Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2021)Volume 10, Issue 5
Background: Limited women’s autonomy in Maternal Health Care is the main underlying causes of poor utilization of maternal health care, and contributed in high maternal and children morbidity and mortality, low birth weight, and infertility. However, up to our search, in Ethiopia little emphasis has been placed on assessing factors associated with women autonomy. So this study was intended to assess status of Women’s Autonomy and its Associated Factors on Maternal Health Care utilization in west Ethiopia.
Method: A mixed community based cross-sectional study was employed from March 1-30, 2019. We selected 468 study participants through a multi-stage sampling method. Collected data were entered into Epi Data version 3.1 and exported to SPSS 21.0 for analysis. Statistical significance level was set at p < 0.05.
Result: Response rate of the study was 99.2%. This study revealed that 66.2% of women had high autonomy. Women who attended secondary and above education [AOR=3.22, 95% CI [1.40, 7.44]], those from richest family [AOR= 9.86, [95% CI [4.21, 23.08]], having favorable attitude toward maternal health care, [AOR:[3.34, 95%CI [1.89, 5.89]], being urban dwellers [AOR: 2.47,95% CI [1.212, 5.046]], early marriage [3.30[1.89, 5.75]], and women’s employment for payment [3.39[1.84, 6.23]] were showed significant association with high women’s autonomy on maternal health care utilization.
Conclusion: Even though there is a progress, still women autonomy regarding maternal health care utilization needs emphasis.
Women autonomy, Maternal health care utilization, Homa, Ethiopia
Women’s autonomy is defined through social, traditional and religious views of each society [1]. We call woman is autonomous when she can determine on events in lives, such as control over financial resources, freedom of movement and opportunity to take part in decisions making process even if men and other women opposed them [2].
Throughout the world women’s status often limits their capability to decide about many aspects of their own lives. It plays a central role for women from health care seeking and utilization up to choosing among various treatment choices [3]. Worldwide, about 830 women die every day from pregnancy- or childbirth-related complications. Almost all of these deaths happened in low and middle-income settings, and most of it could have been prevented [4]. And limited autonomy and control over their health decisions contribute a big share [3].
Women’s autonomy impacts maternal and child health [MCH] care utilization [5,6] . Besides increasing MCH, it also increases global food production, declines rates of malnutrition [7] and has long-term consequences on country development [8,9]. Along with different goals; sustainable development goal (SDG) provides an important framework to achieve gender equality and women empowerment. But according to the progress report from 45 countries in 2017, only 50% of married or in-union women aged 15-49 years make their own decisions regarding sexual relations, contraceptive use and general health care [10].
In developing countries women require male permission for seeking health care for themselves and their children, visiting their relatives, and even to go out of the compound. This restriction of women’s autonomy reduces access to key determinants of health which results in higher levels of health problems like, depression, malnutrition, health risks from greater numbers of pregnancies and childbirth [11]. In Ethiopia, 71% of married women take part in decision making but specifically, less than 50% of women in union decide for their own or their child’s health care [12]. Likewise, assets ownership rate is higher among men than women and 68.5% of employed women were unpaid workers [13].
Women autonomy is context based [14], however per our search no information regarding women’s autonomy on MHC utilization and its associated factors in West Ethiopia. In addition, despite of recent shift toward capturing population issues using qualitative and quantitative method [15], no single research was done in our country by mixed method on this topic of interest. So, this study aims to determine the status of women’s autonomy in west Ethiopia and exploring factors associated with it.
It is hoped that the findings of this study will provide an important information for program managers and policy makers at all levels to concentrate on the relevant factors of interest for possible intervention. Also used to sensitize the community to make them to take a part with a government by identify what things have to be done at community level. It is expected that it will add an immense value to achieve SDG. Furthermore, the finding of the study will supply information for further research.
Study Design, Setting and Period
Community-based cross-sectional study with both qualitative and quantitative methods was employed from March 1-30, 2019 in Homa district, western Wollega zone, Oromia Regional State. The study site is located to the west of Ethiopia at a distance of 496 km from Addis Ababa. The district has a total population of 52,560; females account for around 25,000 out of this 9,687 were women of Child bearing age group.
Population, Sample Size and Sampling Procedure
Study participants were, married women who gave birth in the past one year and had lived in the area for over 6 months. Single population proportion formula was used to calculate sample size with the assumptions of 95% confidence level, 5% margin of error and 41.4% (p =0.414) estimated proportion of women's autonomy on maternal and child health matters [12]. Since the source populations are below 10,000 finite population corrections were applied. Design effect of 1.5 and finally 10% non-response was added and the final sample size was 472. Multi stage sampling technique was employed by dividing the 13 kebeles in the district in to urban and rural. Then five rural and two urban kebeles were selected randomly. Sample size was distributed proportional to the size of the population in the selected kebeles to assure representativeness. To select study participants list of all women who gave birth in the past one year were obtained by reviewing health post registration of kebeles. Then sampling frame was done and study subjects were selected by simple random sampling technique (random number generated by computer).
For qualitative part, four FGD with 15 participants disaggregated by sex were selected purposively from husbands and wives and a total of 8 IDI with, kebele managers, head of district administrator, gender office head, HEW, Aba geda (leader of geda system) and religious leaders were held.
Data Collection Instrument and Process
After reviewing relevant literature, interviewer administered structured questionnaires, focus group discussion (FGD) and in-depth interview (IDI) guide were developed. The structured instrument contains socio-demographic and socioeconomic characteristics of the respondents, Knowledge of women on MHC, attitude of women towards MHC, media exposure, and women autonomy indicators [control over finance, decision making power, extent of freedom of movement]. FGD and IDI guide contains probing topics related to women’s autonomy. Data collection was conducted by three BSC and three diploma holders of female health care providers to address the women’s safety and confidentiality of the information, and two health officers were assigned as supervisors. The principal Investigator along with two assistants were conducted the qualitative study.
Operational Definitions and Measurements
Maternal health care: A care given for a mother during prenatal, natal, post-natal including family planning services.
Women autonomy: Calculated by computing from women’s control over finance, decision-making power and extent of freedom of movement. The overall score of the three constructs is 24. The sum value less than the mean was categorized as a low level of women's autonomy and the value greater than or equal to the mean was categorized as a high level of autonomy and coded 0 and1 respectively.
Decision making power: The ability of women to make decision regarding her own health where to seek for maternal health services.
Autonomy related to decision making was captured from the information on that usually has final say on: her own health care, Number of children, Use of contraception, antenatal care (ANC), preference of delivery site, and post-natal care (PNC). The possible responses for each items in decision making autonomy was respondent alone, respondent and husband/partner jointly, respondent and someone else, husband/partner alone & someone else. For each items the response was scored as: 2 if a woman made sole decision, 1 if she was involved with someone [husband/ partner or someone else] and 0 otherwise. The sum of the scores was representing an overall index of a woman decision-making power. The maximum score on decision making autonomy was 12 and those who scored mean and above were categorized as high decision making whereas those scored less than mean were categorized as women with low decision making power.
Freedom of movement: the women’s ability to move to health care facility without seeking permission from others (husband’s/ partner or someone else) for their own health care.
Autonomy regarding freedom of mobility was estimated from questions related to woman independent ability to leave the house without seeking permission from others to; 1. Go to health facility for her own health care, 2. Go out to visit family or relative, 3. Go outside this village for public meeting and 4. go to market. These items are with binary responses (yes or no). Hence, those with ‘yes’ response scored 1 while those with ‘no’ response scored 0. The maximum score on freedom of movement is four. Those with score of two and above were considered as high freedom of movement whereas those who scored less than two were categorized as low freedom of movement.
Control over financial resources: Women’s access to sources of money and ability to spend it without consulting anyone for their own health care concern.
The index for control over finance is composed of five items:
1. whether the woman had regular access to a source of money,
2. whether she state that she could spend this money without consulting anyone
3. who decides how the money she earned and
4. Who decides how the money her husband’s earnings are used, and
5. Who decides on major house hold purchasing?
A possible response for the first two items binary responses [i.e. yes or no] was scored as 1 if yes and 0 other wise. A possible response for the last three items are respondent alone, respondent and husband/partner jointly, respondent and someone else, husband/ partner alone & someone else. The response was scored as 2 if a woman made sole decision, 1 if she is involved with someone (husband/partner or someone else) and 0 otherwise. Since the total score on control over finance is 8, those women with a score of mean and above were considered as having high control over finance, while those women who scored less than mean had low control over finance.
Knowledge of women on maternal health care: A total of 19 questions were asked to assess women’s knowledge on maternal health care. After a composite score was done mothers who scored above 84% were considered as highly knowledgeable and moderately knowledgeable if they scored between 50-84% and Poor knowledgeable if they answered <50%.
Mothers’ attitude towards maternal health; To measure attitude of mothers towards MHC six questions with possible response of five Likert scale were asked. Those scored mean and above were considered as having favorable attitude and those who scored below the mean value were considered as having unfavorable attitude.
Nuclear Family Structure: Family consisting of married couples & their children; the children can be born or adopted.
Extended Family Structure: Nuclear family plus collateral kinship.i.e. Father, grandfather, mother uncles, aunts, nieces, nephews etc.
Wealth index: Households are given scores based on the number and kinds of consumer goods they own, ranging from a television to a bicycle or car, in addition to housing characteristics such as source of drinking water, and flooring materials.
Data Processing and Analysis: Data was entered and coded in Epi data version 3.1 and transported to SPSS version 21.0 for analysis. Principal component analysis [PCA] was used to compute the wealth status of households. Descriptive statistics was done to describe the study population concerning socio-demographic and other relevant variables. Multi co-linearity test was done to assess the correlation between independent variables and the variance inflation factor of a maximum of 2.1 was observed. Binary logistic regression analysis was done to select candidate variables for multivariable analysis and those variables having P-value <0.25 were fitted. Finally, Multivariable analysis with Adjusted Odds Ratio [AOR] was computed and P-Value of < 0.05 was considered as the criterion for statistical significance. The goodness of the model was assessed by Hosmer and Lemeshow test (p=0.658).
Data from the qualitative part were transcribed, translated to English, coded and categorized accordingly to main thematic areas manually. Then after repeatedly read the data, finally the findings were triangulated with the quantitative findings.
Data Quality Management
Questionnaires were initially prepared in English and then translated to Afan Oromo and then back-translated to English to check for consistency. We trained data collectors and supervisors for two days on objectives of the study and ways of data collection. Before actual data collection, we pretested the questioner in 5% of the total sample size in the neighbor district to check the internal consistency of items, to ensure clarity and logical sequence of the tool. Cronbach’s Alpha was computed to estimate internal reliabilities of the tools. During data collection supervisors checked completeness and consistency of administered questionnaires daily and timely corrections were made.
Reliability of Scale and Principal Component Analysis
Cronbach’s Alpha was computed for each of the three autonomy dimension separately and for an overall composite combining them. The estimated internal reliabilities for the control over finances 0.73, freedom of movement 0.83, and decision-making power measures were 0.88. The Cronbach's alpha coefficient for the three measures combined into a general index for autonomy was 0.73.
To use wealth index as explanatory variable, after minimum requirement for Principal component analysis (PCA) was checked, then from a total of 24 items included in the analysis three factors with eight items was created which could explain 65.3% total variance. Throughout the procedure variables with anti-image and communality of less than 0.5 and at the end, variables with complex structure were removed from analysis. Finally, outliers were detected and reliability test was computed and both values are fall inside the acceptable range, then newly created variable (wealth index) was taken as independent variable by ranked into five quantiles for further analysis.
Socio Demographic Characteristics of the Study Participants
Of 472 randomly selected women, 468 participated in the study yielding a response rate of 99.15% with a mean (±SD) age of 26.78 (±5.2) years. About 63.4% of the study participants were in the age ranges of 20-29 years. Ninety-seven percent of women were Oromo by ethnicity and 70.7% are protestant in religion. Over 70% of study participants were from rural areas, nearly half of them had attended primary education and 82.9% of them reported that their husbands had formal education. Majority of the women [89.3%] were living in nuclear family structure, and 39.5% of them reported that they married at age of less than 18. Most [24.8%] of women were residing in a family with poorest quintile of wealth index (Table 1).
| Characteristics | Categories | Frequency(percent) |
|---|---|---|
| Age | <20 20-24 25-29 30-34 ≥35 |
47(10) 112(23.9) 185(39.5) 72(15.4) 52(11.1) |
| Ethnicity | Oromo Others® |
455(97.2) 13(2.8) |
| Religion | Protestant Orthodox Muslim |
331(70.7) 95(20.3) 42(9) |
| Residence | Urban Rural |
139(29.7) 329(70.3) |
| Wealth index | Poorest Poor Medium Rich Richest |
116(24.8) 76(16.2) 88(18.8) 81(17.3) 107(22.9) |
| Educational Status of respondent | No formal education Primary education Secondary education (9-12) College and above(12+) |
95(20.3) 225(48.1) 96(20.5) 52(11.1) |
| Employment status of respondent | Employed Not employed |
300(64.1) 168(35.9) |
| Payment status of respondents | Paid Not paid |
228(76.1) 72(23.9) |
| Educational Status of husband | No formal education Primary education Secondary education College and above |
80(17.1) 197(42.1) 106(22.6) 85(18.2) |
| Employment status of husband | Employed Not employed |
281(60.0) 187(40.0) |
| Marriage type | Monogamous Polygamous |
443(94.7) 25(5.3) |
| Family Structure | Nuclear Extended |
418(89.3) 50(10.7) |
| Number of children surviving. | ≤2 3-4 ≥5 |
246(52.6) 160(34.2) 62(13.2) |
| family size. | ≤5 >5 |
335(71.6) 133(28.4) |
Table 1: Socio demographic profile of (n=468) and reproductive history of study participants in Homa district, west Ethiopia, March 2019.
Distributions of the responses to the women autonomy related questions.
Nearly half (54.5%) of women were decided about their own health care independently, 77.8% of them had joint decisions regarding contraception use and 17.5% hadn’t take part in decision over desired number of children (Table 2). Most of the participants in both FGD and IDI agreed that even if joint decision making becomes familiar in the community there is a situation in which women's decision-making power on maternal health care is violated. Also, they mention that women are not 100% free to decide on their health.
| Autonomy questions | Frequency(percent) | |||
|---|---|---|---|---|
| Independent decision | joint decision | not involved in decision |
||
| final say on your Health care | 255(54.5) | 185(39.5) | 28(6.0) | |
| final say on desired number of children | 43(9.2) | 343(73.3) | 82(17.5) | |
| final say on your contraception utilization | 35(7.5) | 364(77.8) | 69(14.7) | |
| final say on ANC utilization | 229(48.9) | 227(48.5) | 12(2.6) | |
| final say on preference of delivery site | 100(21.4) | 315(67.3) | 53(11.3) | |
| final say on PNC utilization | 245(52.4) | 212(45.3) | 11(2.4) | |
| On the use of wife’s money | 70(22.3) | 220(70.1) | 24(7.6) | |
| On the use of husband’s money | 5(1.1) | 332(70.9) | 131(28) | |
| Major household sales & purchases | 9(1.9) | 379(81.0) | 80(17.1) | |
| Yes | No | |||
| Freedom to go health facility for your own health care | 319(68.2) | 149(31.8) | ||
| Freedom to visit family or relative | 235(50.2) | 233(49.8) | ||
| Freedom to go market places | 307(65.6) | 161(34.4) | ||
| Freedom to go for public meeting | 169(36.1) | 299(63.9) | ||
Table 2: Distributions of the respondents’ responses to autonomy related questions.
“There is mutual discussion and understand in my family to decide on FP, number of children desired, ANC utilization and other service” (35yrs husband, FGD).
“In contrast, health extension worker participated in IDI says to share you a pain-full history of one mother, she is a mother of 7 children, and she decided to stop having any more children but her husband refused her decision. Since she had no option she conceived and finally she died on giving her 8th birth soon she arrived a hospital. (26yrs HEW, IDI). Also, a 33years old religious leader says “our culture violates women's autonomy. For instance, on FP even though she is counseled by health care provider, she gives a high credit for a husband to decide and prefers to be subordinate,”
Religion and impact of the past culture remains affecting women autonomy on their health matters.
“For me more than 80% of our women are exercising their autonomy on their own health, but regarding decision on desired number of children, and contraceptive utilization, women autonomy is restricted in some religious area” (42 yrs. district administrator, IDI).
“Due to the pressure from previous culture there is no sense of autonomy in the women. …. they give a high credit for their husband to decide and they prefer to be subordinate” (32 yrs. head of gender office).
Around two-thirds [67.1%] of women had regular access to a source of money, of which 35.5% of them reported that they are autonomous to use the money without consulting others. Nearly two percent (1.9%) of women were decide alone about large item purchase for households and most (81%) of them had joint decision.
Participants in the qualitative study also mentioned that financial control is more in the hands of husbands (male). Especially women side agrees that due to lack of means of income and lack of control over house hold income, their autonomy is limited.
One of the FGD female discussant discussed that “I don’t have my own income. Regarding large-item purchasing my husband tells me only for the sake of informing after finishing the procedure of buying and selling” (24 yrs woman, FGD). Similarly, IDI participants also strength the idea, “Sometimes, its observable when HH income is decided only by husbands. Because the main source of income in this area is coffee and a major part of coffee is owned by husband” (32 yrs. old female gender office head).
“…... to Purchase big item they might discuss together but the final say is that of husband. If it is decided by wife, he feels inferiority in the society “(33yrs religious secretary, IDI).
Regarding freedom of movement around 31.8% of women need an additional husband's or someone’s decision to go to the health facility for their health care (“Table 2”). Most of FGD and IDI participants agree that women should have to wait for their husband’s permission to visit health facilities if not family relation might be disturbed to the worst of divorce.
A 44 year’s old male FGD participant told that “Women’s should keep God’s order and wait for husband’s consent before going anywhere. If they move without informing, it results in a great problem even divorce”.
“Based on our religion guide, the husband is the head of the house. So, it’s not allowed for women to move anywhere without getting permission from her husband.” (33yrs religious leader, IDI).
Dimensions of Women’s Autonomy
The mean (±SD) score of women on decision making power index was 7.4 (±2.5) out of a possible maximum of 12. The mean (±SD) score of women on freedom of movement was 2.2 (±1.2) out of 4. The mean (±SD) score of women on control over financial resource was 3.37(±1.7530) out of 8. The mean (±SD) score of overall index women’s autonomy was 12.97 (±4.54) out of a possible maximum of 24 score and 66.2% of the women had higher autonomy (Figure 1)
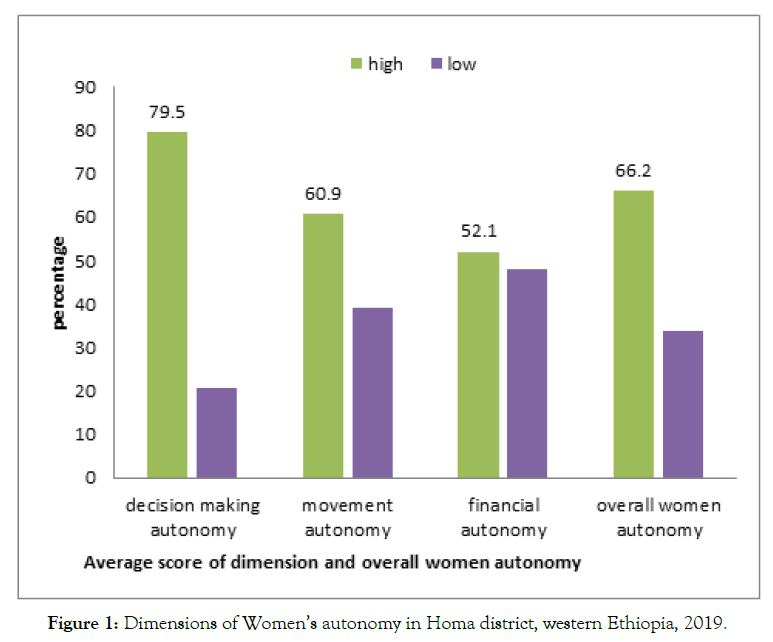
Figure 1. Dimensions of Women’s autonomy in Homa district, western Ethiopia, 2019.
Logistic Regression Estimates of Factors Associated With Women Autonomy
Primarily binary logistic regression analysis was done to identify candidate variables for multivariable logistic regression and 11 variables [current age, age at marriage, place of residence, wealth index, educational status of respondents, employment status of couples, payment status, knowledge and attitude towards maternal health care] were selected. In multivariable logistic analysis; educational status of respondent, age at marriage, place of residence, payment status of respondents, wealth index, and attitude towards maternal health care were found to be positively and significantly associated with the level of women autonomy.
Women who attended secondary and above education had 3.2 times higher odds of high autonomy than those who haven’t formal education (AOR=3.221, 95% CI (1.395, 7.439]).
“…. Lack of education especially on women side and culture of school dropout at low level affecting autonomy of women in our district” (23yrs kebele manager, IDI).
“some of our women, especially those who haven’t education still a victim of the past culture, due that they are not confident enough to exercise autonomy at required level, rather they prefer to be husband subordinate” (42 yrs. district administration head, IDI).
Women who have favorable attitude towards maternal health care services were 3.3 times more likely to be highly autonomous than mothers with unfavorable attitude (AOR :(3.338, 95%CI (1.891, 5.893)).
“Mainly women are not interested to attend women conference, public meeting, and other opportunities created by the government to improve their knowledge, attitude towards maternal health care, build their self-confidence. This could affect their level of autonomy on maternal health care utilization” (26yrs HEW, IDI)
Women who reside in urban had 2.5 times higher odds of having high autonomy than their counterparts in rural areas ([AOR: 2.473, 95% CI (1.212, 5.046)). Women who married at age of eighteen and above had 3.3 times higher odds of high autonomy than those married at early age [[AOR= 3.296 95% CI(1.887, 5.754) (Table 3).
| Variables | Women autonomy | COR(95%CI) | AOR(95%) | P-value | |
|---|---|---|---|---|---|
| High | Low | ||||
| Age at marriage <18 ≥18 |
84(53.2) 74(46.8) |
84(27.1) 226(72.9) |
1 3.054[2.046, 4.558] |
3.296(1.887, 5.754) |
0.001⃰ |
| Residence Rural Urban |
142(89.9) 16(10.1) |
187(60.3) 123(39.7) |
1.0 5.838(3.319, 10.268) |
2.473(1.212, 5.046) |
0.013⃰ |
| Wealth index Poorest Poor medium rich richest |
70(44.3) 34(21.5) 23(14.6) 17(10.8) 14(8.9) |
46(14.8) 42(13.5) 65(21.0) 64(20.6) 95(30.0) |
1 1.880[1.047,3.376] 4.301[2.351, 7.866] 5.729[2.986, 10.990] 10.109[5.153,19.831] |
2.336(1.089, 5.011) 4.832(2.245, 10.400) 7.330(3.220, 16.686) 9.858(4.211, 23.082) |
0.029⃰ 0.001⃰ 0.001⃰ 0.001⃰ |
| Payment status of respondents not paid Paid |
30(51.7) 28(48.3 |
42(17.3) 201(82.7) |
1 5.128[2.778, 9.466] |
3.386(1.840, 6.233) |
0.001⃰ |
| Educational status of respondents no formal education primary education secondary and above |
58(36.7) 79(50.0) 21(13.3) |
37(11.9) 146(47.1) 127(41.0) |
1 2.897[1.766, 4.752] 9.480[5.105, 17.606] |
2.618(1.351, 5.071) 3.221(1.395, 7.439) |
0.004⃰ 0.006⃰ |
| attitude towards MHC unfavorable favorable |
115(72.8) 43(27.2) |
73(23.5) 237(76.5) |
1 8.683[5.605, 13.451] |
3.338(1.891, 5.893) |
0.001⃰ |
Table 3: Bivariate and multivariable regression analysis of factors associated with women's autonomy on maternal health care utilization in Homa district, west Ethiopia, 2019.
This study reveals that autonomy decreases with wealth decrement. Women in the richest quantiles had 10 times (AOR= 9.9,(95% CI (4.21, 23.08)), women from the rich family had 7 times (AOR=7.3 (95% CI (3.2, 16.69), women from medium wealth quantiles had 5 times (AOR= 4.8 (95% CI (2.25, 10.40), and women from poor wealth quantiles had 2 times (AOR=2.34(95% CI (1.09, 5.01)) higher odds of having high autonomy than women living in the poorest families. Women who get paid for their employment had 3.4 times higher odds of having high autonomy than women who don’t get paid for their employment (AOR=3.39(95% CI (1.84, 6.23) (Table 3).
High proportion of women in our district are house wives, due that they are not participating in income generating activities. This made them to be dependent financially on husbands (24yrs kebele manager, IDI).
In this study, 66.2%, of women exercised high autonomy. This finding is in line with studies conducted in Nepal [16] which showed that about 67% of women had high autonomy but higher than a study done in southeast Ethiopia, in which 41.4% of women had high autonomy [12]. This difference might be since there is a time gap between the study, measures taken to promote women's empowerment and gender equality through different interventions have become strengthened over time [17–19].
Finding of this study revealed that those who attained primary education were 2.62, and those who attained secondary and above education were 3.22 times more likely to have high autonomy than women without formal education. Studies done in Dabat of Ethiopia [20], Nepal [21,22], Nigeria [23] and Ghana [24] reported consistent findings. This is mainly because educated women are more aware of their right to free choice and might be more capable of exercising their will as far as health care decision is concerned, either alone or with their partners [24], education may impart feelings of self-worth and self-confidence, which are more important features in bringing about changes in health-related behavior than exposure to relevant information [25].
The study shows that, women who married at 18 and above were 3.3 times more likely to have high autonomy than women married while they were minors. This result is in line with the study done in Egypt [26], and contradicts the report from Albania [27]. The explanation for the difference is the age classification used in the studies, which is 20 years for the Albania and 18 years in this study. This finding implies that delaying age at marriage provides more opportunities for education, employment, and participation in the choice of a husband [28]. This will enhance women’s power within the households, her ability to negotiate with husbands and other household members and her involvement in decision-making after marriage [28].
In our analysis women from the richest, rich, medium and poor quintile of wealth index were about 10,7,4 and 2 times more likely to be highly autonomous than women from the poorest quintile households, respectively. This finding is supported by different studies done in Ethiopia and other countries [20,21,29,30]. This study reveals that women who get paid for their employment were more likely to have high autonomy than those who don’t get paid for their work.
Our analysis shows that, having a favorable attitude towards maternal health service utilization is also a factor for women’s autonomy on maternal health service. This finding is in line with the finding of a study done in Ethiopia [3]. This result strengthens the idea that implies, women who had favorable attitudes towards maternal health care services could easily influence their husbands and significant others [29].
Triangulation of quantitative and qualitative methods and the dimensions used to assess autonomy are the strength of this study. A relative measure of socio-economic status [wealth index] was computed. There was a high response rate for the study. Limitation of the study was recall bias and autonomy was not specific for services like for Antenatal care, delivery, post-natal care or family planning.
Women in the Homa district have relatively high autonomy. Educational status of women, women employed for payment, wealth index of household, age at first marriage, attitude towards MHC and place of residence are factors significantly associated with women's autonomy in the study area. This factor was supported by the qualitative finding too. To improve women's autonomy emphasis should have to be given on the above factors, especially on education and financial security of women.
Ethical Approval and Consent to Participate
Jimma University institutional review board approved the study (reference, IHRPGD/720/2019). To proceed further, we took a letter of permission from local authorities. Informed consent was obtained from study participants after explaining the purpose, procedure, duration, and benefits of the study. Women who were not willing to engage in the study and those who want to stop interview at any time were allowed to do so.
Availability of data and materials: The one in need of data of the study can contact the corresponding author on reasonable request.
Competing interest: All authors declared that there is no conflict of interest.
Funding: I, the corresponding author, have received a limited funding from Jimma University, Jimma, Ethiopia. This funding is part of post graduate students support program which covers only travel expenses. We declare that the funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Authors’ Contribution
Aboma. D, involved from the inception to design, participated in data collection, analysis, interpretation, and drafting the manuscript and reviewing it.
Abebe G/M, assisted in designing, analysis, interpretation, manuscript preparation and critically reviewing the manuscript
Tadesse Sime, assisted in designing, analysis, interpretation, manuscript preparation and critically reviewing the manuscript
Rahma A, assisted in designing, analysis, interpretation, manuscript preparation and critically reviewing the manuscript.
We acknowledge the support of Jimma University for reviewing the ethics. We are thankful to all study participants for giving their time to participate in our study.
Citation: Diriba A, Gebremariam A, Ali R (2021) Women’s autonomy on maternal health care utilization and its associated factors in western Ethiopia, a community based mixed cross-sectional study, 2019. J Women's Health Care 10:530. doi:10.35248/2167-0420.21.10.530.
Received: 19-Apr-2021 Accepted: 12-May-2021 Published: 18-May-2021 , DOI: 10.35248/2167-0420.21.10.530
Copyright: © 2021 Diriba A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.