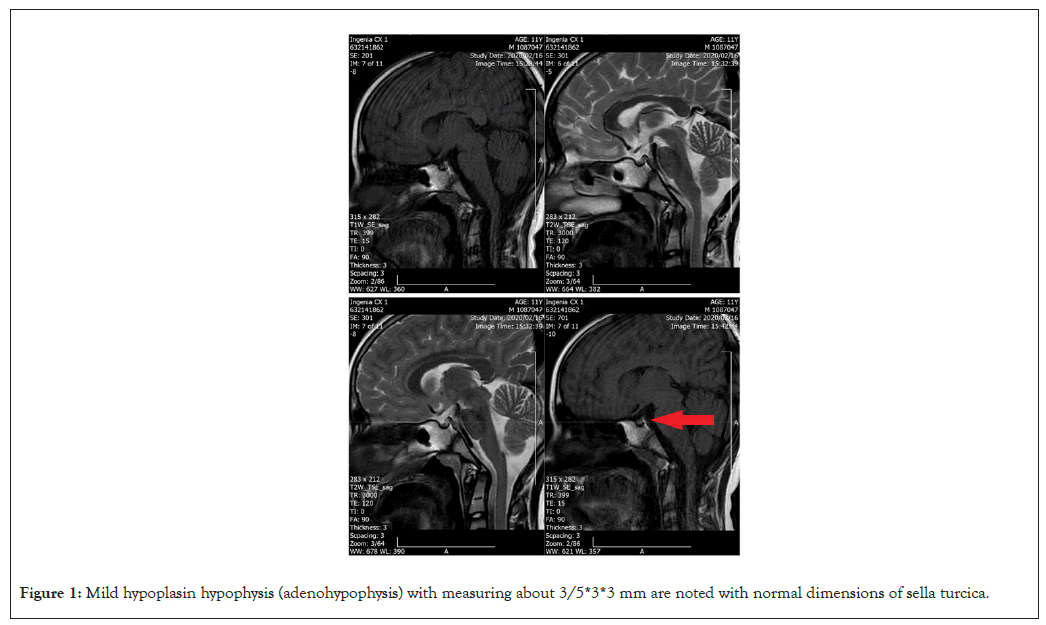
Figure 1: Mild hypoplasin hypophysis (adenohypophysis) with measuring about 3/5*3*3 mm are noted with normal dimensions of sella turcica.
Therefore, the patient diagnosed with hypopituitarism was treated with levothyroxine, hydrocortisone and desmopressin spray. Currently, by examining the laboratory documents and previous and current imaging of the patient, it was seen that the increase in creatinine of the patient started at the age of 9 with slow progress and gradually the creatinine level reached 1.8, but still, in the urinalysis, only the specific gravity of the urine is low without hematuria and proteinuria [4,5]. Therefore, according to high serum creatinine and urinalysis with hyposthenuria and normal size of kidneys with increased parenchymal echogenicity of kidneys along with left kidney cyst in ultrasound and attribution of parents, caused the suspicion of NPHP, which was justified by the patient's hypopituitarism with its extrarenal manifestations. Therefore, with the initial suspicion of one of the types of NPHP that can lead to hypopituitarism, the initial diagnosis of Rhyns syndrome was made for the patient and in a further investigation in terms of eye and ear involvement, mild retinal dystrophy was reported in the ocular examination, but the ear examination and audiometry were normal. In the densitometry performed on the patient, there was severe osteopenia and in the fibro-scan of the liver, mild fibrosis of the liver was reported. A decrease in corticomedullary differentiation in the kidneys and a brief coarsening of the liver parenchyma were also reported. According to the above, to confirm the diagnosis, a Whole Exome Sequencing (WES) genetic test focusing on NPHP genes has been done and the diagnosis of Senior-Loken Syndrome-4 (SLSN-4)/NPHP-4 was reported. The patient now is undergoing medical and symptomatic treatment for renal and extrarenal complications of NPHP [6].
Clinical symptoms of the patient
Proband is a 13 years old boy with kidney failure, muscles cramp, polyuria, polydipsia, vision problems, osteoporosis and hypothyroidism. Symptoms started when he was 7 years old.
NPHP-4 gene
The NPHP-4 gene encodes a protein which contains a prolinerich region. The encoded protein may function in renal tubular development and function [7]. This protein interacts with nephrocystin. Mutations in this gene cause Senior-Loken Syndrome-4 (SLSN-4), which is a rare disorder characterized by the combination of two specific features: a kidney condition called nephronophthisis and an eye condition known as Leber Congenital Amaurosis (LCA). Nephronophthisis causes fluidfilled cysts to develop in the kidneys beginning in childhood. These cysts impair kidney function, initially causing increased urine production (polyuria), excessive thirst (polydipsia), general weakness and extreme tiredness (fatigue) [8,9]. Nephronophthisis leads to End-Stage Renal Disease (ESRD) later in childhood or in adolescence. ESRD is a life-threatening failure of kidney function that occurs when the kidneys are no longer able to filter fluids and waste products from the body effectively. LCA primarily affects the retina, which is the specialized tissue at the back of the eye that detects light and color. This condition causes vision problems, including an increased sensitivity to light (photophobia), involuntary movements of the eyes (nystagmus) and extreme farsightedness (hyperopia). Some people with SLSN develop the signs of LCA within the first few years of life, while others do not develop vision problems until later in childhood [10-13].
Based on American College of Medical Genetics and Genomics (ACMG) classification, the c.3644+1G>A variant in the NPHP-4 gene is pathogenic, shown in Table 1. Multiple lines of computational evidences such as Machine Translation (MT), BayesDel, SpliceAI, dbscSNV Ada, Radio Frequency (RF), Genomic Evolutionary Rate Profiling (GERP) and Geno-canyon support a deleterious effect of this mutation on the gene or gene product.
| Gene | Position/variant | Zygosity | Inheritance | Disease | Allele frequency (gnomAD) | Classification |
|---|---|---|---|---|---|---|
| NPHP-4 | chr1:5926432:C>T: NPHP4NM_015102:exon26: c.3644+1G>A |
HOM | AR | Senior-loken syndrome 4 (606996) | 0.0000319 | Pathogenic |
Table 1: Characteristics of Nephronophthisis (NPHP) gene.
The primary objective of therapy is to delay the onset of renal failure as well as the need for dialysis treatment and kidney transplantation. In the future, more recent medications, such as Vasopressin2 (V2) receptor antagonists, which may alter the progression of the illness as well as the process by which cysts are formed, may be employed. Management of ocular illness is mainly supportive therapy. To monitor the development of the disease's involvement in the retina, yearly eye exams are advised. Early diagnosis, hypertension management and protein intake can all postpone dialysis. Proving the genetic diagnosis of the disease helps in the management of the patient and also helps the parents in genetic counseling to prevent the occurrence of the disease in subsequent pregnancies. NPHP-4 is located on chromosome 1p36 and encodes nephrocystin 4. Approximately 50 percent of NPHP cases arising from NPHP-4 biallelic pathogenic variants develop extrarenal symptoms. In an investigation of 152 children with NPHP monitored for a mean of 7.5 ± 6.1 years (standard deviation), NPHP-4 subgroup patients had a higher mean age at diagnosis (mean, 12.0 ± 4.4 years), which is consistent with previous reports of NPHP-4 complications. It relates to renal failure that happened between the ages of 6 and 20 and 6 and 35 respectively, which corresponds to the average age of 12.7 and 22 years, respectively. Studies showed that the inheritance of SLSN is autosomal recessive. The discovery of this pathogen made it possible to confirm the clinical diagnosis and provide pre-marriage counseling and appropriate genetic tests for couples who want to marry in this high-risk family.
Smith, Graham and Fanconi were the first to describe cystic diseases of the renal medulla, which led to the coining of the name juvenile familial nephronophthisis in 1951. Both senior and Loken reported the association between nephronophthisis and tape-to-retinal degeneration in 1961, occurs in around 10 to 15 percent of all instances of nephronophthisis. Renal dysplasia-blindness, inherited renal-retinal syndrome and renalretinal dysplasia are further names for SLSN [4-6]. Nephrocystin genes, including NPHP-1, NPHP-2, NPHP-3, NPHP-4, NPHP- 5, NPHP-6, NPHP-7, NPHP-8, NPHP-9, NPHP-10, NPHP-11, NPHP-12 and mutations in IQCB 1 (also called NPHP-15) are known to be the most frequent causes [7]. Depending on the age at which end-stage renal disease manifests, there are three clinical types of nephronophthisis: severe, infancy and adolescent; severe childhood, adolescent. The initial symptoms of polyuria, polydipsia and enuresis are due to a focal defect, which is consistent with our patient's symptoms in early childhood. Although late onset in the third decade has also been observed, most cases develop into end-stage renal disease before the age of 20 [8,9]. Primary cilia, sensory organelles that link mechanosensory, osmotic, visual and other stimuli for cell cycle regulation, dysfunction in nephronophthisis, which causes multisystem involvement and a wide range of extrarenal symptoms, which includes retinal degeneration, coloboma, aplasia of the cerebellar vermis, polydactyly, oculomotor apraxia (cogan type), neonatal tachypnea (Joubert syndrome), electro retinal abnormalities (Sensenbrenner syndrome) and cranioectodermal dysplasia [7,10]. Ocular manifestations may be tape-to-retinal degeneration, the most prevalent form, Leber-type congenital amaurosis, late-onset pigmentary retinal degeneration or progressive choroidal and retinal degeneration. Additionally, it may manifest as keratoconus, coats disease or cataracts [14]. Interstitial infiltration, renal tubular cell atrophy with cyst formation and renal interstitial fibrosis are the three hallmarks that define the histology of a kidney. Interstitial infiltration, renal tubular cell atrophy with cyst formation and renal interstitial fibrosis make up the triad that defines renal histology [15]. Juvenile nephropathy may have normal ultrasonographic results or may show increased echogenicity of the renal parenchyma, medullary cysts, poor corticomedullary differentiation and a small kidney. However, the diagnosis of juvenile nephropathy is not ruled out by the absence of a medullary cyst at the time of examination. Nephronophthisis has no curative treatment [14-16].
According to the patient's history of polyuria and polydipsia, decreased ability to concentrate urine in the morning sample, lack of edema and hypertension as a sign of kidney failure and a kidney ultrasound report consistent with the disease, including normal kidney size, kidney cyst, increased renal parenchymal echo and decreased corticomedullary differentiation. NPHP was presented to the patient and considering that other extrarenal symptoms of the patient could be justified with this syndrome, a genetic study was performed for the patient, which is an accurate and reliable method of diagnosing NPHP. Finally, SLSN was diagnosed with NPHP-4 gene involvement.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Farhad S, Ekhlasi N, Kisomi ER, Mohebbi A, Shahla MM (2024) A Rare Case of Nephronophthisis Type IV (Senior-Loken Syndrome) Representing with Hypopituitarism. Adv Pediatr Res. 11:072
Received: 27-Dec-2023, Manuscript No. LDAPR-23-28618; Editor assigned: 29-Dec-2023, Pre QC No. LDAPR-23-28618 (PQ); Reviewed: 12-Jan-2024, QC No. LDAPR-23-28618; Revised: 19-Jan-2024, Manuscript No. LDAPR-23-28618 (R); Published: 26-Jan-2024 , DOI: 10.35248/2385-4529.24.11.072
Copyright: © 2024 Farhad S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.