Journal of Sleep Disorders & Therapy
Open Access
ISSN: 2167-0277
ISSN: 2167-0277
Research Article - (2023)Volume 12, Issue 10
Introduction: Acute Coronary Syndrome (ACS) is one of the most prevalent cardiovascular diseases in society, being characterized by myocardial ischemia or necrosis. Among the main risk factors for this pathology are sleep disorders, the most common being Obstructive Sleep Apnea (OSA), responsible for the obstruction of the airways. This blockage of respiratory flow can impair the functioning of the cardiometabolic system, leading to several cardiovascular events.
Objectives: The aim of this paper is to relate Obstructive Sleep Apnea (OSA) to Acute Coronary Syndrome (ACS).
Methodologies: Systematic and integrative review of the literature in the MEDLINE (via PubMed) and SCIELO databases, with the search strategy “Acute Coronary Syndrome (ACS) and sleep” in PubMed and sleep-disordered breathing (distúrbios respiratórios do sono) and acute coronary syndrome (síndrome coronariana aguda) in SCIELO, with the descriptors verified in Decs. Papers in all languages and papers without locality restriction were used as inclusion criteria. As exclusion criteria, papers that addressed Obstructive Sleep Apnea (OSA) as a consequence of Acute Coronary Syndrome (ACS), papers that exclusively addressed hypopnea and COVID-19, papers that related sleep-disordered breathing with pathologies not related to the cardiovascular system. The selection steps were reading titles, abstracts, and papers.
Results: A total of 157 results were found, 153 in medline (via PubMed) and 4 in SCIELO, of which 107 were eliminated by reading the titles, leaving 50. Subsequently, 34 were chosen by reading the abstracts. Then, 15 were eliminated through full reading, leaving 19 as the basis for this review.
Conclusion: There is a proven relationship between Obstructive Sleep Apnea (OSA) and a risk factor for Acute Coronary Syndrome (ACS).
Obstructive Sleep Apnea (OSA); Cardiovascular diseases; Circadian cycle, Acute Coronary Syndrome (ACS)
Acute Coronary Syndrome (ACS) is one of the main causes of death in the world, it is among the most dangerous cardiovascular diseases and is characterized by the partial or total obstruction of the coronary artery [1]. This pathology can be caused by the dissection of the coronary artery, coronary spasms, microvascular disfunction, embolism and, mainly, atherosclerotic plaque, developing then, an ischemia in the muscle tissue of the heart [2]. The ACS can be classified as an unstable angina and sudden Myocardial Infarction (MI), and can have an ample spectrum of clinical representation, exemplified by its subdivision that consists in electrocardiographic presentation through analysis of the presence or not of a sudden elevation of the ST segment [1]. The ACS manifests prodromic clinical signs like tachycardia, diaphoresis, emesis and, particularly, progressive anginal chest pain and discomfort with upper limb paresthesia [3]. Accordingly, with the intention to prevent and minimize the development of the aforementioned symptoms, it is worth noting the risk factors for this pathology, among them the Sleep-Disordered Breathing (SDB) growing gradually nowadays, besides hypertension, diabetes, obesity, sedentarism and dyslipidemias [4]. Currently, with technology development and globalization, there are drastic changes in population’s lifestyle; among them, the excessive use of electronic devices, reduction in physical activity and the rising of junk food consumption, affecting individual healthy directly. The main consequence of this change is the negative interference of SDB in the human body in a systemic way, particularly, in the cardiovascular system, resulting in high blood pressure, inflammation and insulin levels [5].
Moreover, cortisol, a hormone produced by adrenal glands and regulated by the Hypothalamus-Pituitary-Adrenal (HPA) axis, coordinates the circadian cycle which synchronizes the biological tasks with the ecosystem. This circadian rhythm contributes to a better mental and physical well-being, besides influencing many physiological functions of the human body, especially the aligning of the cardiovascular system in an impressive way [6]. The SDB, one of the main risk factors of ACS, has as its main manifestation the Obstructive Sleep Apnea (OSA), characterized by a periodic blockage of air flow by the collapsing of upper airways, resulting in ample fragmentation of sleep during the circadian cycle, an intermittent hypoxia and in variations in the intrathoracic blood pressure [7]. The OSA can be subdivided into light and moderated, affecting approximately 15% of the population, or severe, affecting around 4 to 5% of citizens [8]. The OSA is an indicator of emerging ACS risk, since OSA promotes hypoxia, oxidating stress and systemic inflammation, besides a deregulation of the sleep-wake cycle and the endogenous circadian regularity, which affects directly the cardiovascular regulation [7,9,10]. Hence, this
relationship becomes evident because the prevalence of OSA was specified in 65.7% of patients with ACS [11]. Therefore, this review has as an objective to connect Sleep-Disordered Breathing, especially, Obstructive Sleep Apnea (OSA), as one of the main risk factors of Acute Coronary Syndrome (ACS). The result of this analysis can contribute to a better prevention of the disease and help in its treatment.
Study of systematic and integrative literature review using the medline (via PubMed) and SCIELO databases. The bibliographic search took place in July 2023 and a filter of papers with at least 10 years of publication was used. As the inclusion criteria, were applied: a) papers in all languages; b) papers without locality restrictions. As the exclusion criteria, the following were used: a) papers hat addressed OSA as a consequence of ACS; b) papers that exclusively addressed hypopnea; c) papers that relate SDB with pathologies unrelated to the cardiovascular system; d) papers that associated SDB with COVID-19. On the SCIELO platform, the descriptors sleep-disordered breathing (distúrbios respiratórios do sono) and acute coronary syndrome (síndrome coronariana aguda) were applied, which were verified in the Health descriptors (DeCS) and associated with the Boolean operator “AND” to structure the strategy of the search shown in Table 1. On PubMed, the descriptors verified in DeCS, Acute Coronary Syndrome (ACS) and sleep, were used, which were linked by the Boolean operator “AND” to result in the search strategy search depicted in Table 1. After applying the eligibility criteria, there were 157 papers, from which a selection was made by reading titles, abstracts and full text, in order to analyze whether they corresponded to the proposed theme. Finally, 19 papers were selected for this review.
| Title | Authors | Year | Publication | Methodology |
|---|---|---|---|---|
| Short sleep duration, obstructive sleep apnea, shiftwork, and the risk of adverse cardiovascular events in patients after an acute coronary syndrome | Barger LK, et al. [10] |
2017 | Journal of the American Heart Association | Clinical Trial |
| The importance of apneic events in obstructive sleep apnea associated with acute coronary syndrome | Calcaianu G, et al. [19] | 2019 | Sleep Disorder Journal | Clinical Trial |
| Sleep Study-Guided Multidisciplinary Therapy (SGMT) for patients with acute coronary syndrome: Trial rationale and design. | Chua AP, et al. [7] | 2018 | Clinical Cardiology Journal | Clinical Trial |
| 1° Posicionamento Brasileiro sobre o impacto dos Distúrbios do Sono nas Doenças Cardiovasculares da Sociedade Brasileira de Cardiologia | Drager L, et al. [14] | 2018 | Arquivos Brasileiros de Cardiologia | Literature review |
| Impact of obstructive sleep apnea on platelet function profiles in patients with acute coronary syndrome taking dual antiplatelet therapy | Gong W, et al. [12] | 2018 | Journal of the American Heart Association | Cross-sectional observational study |
| Specific prodromal symptoms in patients with acute coronary syndrome. | Heidarzadeh M, et al. [3] | 2021 | The Open Nursing Journal | Observational case-control study |
| Obstructive sleep apnea and coronary artery disease: An unholy nexus or a holy alliance? | Mahajan SK, et al. [16] | 2022 | Journal of the Lung India | Observational cohort study |
| Apnea on survival after acute coronary syndrome: Insights from the ERICO registry | Maia FC, et al. [18] | 2017 | Journal of the American Heart Association | Observational cohort study |
| Circulating autoantibodies against neuroblastoma suppressor of tumorigenicity 1 (NBL1): A potential biomarker for coronary artery disease in patients with obstructive sleep apnea. | Matsumura T, et al. [17] | 2018 | Arquivos Brasileiros de Cardiologia | Cross-sectional observational study |
| Cortisol on circadian rhythm and its effect on cardiovascular system | Mohd Azmi, NA, et al. [6] | 2021 | Revista Internacional de Pesquisa Ambiental e Saúde Pública | Literature review |
| Obstructive sleep apnoea in acute coronary syndrome | Randerath W, et al. [9] | 2019 | European Respiratory Review | Observational cohort study |
| Analysis of the ischemia-modified albumin as a potential biomarker for cardiovascular damage in obstructive sleep apnea patients with acute coronary syndrome | Resano-Barrio P, et al. [15] | 2023 | Jornal Internacional de ciência molecular | Literature review |
| Short sleep duration after hospital evaluation for acute coronary syndrome is associated with increased risk of 6-month readmission | Romero EK, et al. [5] | 2020 | Psychosomatic Medicine Journal | Observational cohort study |
| Cardiac troponin values in patients with acute coronary syndrome and sleep apnea: A pilot study | Sánchez-De-Lá-Torre A, et al. [11] | 2018 | Chest Journal | Cross-sectional observational study |
| Clinical characteristics of patients with acute coronary syndrome at high clinical suspicion for obstructive sleep apnea syndrome | Szymanski, FM, et al. [4] | 2013 | Hellenic Journal of Cardiology | Cross-sectional observational study |
| Acute coronary syndrome: Unravelling the Biology to Identify New Therapies | Tucker B, et al. [2] | 2022 | Cells Journal | Literature review |
| Reducing cardiovascular risk through treatment of obstructive sleep apnea: 2 methodological approaches. | Yaggi HK, et al. [8] | 2016 | American Heart Journal | Cross-sectional observational study |
| Abnormal circadian rhythms are associated with plaque instability in acute coronary syndrome patients | Zhang ZQ, et al. [1] | 2019 | International Journal of Clinical and Experimental pathology | Observational case-control study |
| Effects of gender on the prevalence of obstructive sleep apnea in patients with coronary artery disease | Zhao LP, et al. [13] | 2014 | J Clin Sleep Med | Observational cohort study |
Table 1: 19 Selected papers
157 papers were found of which 107 were eliminated by reading the title, leaving only 50 of these 34 were chosen by reading the abstracts, that is, 15 were discarded. Then 19 were selected by reading the papers in full as represented in Figure 1.
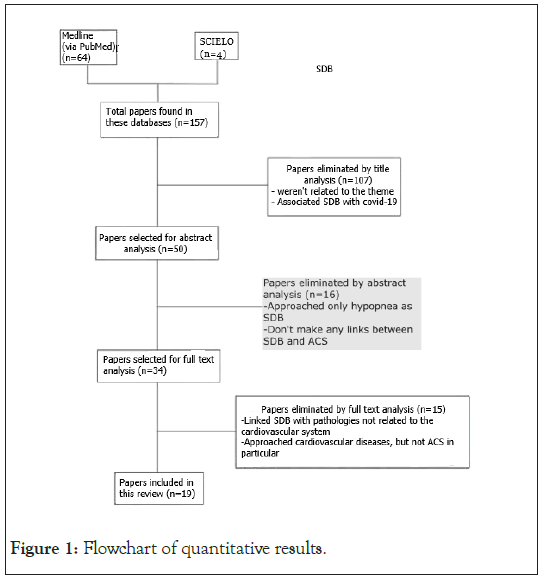
Figure 1: Flowchart of quantitative results.
From the 19 papers chosen, 1 (5.26%) was published in 2013, 1 (5.26%) in 2014, 1 (5.26%) in 2016, 2 (10.52%) in 2017, 4 (21.05%) in 2018, 4 (21.05%) in 2019, 1 (5.26%) in 2020, 2 (10.52%) in 2021, 2 (10.52%) in 2022 and 1 (5.26%) in 2023. It is clear to see that the oldest study was published in 2013, while the most recent in 2023, that is, despite being a topic covered previously, there are recent studies, which highlight its relevance and topicality in the scientific community. Regarding the language of publication, 1 (5.26%) was published in Portuguese and 18 (94.74%) were published in English.
Acute Coronary Syndrome (ACS)
Among the main cardiovascular diseases, we have ACS, a nosological entity defined by a range of ischemic expressions, caused by a partial or complete obstruction of a coronary artery, which is one of the branches of the ascending aorta artery, being responsible for the vascularization of the heart muscle, the myocardium16. Therefore, there are numerous etiologies for ACS, such as coronary artery dissection, coronary spasms, microvascular dysfunction, coronary embolism and atherosclerosis, the latter being the most prevalent in the syndrome. Furthermore, atherosclerosis itself can cause other pathologies, not exclusively in the heart, such as a cerebral ischemic stroke [2]. The pathophysiology of ACS is incidentally related to atherosclerotic plaques, which are formed by the accumulation of lipids, more specifically, Low Density Lipoproteins (LDL), in the intima layers of the arteries. The lipid cluster is capable of detaching from the arterial walls, forming a thrombus or clot, which reduces the lumen of the arterial lumen and the blood supply, causing transient ischemia and, subsequently, myocardial necrosis [2]. ACS can be classified as an Unstable Angina (UA), which consists of ischemia of the heart muscle and, thus, compromises the contractility and relaxation of the muscle pump, being considered a “pre-infarction”, due to the sudden chest discomfort felt by the patient. Furthermore, Acute Myocardial Infarction (AMI), which corresponds to a restriction of the blood supply, causing total necrosis of the heart muscle is subdivided into acute myocardial infarction with ST segment elevation (STEMI) and acute myocardial infarction without ST segment elevation (STEMI). The difference between these two types of infarctions can only be identified on the electrocardiogram, through the elevation or not in the ST segment [1].
Therefore, the identification of ACS occurs initially through prodromal signs, which appear before the pathology itself. Among them, anginal pain or discomfort radiating to the upper limbs that lasts about 10 minutes and worsens with exertion, in addition to tachycardia and diaphoresis. However, there are other, less common clinical signs that may be signs of a possible episode of ACS, such as emesis, sweating, nausea or dizziness, which despite being unusual, should not be neglected or disregarded [3]. After the appearance of the aforementioned symptoms, whether common or not, tests are carried out to ensure the clinical diagnosis is made. Among the tests, those of myocardial necrosis markers stand out, which are responsible for confirming if there was a heart attack or not, namely Troponin and CK-MB, followed by an electrocardiogram to check whether the elevation of the ST segment occurred or not [9].
The risk factors for ACS include genetic and environmental aspects, which together can be extremely dangerous for the development of this pathology. These include SDB, diabetes, obesity, hypertension, physical inactivity, smoking and a diet rich in cholesterol. Therefore, the best way to prevent and minimize the effects of this pathology is by combating these factors [4].
The circadian cycle is known as a pattern that takes approximately 24 hours, where the light-dark intervals harmonize biological functions with the environment, coordinating human physiology in such a way that the body functions as a properly harmonized clock. The suprachiasmatic nucleus of the hypothalamus functions as the “master of the clock”, as it induces sleep and anabolic and catabolic functions during the night [6]. Thus, sleep-disordered breathing corresponds to a wide range of clinical conditions, which is capable of negatively influencing the physiological functioning of the human body [12]. Possible complications in the sleep cycle, whether awake or in a drowsy state, can result in the emergence of pathologies, and consequently, reduce the individual’s quality of life, for example, the short duration of the drowsy period, described as<6-7 hours per night is a proven risk factor for incident Cardiovascular Disease (CVD) [2,5]. Among sleep-disordered breathing, there is hypopnea, which is characterized by a partial reduction in oxygen flow in tissues, and apnea, a respiratory dysfunction that highlights periods of hypoxia. Therefore, it is worth noting that apnea can be classified into several types, including Central Apnea, defined by the interruption of respiratory flow due to the absence of an inspiratory effort, being identified by Cheyne-Stokes breathing, a clinical condition defined by intermittent phases of central apneas and hypopneas. Moreover, Obstructive Apnea is defined by the interruption of respiratory flow with the presence of an inspiratory effort [5].
Furthermore, Obstructive Sleep Apnea (OSA) is classified according to the recurrence of obstructive events during the state of drowsiness, being classified as mild (5-14.9 obstructive events per hours of sleep), moderate (15-29.9 events obstructive events per hour of sleep) and severe (30 or more obstructive events per hour of sleep) [5]. Besides, there are factors that contribute to the worsening of this clinical picture, such as hypothyroidism, obesity, reduced ventilatory stimulus and, in particular, the male sex, given that OSA is 2-4 times more common in men. This prevalence occurs due to the presence of female protective hormones in relation to the accumulation of adiposity, the chemical impulse to breathe and higher levels of leptin [13]. Patients who have OSA manifest numerous clinical signs, which can be daytime or nocturnal and are presented in Table 2.
| Period of symptoms | Circumstances | Symptoms |
|---|---|---|
| Nighttime | Apneas Seen | Habitual Snoring |
| Suffocation on awakening | ||
| Gastroesophageal Reflux | ||
| Nighttime Urinary Incontinence | ||
| Night Sweating | ||
| Fractioned Sleep | ||
| Daytime | Excessive drowsiness | Transient Amnesia |
| Mood Swings | ||
| Decreased Libido | ||
| Xerostomia upon awakening | ||
| Morning Headache |
Table 2: Characteristic clinical symptoms of obstructive sleep apnea
Habitual snoring is the most common symptom in OSA; still, it is insufficient to make a diagnosis in isolation, regardless of its level of intensity. However, resuscitative snoring, which is characterized by a continuous respiratory pause with explosive snoring and nocturnal choking, can be considered a high probability of being OS [14].
The relationship between Obstructive Sleep Apnea (OSA) and Acute Coronary Syndrome (ACS)
OSA is a clinical condition that causes partial or total blockage of the upper airways during sleep. These occlusive occurrences cause a series of mechanical, hemodynamic, chemical, neuronal, and inflammatory manifestations. These physiological responses of the body result in alterations in cardiometabolic processes, including the interruption of insulin signaling, endothelial function, increased blood pressure and inflammation, because of oxidative stress [15]. That said, these changes occur due to OSA, resulting in recurrent cycles of hypoxia and restricted sleep. Intermittent hypoxia, characterized by a reduction in O2 levels, and sleep limitation promote an increase in oxidative stress, as it accentuates the formation of reactive oxygen species. Furthermore, the activation of the Sympathetic Nervous System occurs, stimulating inflammatory pathways, which drive endothelial, leukocyte and platelet cells, in order to increase the levels of inflammatory cytokines and interleukins-6 that can lead to endothelial injury and dysfunction [7,16,17]. Additionally, individuals with OSA have substantially higher levels of endothelin and lower levels of nitric oxide. Thus, these people who have elevated levels of endothelin associated with resulting arterial desaturation and hypercapnia (increased CO2 concentration), are predisposed to deregulation of systolic arterial pressure, since activation of the Sympathetic Nervous System occurs, causing the progression of BP, which may cause subsequent hypertension [16].
Moreover, activation of the Sympathetic Nervous System (SNS) promotes changes in insulin levels, an anabolic hormone, which is secreted by the beta cells of the pancreatic islets. That said, this hormone is essential for the regulation of glucose and cellular energy metabolism, acting on functions such as the synthesis of glycogen, proteins, and lipids. Therefore, unregulated insulin levels favor the exacerbated production of fatty acids and cholesterol, allowing the formation of atheroma plaques, which can mainly cause ACS13.
In addition, sleep-disordered breathing is capable of causing endocrine dysfunction, such as the relationship between cortisol production and insulin secretion. Physiologically, cortisol secretion is regulated by the Hypothalamic-Pituitary-Adrenal (HPA) axis. Thus, during the circadian cycle, cortisol levels are reduced in the initial period of sleep, and then there is an increase in the final phase of sleep. Upon awakening, there is a high level of cortisol, which controls physiological functions, such as the sleep-wake cycle, electrolyte balance, immune and neuroendocrine systems, and especially cardiovascular functions [6]. Cortisol levels in the body are regulated by the activity of the HPA axis and the enzyme 11 β-hydroxysteroid dehydrogenase (11 β-HSD 1), which performs the function of converting cortisone into active cortisol. Cortisol levels directly influence the risk of cardiovascular events, as 11 β-HSD 1 manifests itself as an extremely considerable factor in the pathogenesis of cardiovascular diseases, such as AMI and atherosclerosis. Therefore, low rates of 11B-HSD 1 generate a change in the lipid profile, modifying the hepatic metabolism of lipogenesis, which promotes a high content of peripheral adipose tissue, causing obstruction in the vessels and, consequently, ACS10. Thus, all the physiological changes mentioned above and depicted in Figure 2, are caused by OSA and are considered strong risk factors for the development and worsening of ACS, considering that OSA, in addition to being one of the main threats to cardiovascular homeostasis, it is often neglected by the population [18].
Figure 2: Flowchart demonstrating the relationship between OSA and ACS.
Treatments for Obstructive Sleep Apnea (OSA) and Acute Coronary Syndrome (ACS)
Although there are already treatments for ACS, such as the use of thrombolytics associated with angioplasty, it is worth highlighting that the most efficient therapeutic method would be to combat the pathology’s risk factors, especially OSA, as this would minimize the incidence and severity of the syndrome [8]. Thus, the main form of treatment for OSA is Continuous Positive Airway Pressure therapy (CPAP), which is defined by stimulation of hematosis, carried out by promoting a longer opening time of the pulmonary alveoli and, consequently, greater efficiency in gas exchange [8]. Therefore, this treatment can repress the effects of inflammation, blood lipid levels and blood pressure. However, despite being the most successful and most used method, acceptance of CPAP varies between 29% and 85%, a rate that is relatively low, given that adherence should be greater [17]. Due to the low adherence of individuals to CPAP, it is essential to use biomarkers, which indicate patients who require more intense therapy. Initially, this treatment was carried out based on some markers such as soluble tumor necrosis factor receptor, tumor necrosis factor beta, interleukin-6 and soluble intercellular cell adhesion molecule 1. Currently, the most modern therapy consists of using circulating antibodies as opposed to special atherosclerosis antigens as new biomarker [17].
Furthermore, reduced sleep hours pose a significant threat to cardiovascular diseases, as they reduce adherence to health habits, especially physical activities. Thus, due to the reduction in physical exercise, there is a substantial increase in sedentary lifestyle rates, leading to a biological predisposition to obesity. Therefore, this tendency to accumulate lipids can directly impact human arteries, causing dyslipidemia, which can progress to atherosclerosis and, subsequently, to ACS13. On the other hand, specific primary treatments for ACS should not be disregarded, which are based on the use of medications, mainly P2Y12 inhibitor antiplatelet drugs, such as clopidogrel and ticagrelor, and anticoagulants, which have the ability to reduce ischemic events. Furthermore, there is still the possibility of a procedure called percutaneous coronary intervention to remove the thrombus, in order to guarantee efficient reperfusion [12,13,19].
Based on the scientific papers analyzed, it is concluded that there is a considerable relationship between Obstructive Sleep Apnea (OSA) and Acute Coronary Syndrome (ACS). In addition, in order to ensure efficient reperfusion, a procedure known as percutaneous coronary intervention might be used to remove the thrombus. This association occurs due to hypoperfusion during the circadian cycle, causing several negative events that can be extremely harmful to cardiometabolic physiology. Furthermore, it is worth highlighting that the regularity of the sleep cycle is a contributing factor to homeostasis, whether physical or psychological.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Motta RFOS, Vieira LLP, Milones MESV, Nascimento ALD, Gaia BOF, Fachin LP, et al. (2023). The Relationship between Sleep-Disordered Breathing and Acute Coronary Syndrome. J Sleep Disord Ther.12:479.
Received: 17-Oct-2023, Manuscript No. JSDT-23-27614; Editor assigned: 19-Oct-2023, Pre QC No. JSDT-23-27614 (PQ); Reviewed: 02-Nov-2023, QC No. JSDT-23-27614; Revised: 09-Nov-2023, Manuscript No. JSDT-23-27614 (R); Published: 17-Nov-2023 , DOI: 10.35248/2167-0277.23.12.479
Copyright: © 2023 Motta RFOS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.