
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2023)Volume 14, Issue 4
During shoulder arthroscopy, extravasation of irrigation fluid can lead to nearby soft tissue pain. This pain is assumed to be caused by hydrostatic swelling. The diagnosis can be confirmed by looking for streaking of the muscle with ultrasound visualization. Traditionally, this discomfort has been treated with analgesics until the irrigation extravasation is reabsorbed and eliminated. This leaves the patient with the discomfort of pectoral pain. In this case, we report sonographically document of extravasation in the pectoral region, and introduce the novel technique of the ultrasound guided INTRAPEC injection as an alternative for pain control due to extravasation.
INTRAPEC; Ultrasound; Extravasation pain; Arthroscopy
Arthroscopy offers our orthopedic colleagues significant advantages in terms of reducing surgical incisional trauma and pain, while increasing visibility of relatively small structures. Often common injuries such as rotator cuff tears can be repaired without large incisions allowing for pain reduction and earlier return to function. A search of arthroscopy extravasation was conducted yielding many results. A summary of information was acquired by Memon and colleagues. In 2018 they reported the summary of literature related to shoulder arthroscopic extravasation. In their study they report that 26 studies existed including 4 case series, 20 case reports and 2 formalized studies. They report that the most common sign of shoulder arthroscopy extravasation included swelling of chest on the operative side. In 32 patients, observation alone was sufficient. Serious complications were rare, but required additional treatments like airway management, diuretics, steroids and percutaneous drainage of fluid in one case. They report that swelling and pain resolved from 2 to 48 hours, and patients were discharged 1 to 20 days postoperatively. They report that of the 205 patients that underwent shoulder arthroscopy, 85 of them had extravasation into the chest or neck, making it the number one complication in their study [1]. Vier and colleagues published a case of extravasation from shoulder arthroscopy that resulted in extensive swelling in the neck and head.
The patient required intubation for 24 hours allowing time for the extravasation to resolve. The patient experienced airway impingement evidenced by symptomology and CT [2]. Abutalib and colleagues published another case report of complications from shoulder arthroscopy involving bilateral pleural effusion and subsequent metabolic acidosis. While the complication involved conservative therapy, it illustrates the importance of awareness and assessment to extravasation associated with arthroscopy [3].
An active 42 year old male patient presented for shoulder arthroscopy to repair a torn rotator cuff. The patient had no prior surgical history, no allergies, not taking prescription medicines at home, and in free of comorbidities. No lab values were ordered or required prior to surgery. Following anesthesia screening and signed informed consent, the patient was placed on standard monitors, and received 2 mg Midazolam. The patient then received an ultrasound guided interscalene block targeting of the C-5 distribution to the brachial plexus. The infiltration consisted of 8 ml Ropivacaine 0.5%. A positive sensory and motor block was confirmed prior to arrival in the operating room by noting the patient’s inability to abduct the arm. The patient underwent induction of general anesthesia with Laryngeal Mask Airway (LMA), and arthroscopic repair of the rotator cuff was completed in the beach chair position. Following the procedure, the patient was taken to the PACU. When awake and conversant, the patient began to express increasing discomfort to the chest, on the operative side. A positive sensory and motor block was noted to the surgical site. Upon examination by both palpation and questioning, the patient was able to express discomfort to the chest and not shoulder. The operative side of the chest was cool to touch, blanched and swollen compared to the non-surgical side. A diagnosis of arthroscopic irrigation extravasation pain was considered and explained to the patient.
In a separate care following shoulder arthroscopy, fluid deposition was estimated to be between 1000 ml and 3000 ml according to Lu, reported in 2006 [4]. Ersin and colleagues provided a valuable summary regarding arthroscopy complications. They support the concept that swelling with concomitant pain to the nearby soft tissue is one of the most common complications of arthroscopy. They state that extravasation usually resolves within about 12 hours, but can be associated with significant discomfort [5]. Interestingly, there are multiple case reports of serious complications such as pulmonary or airway extravasation, but most articles fail to mention the incidence of chest swelling following shoulder arthroscopy [6-10].
Following completion of the case, the patient complained of chest discomfort on the operative side. Examination revealed a swollen and cool pectoral region on the same side of surgery. To confirm the diagnosis of extravasation, the surgical side pectoral region was scanned from superior to inferior using a linear probe. The linear probe was paired with a Terason 3300 (Terason, Burlington, MA) on a musculoskeletal setting. The linear probe is placed in transverse orientation over the prominent portion of the pectoralis major muscle. The scan revealed streaking throughout the pectorals major muscle, respecting the grain of the muscle.
The patient complained of “9 out of 10” pain on a Visual Analog Scale (VAS). An ultrasound guided INTRAPEC injection was offered as a solution to control the extravasation pain confined to the pectoralis major muscle, and patient agreed. The patient was judged to be of sound mind, had not received opiate medicine for surgery, and presented with increased heart rate and blood pressure as well as facial grimacing from the obvious discomfort. The patient was placed into a spine position with anesthesia provider at the opposite side of the bed to the surgical shoulder. For comparison, a linear probe, with probe cover was first placed over the non-operative side of the chest to illustrate the patients non manipulated pectoralis muscle architecture. This scan showed smooth muscle lines throughout the pectoralis major muscle. Figure 1 shows the normal pectoralis major presentation under ultrasound. The linear probe was then placed over the pectoralis major muscle on the operative side (Figure 1).
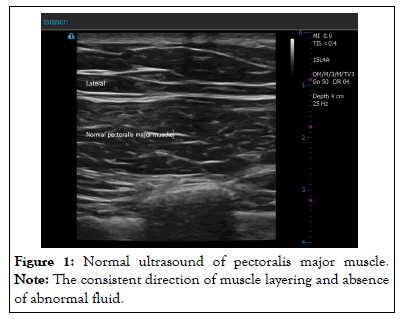
Figure 1: Normal ultrasound of pectoralis major muscle. Note: The consistent direction of muscle layering and absence of abnormal fluid.
This scan revealed multiple anechoic rivulets within the affected muscle described here as a “streaking” appearance. This indicated abnormal fluid collections within the muscle, and is illustrated in Figure 2. The skin was prepped with chlorhexidine and skin wheal rose via lidocaine 1%, 3 ml to the skin and projected needle track. A block needle (PAJUNK SonoTap, Atlanta GA) was introduced in plane, consistent with the original INTRAPEC technique described by Kline and colleagues [11]. A mixture of lidocaine 2% and Ropivacaine 0.5% was infiltrated into the muscle belly of the swollen pectoralis major muscle (Figure 2).
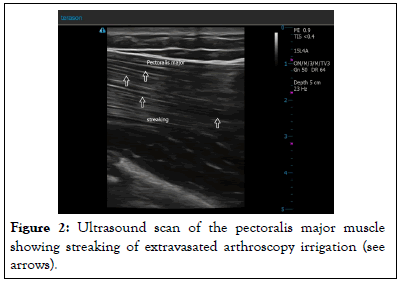
Figure 2: Ultrasound scan of the pectoralis major muscle showing streaking of extravasated arthroscopy irrigation (see arrows).
The mixture provided both fast onset and long duration of action in a dilute mixture of both solutions. Figure 3 shows the INTRAPEC technique and injection of the local anesthetic mixture providing the analgesia. Note the needle position into the bulky region of the pectoralis major muscle, and streaking of extravasated fluid. By the completion of the procedure the pain was decreased to “6 out of 10.” At the 10 minute mark the patient reported pain decrease to “3 out of 10.” The patient was subsequently discharged with a “1-2, out of 10” pain from the chest, and complete control of shoulder surgical pain from the targeted C-5 ultrasound guided injection (Figure 3).
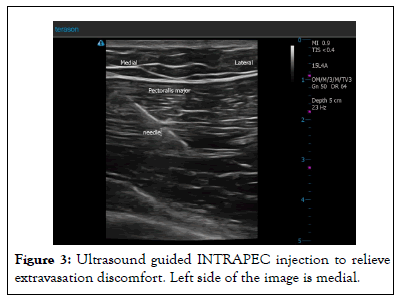
Figure 3: Ultrasound guided INTRAPEC injection to relieve extravasation discomfort. Left side of the image is medial.
Shoulder arthroscopy can sometimes lead to extravasation of irrigation fluid into nearby tissues, particularly the chest. In a study, it was found that 85 out of 205 patients experienced this complication. Swelling of the chest on the operative side was the most common sign. Serious complications were rare, but in some cases, additional treatments were required. Two case reports highlighted extensive swelling in the neck and head and bilateral pleural effusion as complications. In a presented case, ultrasound-guided INTRAPEC injection effectively relieved extravasation pain in the pectoralis major muscle. This technique shows promise as an immediate treatment option compared to conservative measures.
Arthroscopy offers our surgical colleagues distinct advantages over traditional open surgical methods, but is not without unique complications. According to Memon and colleagues, extravasation of irrigation fluid into the nearby tissues, namely the chest, is the number one complication of the procedure. This was reported to occur in about 85 of the 205 patients in their study. This means that chest and neck extravasation, following shoulder arthroscopy, has an incidence of about 40%. No evidence was located regarding an interventional, effective treatment for extravasation chest pain as an immediate modality. Currently, published articles offer time, oral or IV analgesics and potentially diuretic administration as treatment options for extravasation pain caused by shoulder arthroscopy.
Shoulder arthroscopy can be associated with extravasation of required surgical irrigation fluid. The arthroscopy irrigation can be forced into the nearby muscles, in this case the pectoralis major from the surgical region. While it is expected that the extravasation irrigation will resolve with time, the patient can be in significant discomfort. This case presentation reports the first time the INTRAPEC was used to successfully to effectively treat targeted pectoralis major pain caused by shoulder arthroscopy irrigation extravasation. The technique is simple, cost effective and seems relatively low risk. The diagnosis can be confirmed through a simple ultrasound scan including both affected and non-affected pectoralis major muscles. The appearance of streaking or anechoic rivulets through the muscle indicates abnormal fluid collections. It is assumed that these collections appearing on ultrasound examination, combined with palpation and symptoms of pain, are consistent with extravasation of arthroscopy fluid. The INTRAPEC technique may offer a more effective and immediate option for treating extravasation pain from shoulder arthroscopy extravasation pain vs. currently published, conservative measures.
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
Citation: Kline JP (2023) Ultrasound-Guided INTRAPEC Injection for Managing Chest Pain Associated with Shoulder Arthroscopy Irrigation Extravasation: A Case Report. J Anesth Clin Res. 14:1107.
Received: 10-Jul-2023, Manuscript No. JACR-23-24232; Editor assigned: 12-Jul-2023, Pre QC No. JACR-23-24232 (PQ); Reviewed: 26-Jul-2023, QC No. JACR-23-24232; Revised: 02-Aug-2023, Manuscript No. JACR-23-24232 (R); Published: 09-Aug-2023 , DOI: 10.35248/2155-6148.23.14.1107
Copyright: © 2023 Kline JP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.