
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 12
Background: The lung ultrasound score was predictive for prolonged intensive care stay in pediatric cardiac surgery, so we evaluate the role of the lung ultrasound score in predicting the length of postoperative intensive care stay after adult cardiac surgeries.
Methods: Our study collected data from 191 adult patients admitted to the ICU following elective cardiac surgery. Lung ultrasound examinations were done after 12 hours of ICU admission, and six lung areas were examined on each side, scoring each area. The primary outcome is to find the association between the total LUS score and the ICU length of stay in days.
Results: We found a strong correlation between LUS total score and prolonged intensive care stay (more than 3 days) with a median of 3 and an IQR of 3 in patients with short ICU stay compared to a median of 6.5 and an IQR of 8 in patients with prolonged ICU stay with p-value less than 0.001. The total LUS score was also significant when implemented as a continuous variable with other predictors in the multivariate logistic regression model with an adjusted odds ratio of 1.66 and a p-value of <0.001.
Conclusion: The postoperative total lung ultrasound score after cardiac surgery is helpful in the Prediction of prolonged intensive care stay and hospital stay as there is a strong correlation between both.
Lung ultrasound score; ICU; Cardiac surgery; Hospital stay
The Prediction of the length of critical care stay after adult cardiac surgeries is an area of debate. Many predictors for open-heart surgery outcomes have been studied in past years, including The Society of Thoracic Surgeons (STS) risk score and the EuroSCORE II, preoperative clinical condition, associated chronic diseases, type of surgery, age, duration of cardiopulmonary bypass, Brain Natriuretic Peptide (BNP) and cystatin-C [1,2].
Being easy, bedside, non-expensive, noninvasive, and radiationfree, there has been a growing interest in the implementation of lung ultrasound in critical care management in the last decade; cardiac surgery was not an exception, including both adult and pediatric surgeries [3].
A Lung Ultrasound Scan (LUS) can diagnose pneumothorax, pulmonary edema, pleural effusions, and consolidation [4]. Moreover, it improves the clinical approach to shock and cardiorespiratory failure, with the lung component forming a pivot part of the patient's overall assessment [3]. LUS was correlated with Acute Respiratory Distress Syndrome (ARDS) severity and predicted mortality [5]. It also provides reliable dynamic monitoring for regional lung aeration changes in cases such as prone positioning, Positive End-Expiratory Pressure (PEEP), and fluid loadings [6]. A lung ultrasound score of more than 13 measured after a clinically successful spontaneous breathing trial during weaning from mechanical ventilation is predictive of extubation failure [7].
A recent study described the use of a novel postoperative lung ultrasound score scanning for B lines which denote subpleural interstitial edema in various lung regions, to predict critical care length of stay after pediatric cardiac surgeries [2]. Although adult cardiac surgery has a high risk of postoperative pulmonary complications, the implication of such a score in adult cardiac surgeries was not reported in the literature until now.
We hypothesized that the lung ultrasound score could predict the length of postoperative ICU stay after adult cardiac surgeries. Hence, the current study evaluates the role of the lung ultrasound score in predicting the Length of postoperative ICU stays after adult cardiac surgeries.
This prospective observational study was conducted at Fayoum university hospital from August 2020 to March 2022, following the tenets of the Declaration of Helsinki. The ethical review board approved the study design of Fayoum University Hospital (D 230), and the eligible participants signed a detailed informed consent. The study was conducted after registration on ClinicalTrials.gov (NCT04499027; principal investigator: Mohamed Ahmed Hamed; date of registration: 05/08/2020, no protocol amendment or study changes after trial start). This study adheres to the applicable CONSORT guidelines.
One hundred ninety-one patients above 18 years and scheduled for elective cardiac surgery for valve replacement or adult congenital (VSD or ASD) via median sternotomy were included.
The exclusion criteria were subjects with inadequate acoustic windows or preliminary examinations, patients with emergency surgeries, thoracic deformities, or preexisting pulmonary pathology.
Anesthetic technique
All patients were preoperatively examined and investigated by complete blood count, coagulation profile, renal functions, and electrolytes. Electrocardiography, chest x-ray, and echocardiography were routinely done. Coronary angiography and carotid arterial duplex could be requested on-demand.
Patients were premedicated by intramuscular injection of 10 mg morphine on the morning of the operation. Before induction of anesthesia, a five-lead electrocardiography system was applied to monitor heart rate, rhythm, and ST segments (leads II and V5). A pulse oximeter probe was attached, and a peripheral venous cannula was placed. A 20 G cannula was inserted into either right or left radial artery under local anesthesia to measure arterial pressure and blood sampling. After pre-oxygenation, general anesthesia was induced by midazolam 2 mg, fentanyl (10 μg.kg-1), propofol (3 mg.Kg-1), followed by atracurium (0.5 mg.kg-1).
The trachea was intubated; patients were mechanically ventilated with oxygen in the air, and ventilation parameters were adjusted to achieve normocarbia. An esophageal temperature probe and a urinary catheter also had been placed.A triple-lumen central venous catheter was inserted via the right internal jugular vein for drug infusion.
Anesthesia was maintained by inhaling Isoflurane 0.4 to 1% and atracurium infusion of 0.5 mg.kg-1.h-1 for continued muscle relaxation. During extracorporeal circulation, patients received propofol infusion at 50-100 μ.kg-1.min-1. In addition to atracurium infusion.
Before initiation of CPB, the patients received intravenous heparin (300-500 units.kg-1 body weight) to achieve an ACT>480s. CPB was instituted via an ascending aortic cannula and a two-stage right atrial cannula. Before, during (pump blood flow: 2.4 l/min/m2), and after CPB, mean arterial pressure was adjusted to exceed 60 mmHg. Cardiac arrest had been achieved with cold ante-grade blood cardioplegia. Lactate-enriched Ringer's solution was added to the CPB circuit to maintain reservoir volume when needed and packed red blood cells would be added when hemoglobin concentration decreased to less than 7 g.dl-1. After the patient rewarming to 37°C, separation from CPB, reversal of heparin by protamine sulfate (1:1), and sternal closure was achieved.After skin closure and wound dressing, patients were transferred to the intensive care unit intubated with manual ventilation and complete monitoring during transfer.
Intensive care
Tracheal extubation was performed when the patient met the following criteria: awake or arousable, hemodynamically stable, no ongoing active bleeding, warm extremities, no electrolyte abnormalities, no or minimal inotropic support and a satisfactory arterial blood gas with a FiO2<0.5, Ventilator pressure support reduced to 10 CmH2O with Positive End Expiratory Pressure (PEEP) 5-7 CmH2O. ICU management and decisions were left to the intensivist responsible for postoperative cardiac critical care.
Patients were discharged from ICU when the following criteria were met: Awake patient with SpO2 <90% at FIO2>0.5 by facemask, adequate cardiac stability, no intravenous inotropic or vasopressor supportive therapy, no hemodynamically significant arrhythmia, not dependent on epicardial external pacing no major bleeding, i.e., chest tube drainage less than 50 ml/h, urine output of more than 0.5 ml/kg/h and no vital threats to other organ systems such as kidneys and liver [8].
Lung Ultrasound Scan (LUS)
All patients were examined at 12 hours postoperatively using a convex ultrasound probe (Philips clear value 350, Philips Healthcare, Andover MAO1810, USA, Machine ID: 1385); any other LUS was done upon demand.
An experienced radiologist performed all LUS examinations. For each hemithorax, three main areas (anterior (Ant), lateral (Lt), and posterior (Post)) marked by the para-sternal, anterior axillary, and posterior axillary lines were identified. Then, each one was divided into upper and lower halves, making a sum of 6 different quadrants for each side: anterior superior, anterior inferior, lateral superior, lateral inferior, posterior superior, and posterior inferior. For each quadrant, a score was assigned based on B-lines which are defined as discrete laser-like vertical hyper -echoic reverberation artifacts arising from the pleural line and extend to the bottom of the screen without fading, moving synchronously with lung sliding (previously described as comet tails) , indicating subpleural interstitial edema(2,7):(0) normal aeration: A-lines with lung sliding or fewer than two isolated B lines; (1) moderate loss of lung aeration: well-defined, multiple B lines ; (2) severe loss of lung aeration: multiple coalescent B lines; and (3) complete loss of lung aeration or lung consolidation [2,7].
This was used to calculate the total LUS score (calculated as a sum of all quadrants' scores) and individual areas' scores (Ant, Lt, and Post).
Measured parameters
The primary outcome is to evaluate the role of the postoperative lung ultrasound score in predicting the Length of postoperative ICU stays after adult cardiac surgeries in days; a prolonged ICU stay will be considered more than three days. Secondary outcomes included: Baseline characteristics, including patient age, sex, Body mass index, and Euro SCORE II (calculated preoperatively using different variables, which are age, gender, renal impairment, extracardiac arteriopathy, poor mobility, previous cardiac surgery, chronic lung disease, critical preoperative state, presence of insulin-dependent diabetes, NYHA classification, Canadian Cardiovascular Society (CCS) class, left ventricular function, recent myocardial infarction, pulmonary hypertension, urgency and weight of the operation and whether thoracic aorta is involved in the surgery [9]. Scores were calculated using an online calculator on the QxMD website. LUS and Postoperative total LUS score, individual lung areas score, extubation time, hospital length of stay in days (prolonged hospital stay if more than seven days), and in- hospital mortality [10].
Statistical analysis
As there was no previous similar study when designing our study protocol to calculate the sample size, we performed an external pilot study that included 25 patients, with its results not included in the full scale of our research. The minimal sample size of patients was 191 needed to get power level 0.80, alpha level 0.05 (two-tailed), and 0.20 as expected β (slope of regression line) to find the association between total LUS score and critical care Length Of Stay (ICU LOS) in days.
Descriptive statistics are presented as minimum, maximum, mean, and standard deviation for numerical variables, while numbers and percentages are used for categorical variables. In addition, median and IQR are used for the LUS score in each quadrant.
An alternative model ROC curve was used to categorize the lung ultrasound score into two categories. Independent samples t-test, Mann-Whitney test, and Chi-Square test were used to compare patients with long and short ICU stay depending on the nature of the compared variables. The same tests were used to compare short and long hospital stays. Multiple logistic regressions were used to study the association between long ICU stay or long hospital stay with other factors. All statistically significant variables in the univariate analysis were included in the model, and the final model was reached using the backward elimination method. For each predictive model, a nomogram was created. The performance of different models was compared using the area under the curve.
IBM SPSS 28 for windows software was used for the analysis, Stata version 16 was used for nomogram creation, while MedCalc version 20 was used for the ROC curve generation and comparison. P-value <0.05 is considered statistically significant.
For this study, 207 patients were assessed for eligibility based on the inclusion and exclusion criteria. Nine patients were excluded; two cases had emergency surgeries, and seven were due to preexisting pulmonary disease. The remaining 198 patients were allocated to examination; 191 patients received allocated examination. However, seven did not receive an allocated examination because one patient died intraoperatively, two died early in intensive care before an ultrasound examination, and four had a poor acoustic window (Figure 1).
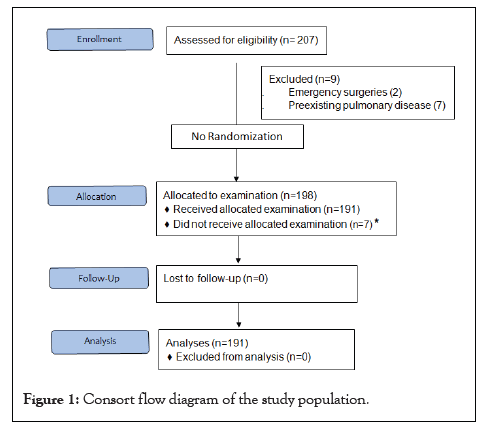
Figure 1: Consort flow diagram of the study population.
Patient characteristics are shown in Table 1. Among our patients, 48.7% had short ICU stays (3 days or less), while 51.3% had long ICU stays (more than three days). However, 48.2% of the patients had short hospital stays (7 days or less), while 51.8% had long hospital stays (more than seven days). For extubation time, 36.1% had early extubation (6 hours or less), while 63.9% had late extubation (more than six hours). The mean total LUS score for patients included in the study was (5.45 ± 4.9).
| Sample size,n | 191 |
|---|---|
| Sex, n (%) | |
| Male | 108 (56.5) |
| Female | 83 (43.5) |
| Mean age (SD) in (years) | 57.36 (8.95) |
| Mean BMI (SD) in kg/m2 | 29.44 (4.40) |
| Planned operation | |
| CABAG, n (%) | 121 (63.35) |
| Valvular | 70 (36.65) |
| Comorbidities | |
| HTN,n (%) | 38 (19.9) |
| Diabetes | 38 (19.9) |
| Mean Euro score (SD) | 1.41 (1.65) |
| Mean CPB time (SD) in min | 104.11(27.46) |
| Inotropes | |
| Single inotrope, n (%) | 108 (56.54) |
| Multiple inotropes, n (%) | 83 (43.46) |
| Postoperative complications (total) n (%) | 48 (25.13) |
| Mortality n (%) | 11 (5.8) |
| Short ICU stay (3 days or less) n (%) | 93 (48.7) |
| Long ICU stay (More than 3 days) n (%) | 98 (51.3) |
| Early extubation (6 hours or less) n (%) | 69 (36.1) |
| Late extubation (more than 6 hours) n (%) | 122 (63.9) |
| Short hospital stay (7 days or less) n (%) | 92 (48.2) |
| Long hospital stay (More than 7 days) n (%) | 99 (51.8) |
| Total LUS score, mean (SD) | 5.45 (4.9) |
Abbreviations: SD, Standard Deviation; n, number; BMI, Body Mass Index; CABG, Coronary Artery Bypass Grafting; CPB, Cardio-Pulmonary Bypass; HTN, Hypertension; ICU, Intensive Care Unit; LUS, Lung Ultrasound Scan.
Table 1: Patient characteristics.
To find the relation between LUS scores and critical care LOS and hospital LOS, we compared LUS scores of different quadrants among patients with short critical care LOS versus those with long critical care LOS. LUS scores were significantly higher in patients with a long ICU stay. Also, the total LUS score was significantly higher for patients with long ICU stay (median, IQR=6.5, 8) compared to (3, 3) for those with short ICU stay. Similar findings were noticed regarding the duration of the hospital stay (Table 2).
| For ICU length of stay | ||||||
|---|---|---|---|---|---|---|
| Short (3 days or less) | long (More than 3 days) | p-value | ||||
| Median | IQR | Median | IQR | |||
| RAS | 0 | 0 | 0 | 1 | 0.001 | |
| RLS | 0 | 0 | 0 | 1 | <0.001 | |
| RPS | 0 | 0 | 1 | 1 | <0.001 | |
| RAI | 0 | 0 | 1 | 1 | <0.001 | |
| RLI | 0 | 1 | 1 | 1 | <0.001 | |
| RPI | 0 | 1 | 1 | 2 | <0.001 | |
| LAS | 0 | 0 | 0 | 1 | <0.001 | |
| LLS | 0 | 0 | 0 | 1 | 0.003 | |
| LPS | 0 | 0 | 1 | 1 | <0.001 | |
| LAI | 0 | 0 | 1 | 1 | <0.001 | |
| LLI | 0 | 0 | 1 | 1 | <0.001 | |
| LPI | 0 | 1 | 1 | 2 | <0.001 | |
| Total | 3 | 3 | 6.5 | 8 | <0.001 | |
| For hospital stay | ||||||
| Short (7 days or less) | long (More than 7 days) | p-value | ||||
| Median | IQR | Median | IQR | |||
| RAS | 0 | 0 | 0 | 1 | 0.002 | |
| RLS | 0 | 1 | 0 | 1 | 0.002 | |
| RPS | 0 | 0 | 0 | 1 | <0.001 | |
| RAI | 0 | 0 | 1 | 1 | <0.001 | |
| RLI | 0 | 1 | 1 | 1 | <0.001 | |
| RPI | 0 | 1 | 1 | 2 | <0.001 | |
| LAS | 0 | 0 | 0 | 1 | <0.001 | |
| LLS | 0 | 0 | 0 | 1 | 0.012 | |
| LPS | 0 | 0 | 1 | 1 | <0.001 | |
| LAI | 0 | 0 | 0 | 1 | <0.001 | |
| LLI | 0 | 0 | 1 | 1 | <0.001 | |
| LPI | 0 | 1 | 1 | 2 | <0.001 | |
| Total | 3 | 2 | 6 | 8 | <0.001 | |
Abbreviations: ICU, Intensive Care Unit; RAS, Right Anterior Superior; RLS, Right Lateral Superior; RPS, Right Posterior Superior; RAI, Right Anterior Inferior; RLI, Right Lateral Inferior; RPI, Right Posterior Inferior; LAS, Left Anterior Superior; LLS, Left Lateral Superior; LPS, Left Posterior Superior; LAS, Left Anterior Superior; LLS, Left Lateral Superior; LPS, Left Posterior Superior; LAI, Left Anterior Inferior; LLI, Left Lateral Inferior; LPI Left Posterior Inferior.
Table 2: Comparison between patients with long and short ICU stay and hospital stay regarding LUS score of different quadrants.
An alternative model ROC curve was used to categorize the lung ultrasound score into two categories. First, for both long ICU stay and long hospital stay, A score of >4 was chosen. For the long ICU stay, it had a sensitivity of 66.3% and a specificity of 88.2%; for the long hospital stays, it had a sensitivity of 64.6% and a specificity of 87.0%. Alternative cut-off points of total LUS for both long ICU and hospital stays with corresponding sensitivity and specificity (Table 3).
| For a long ICU stay | ||||
|---|---|---|---|---|
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI |
| ≥ 0 | 100 | 96.3-100.0 | 0 | 0.0-3.9 |
| >0 | 96.94 | 91.3-99.4 | 15.05 | 8.5-24.0 |
| >1 | 92.86 | 85.8-97.1 | 24.73 | 16.4-34.8 |
| >2 | 86.73 | 78.4-92.7 | 48.39 | 37.9-59.0 |
| >3 | 78.57 | 69.1-86.2 | 69.89 | 59.5-79.0 |
| >4 | 66.33 | 56.1-75.6 | 88.17 | 79.8-93.9 |
| >5 | 55.1 | 44.7-65.2 | 95.7 | 89.4-98.8 |
| >6 | 50 | 39.7-60.3 | 100 | 96.1-100.0 |
| >23 | 0 | 0.0-3.7 | 100 | 96.1-100.0 |
| For a long hospital stay | ||||
| ≥ 0 | 100 | 96.3-100.0 | 0 | 0.0-3.9 |
| >0 | 94.95 | 88.6-98.3 | 13.04 | 6.9-21.7 |
| >1 | 89.9 | 82.2-95.0 | 21.74 | 13.8-31.6 |
| >2 | 84.85 | 76.2-91.3 | 46.74 | 36.3-57.4 |
| >3 | 76.77 | 67.2-84.7 | 68.48 | 58.0-77.8 |
| >4 | 64.65 | 54.4-74.0 | 86.96 | 78.3-93.1 |
| >5 | 53.54 | 43.2-63.6 | 94.57 | 87.8-98.2 |
| >6 | 48.48 | 38.3-58.7 | 98.91 | 94.1-100.0 |
| >7 | 47.47 | 37.3-57.8 | 100 | 96.1-100.0 |
| >23 | 0 | 0.0-3.7 | 100 | 96.1-100.0 |
Abbreviations: ICU, Intensive Care Unit.
Table 3: Alternative cut-off points of total LUS for both long ICU stay and long hospital stay with corresponding sensitivity and specificity.
Associations between multiple variables and LOS (critical care and hospital) were studied, and significant variables were presented (Table 4).
| Group | Short (3 days or less) | long (More than 3 days) | P-value | ||
|---|---|---|---|---|---|
| Mean age (SD) | 53.49 | 8.25 | 61.03 | 8.02 | <0.001 |
| Mean Euro score (SD) | 0.91 | 0.45 | 1.88 | 2.16 | <0.001 |
| Mean ICU Lactate (SD) | 3.42 | 1.98 | 6.26 | 3.22 | <0.001 |
| CPB time | 95.16 | 18.85 | 112.6 | 31.47 | <0.001 |
| Complications n (%) | <0.001 | ||||
| No | 87 (93.5) | 56 (57.1) | |||
| Yes | 6 (6.5) | 42 (42.9) | |||
| Group | Short (7 days or less) | long (More than 7 days) | P-value | ||
| Mean Age (SD) | 53.76 | 8.35 | 60.71 | 8.19 | <0.001 |
| Mean Euro score (SD) | 0.94 | 0.49 | 1.85 | 2.16 | <0.001 |
| Mean ICU Lactate (SD) | 3.43 | 1.91 | 6.21 | 3.27 | <0.001 |
| Mean CPB time (SD) | 96.2 | 20.01 | 111.46 | 31.25 | <0.001 |
| Complications n (%) | <0.001 | ||||
| No | 88 (95.7%) | 55 (55.6%) | |||
| Yes | 4 (4.3%) | 44 (44.4%) | |||
Abbreviations: SD, Standard Deviation; n, number; CPB, Cardio-Pulmonary Bypass; ICU, Intensive Care Unit.
Table 4: Comparison between patients with long /short ICU and long/short hospital stay.
Multiple logistic regressions was used to study the association between long ICU stays and other factors. All statistically significant variables in the univariate analysis were included in the model, and the final model was reached using the backward elimination method. Inotropes (single versus multiple) and extubation time (early versus late) were excluded from the final model as they were insignificant. The first model presented in Table 5 used the total LUS score as a continuous variable and included age, Euro SCORE II, ICU lactate (12 h), CPB time, and the occurrence of complications. All those variables are associated with higher odds of having a long ICU stay with Pseudo R2 =0.60.
| Model 1 for long ICU stay | |||||
|---|---|---|---|---|---|
| Long ICU stay | Crude OR | Adjusted OR | P-value | 95% CI of OR | |
| Age | 1.12 | 1.1 | 0.003 | 1.03 | 1.17 |
| EuroSCORE II | 7.71 | 6.04 | < 0.001 | 2.3 | 15.85 |
| ICU lactate | 1.59 | 1.36 | 0.023 | 1.04 | 1.76 |
| CPB time | 1.03 | 1.03 | 0.041 | 1 | 1.05 |
| Complications (yes) | 10.88 | 13.49 | < 0.001 | 3.56 | 51.08 |
| Total LUS score | 1.65 | 1.66 | < 0.001 | 1.28 | 2.14 |
| Model 2 for long ICU stay | |||||
| Age | 1.12 | 1.11 | 0.001 | 1.04 | 1.17 |
| Euro SCORE II | 7.71 | 8.12 | <0.001 | 3.03 | 21.76 |
| ICU lactate | 1.59 | 1.43 | 0.004 | 1.12 | 1.82 |
| CPB time | 1.03 | 1.03 | 0.03 | 1 | 1.05 |
| Complications (yes) | 10.88 | 13.14 | <0.001 | 3.58 | 48.16 |
| LUS score >4 | 14.68 | 9.59 | <0.001 | 3.3 | 27.9 |
| Model 1 for the long hospital stay | |||||
| Age | 1.11 | 1.08 | 0.006 | 1.02 | 1.14 |
| Euro SCORE II | 5.29 | 3.9 | 0.001 | 1.74 | 8.72 |
| ICU lactate | 1.57 | 1.3 | 0.027 | 1.03 | 1.65 |
| Complications (yes) | 17.6 | 20.85 | <0.001 | 5.41 | 80.35 |
| Total LUS score | 1.53 | 1.45 | <0.001 | 1.19 | 1.77 |
| Model 2 for the long hospital stay | |||||
| Age | 1.11 | 1.08 | 0.004 | 1.03 | 1.14 |
| Euro SCORE II | 5.29 | 4.88 | <0.001 | 2.14 | 11.13 |
| ICU lactate | 1.57 | 1.4 | 0.003 | 1.12 | 1.74 |
| Complications (yes) | 17.6 | 20.14 | <0.001 | 5.47 | 74.12 |
| LUS score >4 | 12.19 | 6.8 | <0.001 | 2.62 | 17.62 |
Abbreviations: ICU, Intensive Care Unit; CPB, Cardio-Pulmonary Bypass LUS, Lung Ultrasound Scan; OR, Odd Ratio.
Table 5: Multiple logistic regression of the factors associated with long ICU stay and long hospital stay (Models 1 and 2).
A second model to study the association between long ICU stay and other factors was built with the same variables in the first model, except for the total LUS score, which was presented as a binary variable (LUS>4, LUS of 4 or less). All those variables are associated with higher odds of having a long ICU stay with Pseudo R2=0.58 (Table 5).
When comparing both models for long ICU stay, the area under the curve in model 1 was 0.953 (95% CI: 0.912, 0.978), while the area under the curve in model 2 was 0.949 (0.907, 0.975). There is no statistically significant difference in the performance of the two models, p-value=0.609.
For the hospital LOS, Multiple logistic regressions was used to study the association between a long hospital stay and other factors. All statistically significant variables at the univariate analysis were included in the model, and the final model was reached using the backward elimination method. CPB time, inotropes (single versus multiple), and extubation time (early versus late) were excluded from the final model as they were insignificant. The first model presented in Table 5 used the total LUS score as a continuous variable and included age, Euro SCORE II, ICU lactate (12 h), and the occurrence of complications. All those variables are associated with higher odds of having a long hospital stay. A second model was built using the total LUS score as a binary variable (LUS>4, LUS of 4 or less) and included age, Euro SCORE II, ICU lactate (12 h), and the occurrence of complications. All those variables are associated with higher odds of having a long hospital stay (Table 5).
When comparing both models for the long hospital stay, the area under the curve in model 1 was 0.932 (95% CI: 0.866, 0.963), while the area under the curve in model 2 was also 0.932 (0.866, 0.963). There is no statistically significant difference in the performance of the two models, the p-value>0.999.
In this study, we found a strong correlation between LUS total score and duration of intensive care stay. The total LUS score was also significant when implemented as a continuous variable with other predictors in the multivariate logistic regression model. Higher LUS total score was associated with prolonged intensive care stay and mortality among our patients.
While LUS examination was not studied before as a predictor for intensive care LOS after adult cardiac surgery, our findings concord with the results of Cantiontti et al., who found a predictive value of this score when added as a continuous predictor to conventional risk models in pediatric cardiac surgery. In addition, both studies found an association between LUS and extubation time [2].
In previous studies, Stein et al. and Haase-Fielitz et al. found an association between fluid overload and prolonged length of intensive care stay and increased mortality. This agrees with our results that depended on the indirect assessment of fluid overload represented by the total lung ultrasound score, which relies on lung B-lines [11,12].
Our study found a significant correlation between LUS score and prolonged critical care LOS for each quadrant independently. However Cantiontti [2] described a difference between lung quadrants, assuming that anterior lung quadrants were more significant and had a better association with outcomes. This discrepancy could be attributed to the difference in age groups and that Cantiontti performed his US examinations at different time intervals of 12, 24, and after 5 days, unlike in our study, where all investigations were after 12 h postoperatively.
Our univariate analysis shows that advanced Age, higher Euro SCORE II, elevated Intensive care serum lactate after 12 hours, prolonged Cardiopulmonary Bypass time (CPB time), multiple inotropic support, delayed extubation time, and presence of major intensive care complications were significantly associated with prolonged intensive care length of stay (more than 3 days).
In our study, high EuroSCORE II was found to be predictive of a prolonged ICU stay of more than three days. Ranjan et al. also found EuroSCORE II predictive for an intensive care stay of five days or more in patients undergoing off-pump CABG. Wang et al. and Meadows et al. found the score also correlates well with prolonged intensive care stay in cardiac surgery. Those results align with our findings despite our population undergoing valvular or CABG surgery [13-15].
Increased age of more than 75 and increased inotropic support were among the significant predictors found in the retrospective study by De cocker et al. LaFaro et al. also included advancing age and increased ionotropic support as a part of their predictive models for ICU LOS after cardiac surgery. Bhukhal et al. also reported increased poor outcomes with an increased number of inotropic supports used at the end of surgery. Our findings assured both; however, the use of multiple inotropes was significant in univariate analysis but not in the multivariate regression model; this might be attributed to the influence of other factors in the model. Advancing in age was predictive for prolonged ICU stay in our model with an adjusted odds ratio of 1.10 and a p-value of 0.003 [16-18].
In our study, we found that extubation time was correlated with critical care LOS in the univariate analysis but not in the multivariate one. This could be explained by the effect of other factors presented in the multivariate analysis. This is met by Fernandez-Zamora et al., who found an association between prolonged mechanical ventilation and poor outcomes in their multicentric study that included 3588 patients [19].
Twelve hours of lactate level was one of the positive predictors for critical care LOS among our patients; this finding is in line with Haanschoten et al. and Radovic et al. who concluded that peak arterial lactate after cardiac surgery was associated with poor outcomes, increased incidence of acute kidney injury, and mortality. They also found that persistently elevated blood lactate after 24 hours had a predictive value of 30-day mortality after mitral valve replacement surgery. On the other hand, we found no predictive significance of lactate level measured just after critical care admission; the same finding was described by Evans et al. [20-22].
One of the other predictors we found is the CPB time, as increased CPB time was associated with prolonged critical care LOS and poor outcomes; also Salis et al. and Nissinen et al. described the same [23,24].
Meadows et al. investigated Euro SCORE as a predictive tool for ICU LOS. This resulted in both old additive and logistic Euro SCORE having a reliable and accurate prediction value of 79.77% and 79.73%, respectively. Despite that, the newer Euro SCORE II was included in our model and was significant as a total score but depending only on Euro SCORE leads to neglection of all intraoperative and early postoperative variables, which have a great impact on outcomes such as bypass time, postoperative serum lactate, and major intensive care complications which all were significant in our model [15].
De Cocker et al. model included twelve independent preoperative predictors, including advanced age, female gender, dyspnea status more than New York Heart Association class II (NYHA II), unstable symptoms, extracardiac arterial disease, impaired kidney function, presence of arrhythmias, mitral insufficiency grade II, Intra-Aortic Balloon Pumping (IABP), inotropic support, aortic surgeries, and emergency procedures. This model has an excellent discriminative ability for the Prediction of intensive care stays of more than 2, 5, and 7 days [16].
Prediction of prolonged stay in intensive care after cardiac surgery was previously investigated with different models among published articles. The discrepancy between different models might be linked to various causes, including the sample size, patient selection, and the wide range of variables in cardiac patients. For example, Rotar et al. recently published a model based on the Society of Thoracic Surgeons (STS) prediction score and included 3283 patients in their study. Risk factors had severe preoperative COPD, recent pneumonia, and dialysis-dependent and preoperative patients. However, this cannot be applied to our study population as any history of a significant chest disease was an exclusion criterion, and hence our sample size was smaller (191); none of our patients was dependent on renal dialysis [25].
Limitations of the current study: limited generalizability of our results as they only included adult elective CABG and valvular surgeries, so further studies including different age groups and different types of cardiac surgery are recommended. Also, factors related to mechanical ventilation and their effect on LUS score, if possible, including; mode, PEEP, peak airway pressure, recruitment maneuvers, and FiO2, were not analyzed.
The postoperative total lung ultrasound score after cardiac surgery is helpful in the Prediction of prolonged intensive care stay and hospital stay as there is a strong correlation between both. Third, management modulation based on LUS scores was beyond the scope of our study, so further studies to assess the effect of this issue are recommended. Despite these limitations, our results emphasize the predictive value of total lung ultrasound score on intensive care length of stay and, subsequently, the patient's clinical course. Hence, modulating intensive care management after cardiac surgery based on LUS scores or targeting to avoid high scores could be helpful in improving patient outcomes.
This study is registered on ClinicalTrials.gov (NCT04499027; principal investigator: Mohamed Ahmed Hamed; date of registration: August 5, 2020).
Ethics approval
The ethical review board of Fayoum University Hospital approved the study design before the start of the study (D 230). The methods were done according to the relevant guidelines and regulations.
Consent to participate
Written informed consent was taken from all patients.
Consent for publication
Not applicable
Competing interests
The authors declare no conflicts of interest.
Author's contributions
Data collection: MAH, MHR, MLB. Data analysis: MAH, RAA, MAA, MLB. Writing: MAH, MAA, MHR, RAA. Revising: MAH, RAA, MLB, MAA, MHR. Study design: MAH, MAA, MHR, MLB. Patient recruitment: MAH.
All authors contributed equally to this work.
Corresponding author and the guarantor: MAH
Funding
The authors have no sources of funding to declare for this manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgment
Not applicable.
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
Citation: Hamed MA, Boules ML, Abdelghaffar RA, Ragab MH, Abdelhady MA (2022) Value of Lung Ultrasound in Predicting Intensive Care Unit Length of Stay after Adult Cardiac Surgery: A Prospective Observational Study. J Anesth Clin Res. 13:1095.
Received: 29-Nov-2022, Manuscript No. JACR-22-21091; Editor assigned: 01-Dec-2022, Pre QC No. JACR-22-21091 (PQ); Reviewed: 15-Dec-2022, QC No. JACR-22-21091; Revised: 22-Dec-2022, Manuscript No. JACR-22-21091 (R); Published: 29-Dec-2022 , DOI: 10.35248/2155-6148.22.13.1095
Copyright: © 2022 Hamed MA, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.