
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 5
Background and aims: Transversus Abdominis Plane (TAP) block has proven to be an effective component of multimodal analgesic regimen for a variety of abdominal procedures. Morphine has the potential to be an ideal adjuvant in TAP block. We studied the efficacy of morphine as an adjuvant to ropivacaine in TAP block in patients scheduled for abdominal surgery under General anesthesia.
Methods: Sixty patients belonging to American Society of Anesthesiologists physical status 1 or 2, aged between 18 and 58 years, scheduled for abdominal surgery under GA. Were recruited. Patients in Group A (n=30) received 20 mL 0.375% Ropivacaine whereas those in Group B (n=30) received 20 mL Normal Saline (NS) in the ultrasound (USG)-guided TAP block performed on each side after the completion of the surgery under GA. They were evaluated for pain at 0 min, 30 min, 2 hrs, 4 hrs, 6 hrs, 12 hrs and 24 hrs after the end of surgery, time to first rescue analgesic and duration of postoperative analgesia were noted.
Results: The post-operative Visual Analogue Scale (VAS) scores were lower in Group A at 4, 6 and 12 h (P<0.05). Mean duration of analgesia was significantly prolonged in Group B with lesser requirement of rescue analgesic (P<0.05) up to 12 hours.
Conclusion: Morphine (2 mg) as an adjuvant to Ropivacaine in USG-guided TAP block reduces post-operative pain scores prolongs the duration of analgesia and decreases demands for rescue analgesics.
Adjuvants; Anaesthesia; Analgésia; Ropivacaine; Pain
Any abdominal surgery such as laparoscopy, laparotomy or abdominal wall repair, are usually associated with severe postoperative pain. The conventional approach to postoperative analgesia after abdominal surgery is multimodal drug technique using Non-Steroidal Anti-Inflammatory Drugs (NSAID), opioid analgesics, and infiltration of local anesthetic at surgical site. Opioids are effective for treatment of postoperative pain, but do cause nausea, vomiting, decreased gastrointestinal motility, respiratory depression, and unwanted sedation. Local infiltration does not relieve deep muscular and visceral pain, and NSAIDs are nephrotoxic and do not provide adequate analgesia. The Transversus Abdominis Plane (TAP) block is a newly developed regional analgesic lock technique involving the nerves of the anterior abdominal wall. Blockade of these nerves accessed in the neurofascial plane between the internal oblique and the transversus abdominis muscles through a well-defined entrance at the triangle of Petit using a double pop or a loss of resistance technique, results in profound analgesia [1,2].
Landmark technique is associated with difficulties due to anatomical variation of triangle of Petit, difficulty in palpation of angle in obese patients and complications like injury to colon, liver and nerve or unpredictable spread of local anesthetic solution [2]. When compared to placebo, the ultrasound TAP block produced significantly reduced pain scores and opioid analgesic requirement in postoperative period following surgery of inguinal hernia repair, open appendicectomy, laparoscopic cholecystectomy, laparotomy, lower segmental caesarean section, hysterectomy and other laparoscopic gynaecological/surgical procedure [2]. Therefore, in this present study, we intend to evaluate the clinical efficacy of ultrasound guided Transversus Abdominis Plane (TAP) block after abdominal surgery using 0.375% ropivacaine, in terms of duration of sensory block, time to first rescue analgesic (morphine), reduction in total opioid consumption, duration of analgesia and complications.
After approval by the Institutional Ethical Committee, this prospective randomized double blind control study was carried out on 60 adult consented patients with ASA physical status I and II, aged 18-58 years, posted for elective abdominal surgeries under general anaesthesia. The exclusion criteria included patient’s refusal, patients using chronic analgesic medication, deranged bleeding profile, patients with hepatomegaly, allergy to the medicine drug, hepatic and renal insufficiency, inability to visualize the plane on ultrasound and patient’s having psychiatric disorder.
All selected patients were randomly allocated to one of the two groups of 30 patients each, using a computer generated random number assignment in sealed opaque envelops. Patients in Group A received TAP block with 20 ml of inj. Ropivacaine 0.375% under ultrasound guidance and Patients in Group B received TAP block with 20 ml of normal saline under ultrasound guidance.
During pre-anesthetic visit, the patients were explained about the aim of study, advantages and risks of procedure. They were instructed to demand analgesia as per requirement and informed written consent was obtained. Patients were also educated about the 10 cm Visual Analogue Scale (VAS) during the preoperative assessment. Study medication was prepared and labeled by an anesthesiologist with code number who was not involved in patient’s assessment. The post-operative parameters were recorded by another anesthesiologist to ensure the blindness of study.
On arrival at Operation theatre, routine monitoring of heart rate, non-invasive automated blood pressure, pulse oximetry, and Electro Cardio Gram (ECG), were started to record the base line vital parameters. An intravenous access was secured with an 18G IV cannula and infusions of lactated Ringer solution were stared in non-dominant arm. All patients were premeditated with midazolam (0.02 mg/kg), glycopyrrolate (0.005 mg/kg), fentanyl (2 μg/kg) and inj. ondansetron 0.15 mg/kg intravenously, 5 minutes prior to surgery. After preoxygenation with 100% oxygen for 3 minutes, patients were induced with propofol 2 mg/kg, followed by vecuronium bromide (0.1 mg/kg) to facilitate the direct laryngoscopy and endotracheal intubation. Anesthesia was maintained with isoflurane, nitrous oxide in oxygen (60:40). They were mechanically ventilated to maintain EtCO2 between 35-40 mm Hg.
Just before extubation, transverses abdominis plane block was given using portable ultrasound device (SonoSite M-Turbo) and a linear 6-13 MHz ultrasound transducer with 20 ml of ropivacaine 0.375% in group A and 20 ml of normal saline in group B. At the end of surgery, the residual neuromuscular block was antagonized with appropriate dose of neostigmine (0.05 mg/kg) and glycopyrrolate (0.01 mg/kg). Patients were extubated when breathing with adequate tidal volume and responded simple verbal commands. They were transferred to post anesthesia care unit for observation. Each patient was assessed by a blinded investigator in the post anesthesia care unit in respect of VAS score, time to first rescue analgesia (inj. morphine), total dose of morphine consumption (to maintain VAS score <4), hemodynamic parameters, peripheral oxygen saturation and any other complication if any, at intervals of 0 min (just after completion of surgery), 30 min, 2 hrs, 4 hrs, 6 hrs, 12 hrs and 24 hrs postoperatively.
Patients were asked to rate the average pain they experienced postoperatively on a 10 cm paper strip for VAS: No pain 0 to very severe pain 10. When the Visual Analogue Scale (VAS) score became more than 4, inj. morphine 0.03-0.15 mg/kg, intravenously was given as a rescue analgesic. The primary outcome measure in the present study was the post-operative VAS score. The secondary outcome measures included the time to first analgesic request (duration of post-operative analgesia), number of supplemental analgesic requirements and nausea/ vomiting. All the patients were monitored in the peri-operative period for hemodynamic changes and any side effects of drugs or technique related. Sample size was estimated using pain scores as the primary variable. Assuming a Standard Deviation (SD) of 10 mm, the minimum sample size needed to detect a difference of 10 mm on the VAS of 10 cm, with type I error of 0.05 and power of 80%, was 54 patients. Hence, each group required at least 27 patients. Total 60 patients were included in the present study to account for probable block failures and drop outs.
The result obtained in the study were compiled and presented in tabulated manner. Statistical analysis was done by using chi square test, one way analysis of variance (ANOVA) and post HOC analysis of one way ANOVA. P value<0.05 was considered statistically significant and P-value <0.001 was considered statistically highly significant. All these statistical analysis was done using SPSS version 16.
A total 80 patients were assessed for eligibility for the study but 10 patients were excluded from the study because of not fulfilling the inclusion criteria, 5 patients were excluded because of declining the participation in the study and 5 patients were excluded due to other reasons. After excluding these patients, the total numbers of patients in each group for the study were thirty (Figure 1).
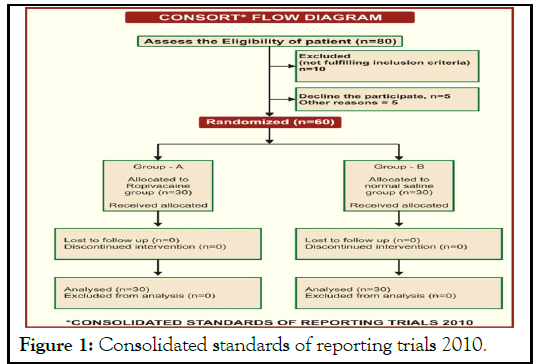
Figure 1: Consolidated standards of reporting trials 2010.
Demographic data
The demographic data of two groups were comparable in respect of age, sex distribution, BMI, and ASA physical status of the patients (Table 1).
| Demographic data | Group A | Group B | P-Value |
|---|---|---|---|
| Patients gender M/F | 13/17 | 14/16 | >0.05 |
| Mean age ± SD | 41.30 ± 10.21 | 41.00 ± 10.66 | >0.05 |
| Mean BMI ± SD | 23.56 ± 1.15 | 23.24 ± 1.49 | 0.3556 (>0.05) |
| ASA I/II | - | - | - |
Table 1: Demographic profile (Data are presented as Mean ±SD).
Postoperative VAS score
The mean baseline VAS pain score of the patients in Group A and Group B was 0.00 ± 0.00. The mean VAS pain score of the patients at 0 min, 30 min, 2 hrs, 4 hrs, 6 hrs, 12 hrs and 24 hrs post operatively in Group A were 0.30 ± 0.47, 0.40 ± 0.56, 0.40± 0.56, 0.70 ± 0.95, 1.17 ± 7.1.53, 2.07 ± 1.87 and 1.27 ± 1.62 respectively and in Group B were 3.27 ± 2.10, 5.50 ± 1.57, 4.77± 1.45, 5.37 ± 1.47, 4.77 ± 1.77, 5.00 ± 1.78 and 4.70 ± 2.20 respectively. The postoperative mean VAS pain score in patients of Group B were higher in comparison to Group A with statistically significant difference at all time intervals (p<001). Majority of patients in Group A did not suffer pain during first 24 hr postoperatively while most of the patients in Group B experienced pain during first 24 hr postoperatively (Table 2 and Figure 2)
| Time | Pain score (VAS) | P-value | |||
|---|---|---|---|---|---|
| Group A | Group B | ||||
| Mean | SD | Mean | SD | ||
| Baseline | 0 | 0 | 0 | 0 | 0 |
| 0 min | 0.3 | 0.47 | 3.27 | 2.1 | <0.001 |
| 30 min | 0.4 | 0.56 | 5.5 | 1.57 | <0.001 |
| 2 hrs | 0.4 | 0.56 | 4.77 | 1.45 | <0.001 |
| 4 hrs | 0.7 | 0.95 | 5.37 | 1.47 | <0.001 |
| 6 hrs | 1.17 | 1.53 | 4.77 | 1.77 | <0.001 |
| 12 hrs | 2.07 | 1.87 | 5 | 1.78 | <0.001 |
| 24 hrs | 1.27 | 1.62 | 4.7 | 2.2 | <0.001 |
Table 2: Postoperative pain score (VAS) of the patents.
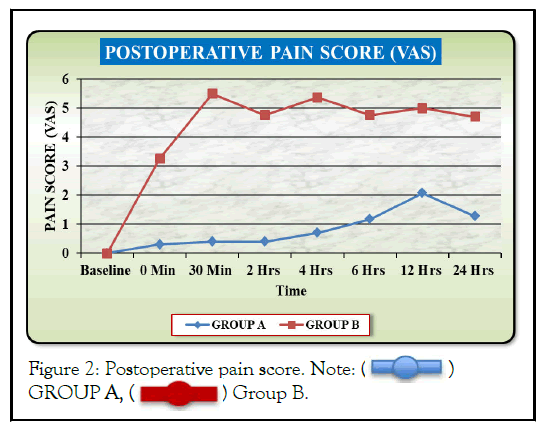
Figure 2: Postoperative pain score. Note:

Time for 1st rescue analgesia (MIN)
In the present study, the first rescue analgesia was given when the VAS score was >4. The median time for first rescue analgesia during postoperative period in patients of Group A was 720 minutes and in patients of Group B, was 30 minutes with statistically significant difference between the groups (p<0.05) (Table 3 and Figure 3).
| Groups | Group A (MIN) | Group B (MIN) | P-value |
|---|---|---|---|
| Time for first rescue analgesia (Min) | 720 | 30 | <001* |
Table 3: Postoperative time for 1st rescue analgesia.
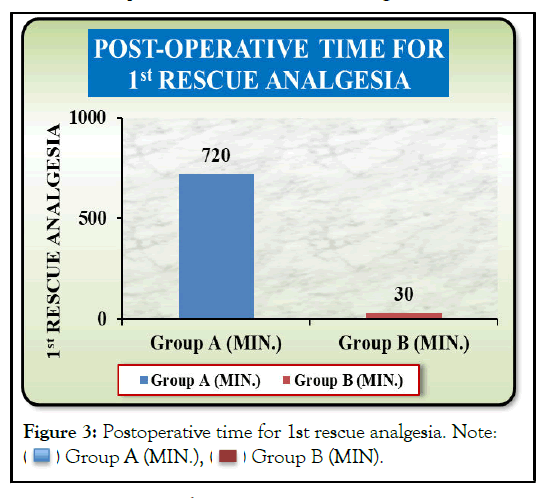
Figure 3: Postoperative time for 1st rescue analgesia. Note:
Postoperative analgesic requirement
The mean postoperative intravenous morphine requirement of the patients to maintain VAS score <4, at different time intervals was more in the patients of Group B (16.50 ± 2.70 mg) in comparison to Group A (2.70 ± 1.22 mg) with statistically highly significant difference (p<0.001) (Table 4 and Figure 4).
| Time | Morphine (mg) requirement | P-value | |||
|---|---|---|---|---|---|
| Group A | Group B | ||||
| Mean | SD | Mean | SD | ||
| Baseline | 0 | 0 | 0 | 0 | 0 |
| O min | 0 | 0 | 1.4 | 1.52 | <0.001 |
| 30 min | 0 | 0 | 2.6 | 1.04 | <0.001 |
| 2 hrs | 0 | 0 | 2.4 | 1.22 | <0.001 |
| 4 hrs | 0.2 | 0.76 | 2.8 | 0.76 | <0.001 |
| 6 hrs | 0.5 | 1.14 | 2.5 | 1.14 | <0.001 |
| 12 hrs | 0.4 | 1.52 | 2.3 | 1.29 | <0.001 |
| 24 hrs | 0.6 | 1.22 | 2.3 | 1.29 | <0.001 |
Table 4: Post-operative requirement of intravenous morphine(mg).
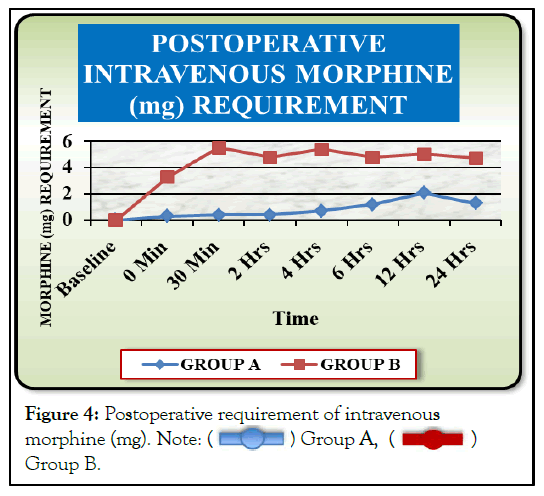
Figure 4:Postoperative requirement of intravenous morphine (mg). Note: Group B.
Group B.
Postoperative hemodynamic changes
The postoperative hemodynamic parameters were more stable in patients of Group A in comparison to Group B. The mean heart rate, mean systolic blood pressure, mean arterial pressure were significantly higher at 0 min, 30 min, 2 hrs, 4 hrs, 6 hrs, 12 hrs and 24 hrs post operatively in the patients of Group B in comparison to Group A (p<0.001). The mean diastolic blood pressure of the patients at baseline, 0 min, 30 min, 2 hrs, 4 hrs, 12 hrs and 24 hr in both the groups were comparable (p>0.05).The mean diastolic blood pressure was significantly higher at 6 hrs postoperatively in the patients of Group B in comparison to Group A (p<0.032). Only 2 patients developed vomiting but no patient developed nausea in Group A. There were 9 patients who developed nausea and 7 patients suffered from vomiting in Group B. There were no incidence of technique related complications or any other study drug related adverse effects in the both the groups.
Postoperative pain after abdominal surgery may be substantial enough to delay the early discharge of patients and ambulation. TAP block is a regional analgesic technique to provide postoperative analgesia after abdominal surgeries. The effective pain relief is achieved by blocking the nerve (T7-T12 intercostal nerves and ilio-inguinal nerve with ilio-hypogastric nerve-L1) of the abdominal wall which traverses the intervening plane between the internal oblique and transverse Abdominis muscle. The use of ultrasound has virtually surpassed the limitation of the conventional blind technique of anatomical landmark by providing direct visualization of target plane.
In our study, VAS pain score of the patients at 30 min, 2 hr, 4 hr, 6 hr, 12 hr and 24 hr post operatively in group B were statistically significantly high in comparison to group A (p=<001). Postoperatively, majority of patients in Group A did not have pain during first 24 hr while most of the patients in Group B experienced pain during first 24 hr. The postoperative hemodynamic parameters were more stable in patients of Group A in comparison to Group B. The median time for first rescue analgesia during postoperative period in patients of Group A was 720 minutes and in patients of Group B was 30 minutes. The time for first rescue analgesia was significantly delayed in the patients of Group A in comparison to Group B. (p<0.001).
The mean total dose of morphine, requiring maintaining VAS score<4 in the patients of Group A was 2.70 ± 1.22 mg as compared to 16.50 ± 2.70 mg in patients of Group B. The mean total dose of morphine requirement of the patients was statistically highly significant in the patients of Group B in comparison to Group A. (p<0.001). Only 2 patients of Group A developed vomiting while no patient developed nausea. There were 7 patients of Group B developed vomiting and 9 patients developed nausea.
When the block is performed by the land mark technique, socalled “pop” or “double pop” technique in the anatomical area of the triangle of Petit, inadvertent needle position can result in severe complications like bowel puncture, nerve injury, and puncture of the liver. Liver injury with landmark technique has been reported in a short stature woman or when liver was enlarged [3,4]. We did not observe any of these complications as we performed USG-guided TAP block, which allowed real-time visualization of needle tip and relevant anatomical structures, thus increasing the margin of safety. Rezza et al., conducted a nonrandomized comparative study to assess the efficacy of the ultrasound guided TAP block in laparoscopic colorectal resections. Their results demonstrated that preoperative TAP blocks effectively reduce the consumption of postoperative opioids when compared with the use of a PCA alone. These results coincide with our study [5]. John Carney and John G Mc Donnell demonstrated the efficacy of the TAP block with ropivacaine to provide postoperative analgesia in 50 female patients undergoing total abdominal hysterectomy under general anaesthesia via a transverse lower abdominal wall incision. Patients undergoing TAP block had reduced 48-h morphine requirements (55 ± 17 mg vs. 27 ± 20 mg, P<0.001) and a longer time to first patient controlled analgesia (PCA) morphine request compared to the placebo group. The median (interquartile range) time to first request for morphine was significantly longer in patients who received a TAP block. The TAP block with ropivacaine reduced cumulative postoperative morphine consumption compared to placebo block at all-time points [6]. These findings are consistent with the findings of present study.
When bilateral blocks are performed, the important concern is the local anesthetic toxicity, as administration of local anesthetic between fascia layers is associated with fast absorption kinetics. TAP block has been shown to cause systemic toxicity if the local anesthetic spills over into the adjacent muscles [7-16]. In the present study, we did not encounter this complication.
We concluded that ultrasound guided TAP block with 0.375% Ropivacaine is clinically highly effective and safe in providing postoperative analgesia after abdominal surgeries, if expertise for ultrasound guided TAP blocks are available. It provides better quality of analgesia of longer duration in postoperative period.
[Cross Reference] [Google Scholar] [Pubmed].
Citation: Parween J, Jain M (2022) The Efficacy of Ultrasound Guided Transversus Abdominis Plane Block for Post-Operative Analgesia after Abdominal Surgery. J Anesth Clin Res. 13:1062
Received: 03-May-2022, Manuscript No. JACR-22-17453; Editor assigned: 06-May-2022, Pre QC No. JACR-22-17453 (PQ); Reviewed: 20-May-2022, QC No. JACR-22-17453; Revised: 26-May-2022, Manuscript No. JACR-22-17453 (R); Published: 03-Jun-2022 , DOI: 10.35248/2155-6148.22.13.1062
Copyright: © 2022 Parween J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.