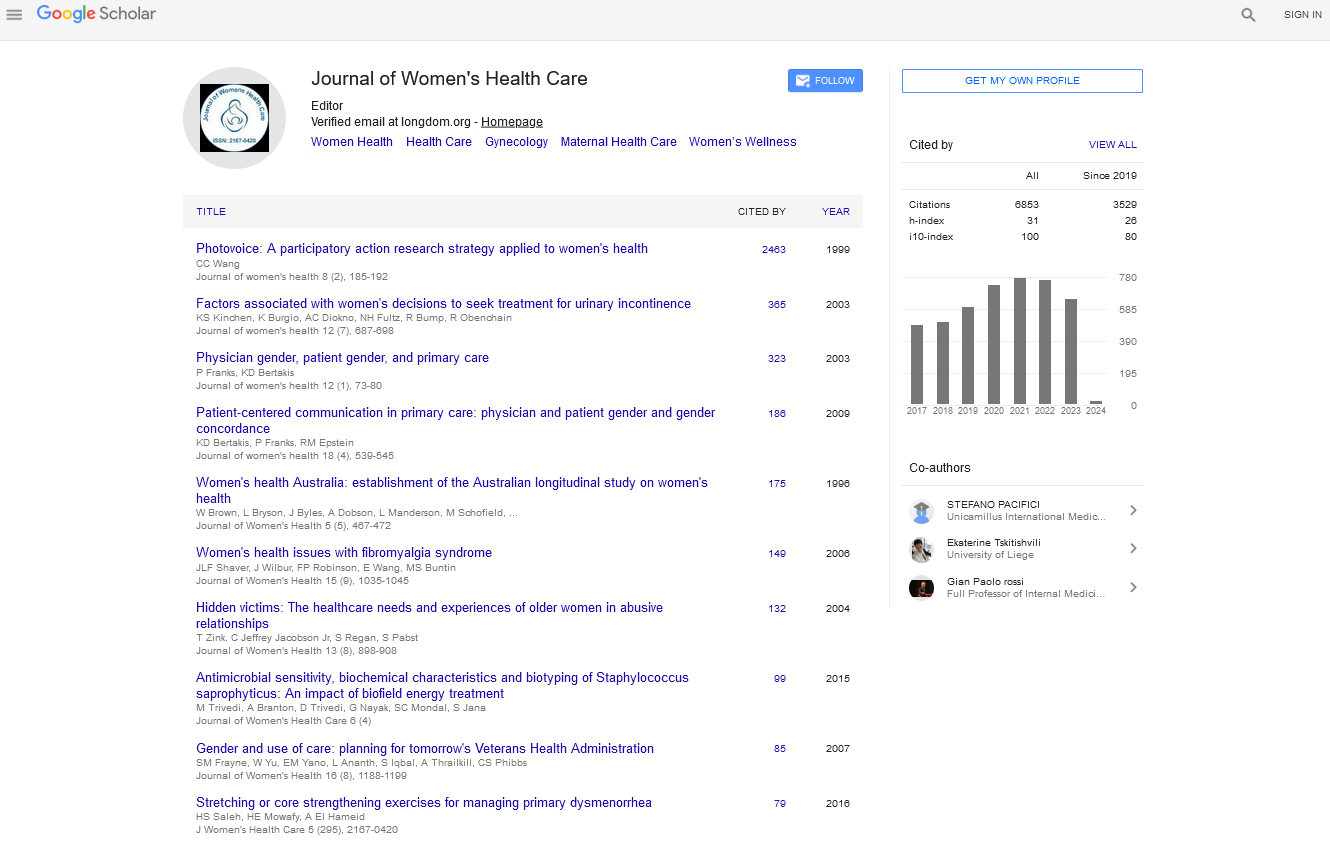
Journal of Women's Health Care : Citations & Metrics Report
Articles published in Journal of Women's Health Care have been cited by esteemed scholars and scientists all around the world. Journal of Women's Health Care has got h-index 21, which means every article in Journal of Women's Health Care has got 21 average citations.
Following are the list of articles that have cited the articles published in Journal of Women's Health Care.
| 2022 | 2021 | 2020 | 2019 | 2018 | |
|---|---|---|---|---|---|
Total published articles |
60 | 61 | 30 | 28 | 43 |
Conference proceedings |
50 | 13 | 0 | 24 | 120 |
Citations received as per Google Scholar, other indexing platforms and portals |
759 | 774 | 728 | 597 | 503 |
| Journal total citations count | 1841 |
| Journal impact factor | 5.14 |
| Journal 5 years impact factor | 4.65 |
| Journal cite score | 5.88 |
| Journal h-index | 21 |
| Journal h-index since 2019 | 21 |
Important citations (1671)
Okube ot, sambu lm. determinants of preterm birth at the postnatal ward of kenyatta national hospital, nairobi, kenya. open journal of obstetrics and gynecology. 2017 sep 22;7(09):973. |
|
Sinta pa. the effectiveness of ginger extract towards reducing the levels of menstrual pain scores in adolescents: study: literature review. |
|
Putra me, pramitaresthi ig, yanti np. hubungan dismenore primer dengan prestasi belajar mahasiswi program studi ilmu komunikasi fisip unud. |
|
Zeru ab, muluneh ma. thyme tea and primary dysmenorrhea among young female students. adolescent health, medicine and therapeutics. 2020;11:147. |
|
Shellasih nm, ariyanti f. factors of primary dysmenorrhea in junior high school students in south tangerang city, indonesia, 2018. |
|
Purba wt, azhar mb, roflin e. association of dysmenorrhea and quality of life in female stundents at xaverius i senior high school palembang academic year 2018-2019. majalah kedokteran sriwijaya. 2019 jun 22;51(1):23-9. |
|
C iwuoha e. effects of dysmenorrhea on academic and social activities of students in tertiary institutions in an urban city, south east nigeria. |
|
Tadese m, kassa a, muluneh aa, altaye g. prevalence of dysmenorrhoea, associated risk factors and its relationship with academic performance among graduating female university students in ethiopia: a cross-sectional study. bmj open. 2021 mar 1;11(3):e043814. |
|
Goda sm, mohamed sa, hassan ak, el-aty a, saad n. prevalence of primary dysmenorrhea among secondary girl students at assiut city. assiut scientific nursing journal. 2020 mar 1;8(20.0):44-54. |
|
Kushwaha rp, rauniar gp, sarraf dp, rai ds, sinha p, sitaula s, yadav p, sah b. evaluation of the severity and self-management practice in primary dysmenorrhea in medical and dental students: a cross-sectional study in a teaching hospital. asian journal of medical sciences. 2021 mar 1;12(3):59-65. |
|
Nermeen tm, soheir m, yosseuf h. effect of body mass index on primary dysmenorrhea and daily activities in adolescents. the medical journal of cairo university. 2020 mar 1;88(march):79-84. |
|
Rifati w, sudiarti t. a family history as dominant factors associated with dysmenorrhea among adolescents. journal of health and medical sciences. 2020 mar 10;3(1). |
|
Magar at, alam n. prevalence of dysmenorrhoeal pain and its impact on school performance: a cross-sectional study. |
|
Ali a, khalafala h, fadlalmola h. menstrual disorders among nursing students at al neelain university, khartoum state. sudan journal of medical sciences (sjms). 2020 jun 25. |
|
Dahlawi h, bukhari i, alshammari f, althaqib g, alhawasawi m, bashiri r, alruweili r. effect of dysmenorrhea on the academic performance among students studying in princess nourah bint abdulrahman university, riyadh. international journal of medicine in developing countries. 2021;5(2):588-94. |
|
Hashim rt, alkhalifah ss, alsalman aa, alfaris dm, alhussaini ma, qasim rs, shaik sa. prevalence of primary dysmenorrhea and its effect on the quality of life amongst female medical students at king saud university, riyadh, saudi arabia: a cross-sectional study. saudi medical journal. 2020 mar;41(3):283. |
|
Nigussie j, girma b, molla a, tamir t, tilahun r. magnitude of postpartum hemorrhage and its associated factors in ethiopia: systematic review and meta-analysis. |
|
Bazirete o, nzayirambaho m, umubyeyi a, karangwa i, evans m. investigating and modelling risk factors for primary postpartum haemorrhage among childbearing women in the northern province of rwanda: a case control study. |
|
Habitamu d, goshu ya, zeleke lb. the magnitude and associated factors of postpartum hemorrhage among mothers who delivered at debre tabor general hospital 2018. bmc research notes. 2019 dec;12(1):1-6. |
|
Kebede ba, abdo ra, anshebo aa, gebremariam bm. prevalence and predictors of primary postpartum hemorrhage: an implication for designing effective intervention at selected hospitals, southern ethiopia. plos one. 2019 oct 31;14(10):e0224579. |
|