
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 2
Background: Strabismus correction surgery is the most common eye operation in children. The present study aims to evaluate the effects of Oro Tracheal Intubation (OTE) using a neuromuscular blocking agent (NMA) in strabismus surgery anesthesia and Laryngeal Mask Airway (LMA) application using Total Intra Venous Anesthesia (TIVA) without using NMA on the deviation angles measured following strabismus surgery.
Methods: ASA I-II group patients with concomitant horizontal strabismus, aged under 14, scheduled for strabismus surgery under general anesthesia were prospectively examined for the study. The study did not include those with restrictive type strabismus, vertical deviation, intraoperative vertical muscle group treatments, anisometropia, and corrected visual acuity less than 0.8. According to the order of arrival, either OTE was conducted with NMA, or LMA (LMA-group) was utilized without NMA for general anesthesia in patients.
Results: The study included 49 patients, divided into LMA (n=24) and OTE (n=25). The patients' mean age was 8.04 ± 3, 63 years. The distribution was similar between groups, with 63% (n=31) having esotropia and 37% (n=18) having exotropia. Angles of deviation were measured to be above 10 Δ D in 1 patient in the LMA group and two patients in the OTE group at the end of postoperative 1st month. There was no statistically significant difference between the groups regarding decreased postoperative deviation angles and preoperative-postoperative deviation angle measurements.
Conclusion: The tone changes in the eye muscles using NMA’s in strabismus surgery anesthesia caused no changes in the postoperative deviation angles or the surgical result.
Anesthesia; Ophthalmic; Surgery; Strabismus
Children with strabismus account for 3-5% of all children, with correction surgeries the most prevalent among eye operations [1]. Most pediatric ophthalmic procedures are done under general anesthesia [2]. Under general anesthesia, airway patency is maintained through endotracheal intubation or the use of a laryngeal mask airway (LMA). LMA is a more practical and less invasive procedure in the current anesthetic practices preferred over endotracheal intubation, especially in short-term surgeries and patients with difficult airways in emergencies. The LMA's design maintains epiglottis patency, allowing for easier ventilation. Air leakage is avoided using the inflatable cuff. The main benefit is that there is no requirement for muscle relaxation, and there are fewer postoperative respiratory problems than Oro Tracheal Intubation (OTE) [3,4].
In strabismus surgery, the extra ocular muscles are milli metrically shortened or lengthened to treat the impairment. Different anesthetic procedures may produce varying degrees of muscle tone loss during the application of anesthesia, resulting in inaccurate surgical correction results. The systemic effects of various anesthetic procedures in strabismus surgery have been mainly studied in patients in the literature so far [1,2,4]. However, there is limited research on the outcomes of anesthetic procedures in strabismus surgery [5,6]. The present study aims to evaluate the effects of Oro Tracheal Intubation (OTE) using a Neuro Muscular blocking Agent (NMA) in general anesthesia and LMA application using Total Intra Venous Anesthesia (TIVA) without using NMA on the deviation angles measured following strabismus surgery.
This study was designed as a single-center prospective observational study. Ethics committee approval was obtained at the Clinical Research Ethics Committee of Okmeydani Training and Research Hospital meeting, dated 07/08/2018, with the decision numbered 48670771-514.10.
The study was carried out with patients who had strabismus surgery under general anesthesia in Okmeydanı Training and Research Hospital Kasimpasa Additional Service Building between September 2018 and September 2019. ASA I-II group patients aged under 14, who were scheduled for surgery under general anesthesia and had deviation angles of 15 prism diopter (Δ D) and above due to strabismus, as well as non-paralytic horizontal strabismus, were assessed in the study. In cooperative patients, the visual acuity was assessed using the Snellen chart and form optotypes, while in non-cooperative patients, it was inferentially determined according to the fixation quality. After securing cycloplegia, a refraction examination was performed using a retinoscope and auto refractometer. Anterior and posterior segments were evaluated using slit-lamp and ophthalmoscope. The fixation and object tracking features were examined in non-cooperative cases, while the worth 4-point test was employed to identify the eye to be operated on. Globe movements were assessed in nine cardinal gaze positions, and instances were classified as esotropia or exotropia. In co-operative cases, deviation angles were evaluated using the prism cover test, while in non-cooperative cases, they were assessed using the Krinsky or Hirschberg test. Those with lens, cornea, retina, or optic nerve pathologies that may cause visual impairment, those with restrictive type strabismus, those with vertical shifts or those who had intraoperative vertical muscle interventions, those with mental retardation, those with over 2 Δ D refractive deficiency (anisometropia) between both eyes or in one eye, those with corrected visual acuity less than 0.8, those who were re-operated for strabismus and those who refuse to participate in the study were excluded.
The patient's parents were informed about the study, and their written consent was obtained. None of the patients were given pre-medication. General anesthesia was induced with intravenous propofol (2-3 mg/kg) and maintained with sevoflurane. Consecutively, either OTE (OTE-group) was applied to patients using rocuronium under maintenance anesthesia with sevoflurane (1-2 minimal alveolar concentration), and remifentanil (0.1-0.4 μg/kg/min), or LMA (LMA-group) was applied under TIVA using propofol (6-9 mg/kg/hour) and remifentanil (0.1-0.4 μg/kg/min). Horizontal (lateral and medial rectus) muscle resections with or without recession were performed in all the cases. In all cases, it is intended for post-surgery deviation angles to be ten prism diopter (ΔD) and below. All these procedures were performed by the same specialist using the same methods. Side effects were recorded, including Post-Operative Nausea and Vomiting (PONV) and Oculo Cardiac Reflex (OCR). OCR was defined as a reduction of at least 15% in baseline heart rate or dysrhythmia. Those with a heart rate of less than <65 beats/min (bradycardia) were given 0.02 mg/kg Atropine intravenously. Those experiencing complications of nausea and vomiting within the 2nd post-operative period were identified as PONV, and they were treated with intravenous 0.1 mg/kg ondansetron. Patients were routinely called for examination on the post-operative 1st day, 1st week, and the 1st month. A physician who was not involved in the study kept track of the patient’s postoperative complications and deviation angles at the end of the first month. Demographic data, anesthetic duration, complications, and preoperative deviation angles of patients in both groups were compared statistically.
Statistical analysis
Number Cruncher Statistical System (NCSS) software was used for statistical analyses. Descriptive statistical methods (mean, standard deviation, median, frequency, percentage, minimum, maximum) were used to evaluate the data. The conformity of quantitative data with the normal distribution was tested with the Kolmogorov- Smirnov and Shapiro-wilk tests and visual examinations. The student t-test was used for the binary intergroup comparisons of the quantitative data with normal distribution. In contrast, the Mann-Whitney U test was used for the binary inter-group comparisons of the quantitative data without normal distribution. The Pearson Chi-square test was used to compare the qualitative data. The Wilcoxon Signed Ranks Test was used for non-normally distributed parameters intergroup comparisons. The significance was evaluated as minimum p <0.05.
Eighty-nine pediatric patients diagnosed with strabismus were assessed during the study. Out of 36 patients who did not meet the study's criteria, 12 had anisometropia, 9 had inadequate visual acuity, 12 had vertical strabismus, and 3 had restrictive strabismus. Fifty-three patients were consecutively divided into the LMA group (n:26) or OTE (n:27). One patient in the LMA group and two patients in the OTE group were eliminated from the study because at least one of the intraoperative vertical muscle groups was intervened. One patient in the LMA group failed to show up for the postoperative follow-up. As a result, 24 patients in the LMA group and 25 patients in the OTE group had their data analyzed (Figures 1 and 2).
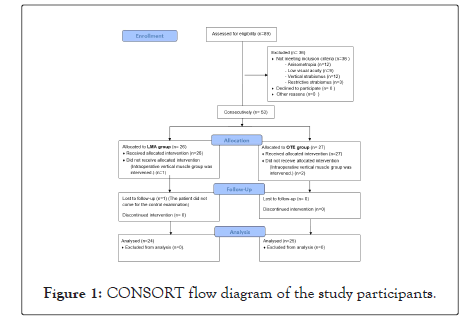
Figure 1:CONSORT flow diagram of the study participants.
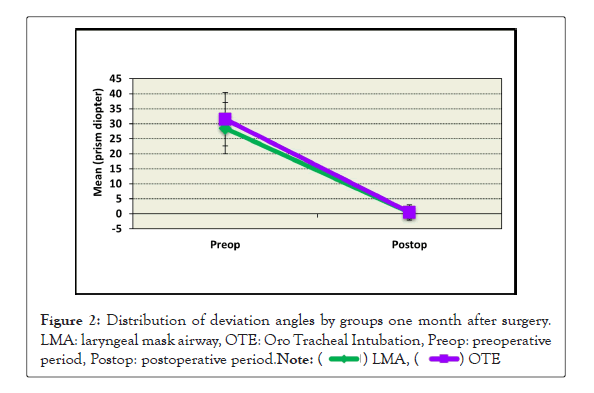
Figure 2:Distribution of deviation angles by groups one month after surgery. LMA: laryngeal mask airway, OTE: Oro Tracheal Intubation, Preop: preoperative period, Postop: postoperative period.
Of the cases included in the study, 33% (n=16) were female and 67% (n=33) were male. The participants' ages ranged from 2 to 14, with a mean of 8.04 ± 3, 63 years. Body Mass Index (BMI) measurements ranged from 20,6 to 25,8 kg/m2 with a mean value 22,20 ± 1,25 kg/m2 There was no statistical difference between the LMA and OTE groups in terms of gender (p=0.232), age (p=0.469) and BMI levels (p=0.109) (Table 1).
| Demographic and statistical data | Total (n=9) | LMA-group (n=24) | OTE-group (n=25) | p | |
|---|---|---|---|---|---|
| Age (year) | Mean ± sd | 8.04 ± 3.63 | 7.78 ± 3.74 | 8.30 ± 3.55 | 0.469 |
| Gender; n (%) | Female | 16 (33) | 10 (42) | 6 (24) | 0.232 |
| Male | 33 (67) | 14 (58) | 19 (76) | ||
| BMI (kg/m2) | Mean ± sd | 22.20 ± 1,25 | 22.00 ± 1,05 | 22.40 ± 1,40 | 0.109 |
| Anesthesia time (min) | Mean ± sd | 49.5 ± 9.9 | 47.6 ± 12.1 | 51.1 ± 8.2 | 0.456 |
| PONV (n) | 20 | 6 | 14 | 0.042* | |
| OCR (n) | 16 | 9 | 7 | 0.763 | |
| Type of strabismus; n (%) | Esotropia | 31 (63) | 16 (67) | 15 (60) | 0.769 |
| Exotropia | 18 (37) | 8 (33) | 10 (40) | ||
Note: LMA: Laryngeal Mask Airway, OTE: Oro Tracheal Intubation, BMI: Body Mass Index, PONV: Post-Operative Nausea or Vomiting, OCR: Oculo Cardiac Reflex, SD: Standard Deviation, min: minute, *p<0.05
Table 1: Demographic and preoperative clinical data of the patients.
While, esotropia was found in 63% (n=31) of the cases, exotropia was found in 37% (n=18), and there was no statistical difference in the distribution between the two groups (p=0.769). In the study, the mean duration of anesthesia was 49.5 ± 9,9 minutes, with 47.6 ± 12,1 minutes in the LMA group and 51.1 ± 8,2 minutes in the OTE group. Bradycardia OCR was noted in 16 patients throughout the intraoperative phase, and 10 cases were treated with intravenous atropine, whereas, bradycardia resolved spontaneously in 6 cases. Both groups had statistically similar distributions (p=0.763). PONV was found in 6 patients in the LMA group and 14 cases in the OTE group, and the difference was statistically significant (p=0.042).
The preoperative degrees of deviation of the cases in the LMA group ranged between 12-50 ΔD, with a mean of 28,48 Δ D. At the end of the first postoperative month, the degree of deviation ranged between 0-11 ΔD, with a mean of 1,2 Δ D. The preoperative and postoperative degrees of deviation in the LMA group were statistically different (p=0.001) (Table 2).
| Deviation angle | Statistical data | LMA-group (n=24) | OTE-group (n=25) | p |
|---|---|---|---|---|
| The deviation angle before surgery (ΔD) | Mean ± sd | 28,48 ± 8,54 | 31,50 ± 8,88 | 0.135 |
| Median (Min/ Max) | 30 (12-50) | 30 (20-55) | ||
| The deviation angle after surgery (ΔD) | Mean ± sd | 1,20 ± 1,98 | 1,50 ± 2,53 | 0.784 |
| Median (Min/Max) | 0 (0-11) | 0 (0-13) | ||
| p | 0,001** | 0,001** | ||
| The corrected deviation angle after surgery (ΔD) | Mean ± sd | -27,28 ± 7,70 | -30,00 ± 7,95 | 0.125 |
| Median (Min/Max) | -27 (-39/-12) | -30 (-42/-20) | ||
Note: LMA: Laryngeal Mask Airway, OTE: Oro Tracheal Intubation, ΔD: prism diopter, SD: Standard Deviation, min: minimum, max: maximum, **p<0,01
Table 2: Evaluation of deviation angles in the postoperative 1st month.
The preoperative degrees of deviation of the cases in the OTE group ranged between 20-55 ΔD, with a mean of 31,50 ΔD. At the end of the first postoperative month, the degree of deviation ranged between 0-13 ΔD, with a mean of 1,5 ΔD. The OTE group's preoperative and postoperative degrees of deviation were statistically different (p=0.001). One patient in the LMA group and two patients in the OTE group had a degree of deviation than 10 ΔD at the end of the postoperative first month. There was no statistically significant difference between the groups regarding preoperative and postoperative deviation angles, the decrease in postoperative deviation angle measurements (Table 2).
In ophthalmic surgeries, as in many other surgical procedures, anesthetists and surgeons use the technique and approach used to treat their patients. There is currently no consensus, particularly in strabismus surgery. Some surgeons prefer NMA to perform strabismus surgery, mainly while doing the Forced Duction Test (FDT). They are not affected by muscle tone fluctuations caused by changing the anesthetic type and depth [7]. However, some clinicians do not opt for NMA studied the effects of the inhalation agent sevoflurane and desflurane in 42 patients undergoing strabismus surgery without NMA by Migliorini, et al. [5]. They found that desflurane increased ocular deviation substantially more than sevoflurane. No study in the literature investigated the effect of employing NMA on the outcomes of strabismus surgery. According to the present study, the use of NMA’s in strabismus surgery anesthetic did not affect the operative outcome, which is the first in this area.
Strabismus surgery aims to rectify the shift in the visual axes, give single binocular vision, and achieve a fair physical appearance. Several elements influence the success of the surgery. Patients with the same degree of strabismus may respond differently to the same amount of surgical correction. This indicated that the degree of deviation or surgery amount (operated muscle) is not the sole factor affecting strabismus surgery. As a result, the inability to predict the outcome of strabismus surgeries becomes a significant issue. The globally approved scales given by the American Academy of Ophthalmology are frequently used to guide the amount of muscle intervention to be made in strabismus surgeries [8]. Because the values in the scales are often organized according to the preoperative deviation angles, full correction may not be possible after surgery. The influence of alterations in ocular muscle tone, which occurred with two distinct anesthetic types, on postoperative deviation angles was explored in this study, and no difference in postoperative deviation angle remission was found between the NMA (OTE) and the NMA-free (LMA) groups.
Many factors influence the degree of deviation in the postoperative period, including age, refractive problems, decreased visual acuity, type and duration of strabismus, preoperative deviation angles, surgeon experience, and how the suture is passed through the sclera [9-11]. Although most strabismus surgeries are operated under general anesthesia, eligible and compatible adult patients can be operated on with local or topical anesthetic [12]. Because all the patients in our study were children (aged between 2 and 14), they were all operated on under general anesthesia by the same surgeon using the same procedure. Esotropia was found in 63% of the patients, while exotropia was found in 37%, with a similar distribution between the two groups. Patients with a corrected visual acuity of greater than 0.8 were also included in the study, excluding most factors that could alter the surgical outcome. While the rates of decrease in deviation angles were similar in both groups in the postoperative 1st-month follow-up, only three (3.4%) patients had a value over the predicted (<10 ΔD) deviation angle. The three patients who did not have the expected outcome were over eight and had a preoperative deviation angle of more than 40 ΔD, Kampanartsanyakorn et al. [10,11] also presented the first surgical results of 304 patients with horizontal strabismus (61.5% esotropia, 38.5% exotropia), reporting that success rates were low in patients aged over six and in patients with preoperative deviation angles greater than 30 ΔD. As a result, we were unable to acquire the desired postoperative values in our patients with advanced age (>8 years) and sizeable preoperative deviation angles (>40 D) in our study.
LMA is regularly and safely used for pediatric anesthesia [13,14]. LMA in pediatric anesthesia was considered an alternative to tracheal intubation in the early 2000s; however, with the advent of next-generation LMAs such as I-gel and Cobra perilaryngeal airway (PLA), LMA has now become the preliminary choice in general anesthetic applications. Gulati, et al. [15] compared the use of LMA and OTE in strabismus surgery in 2004. They found that the LMA group had lower intraocular pressure increase and greater PONV due to LMA-induced gastric inflation. Nevertheless, PONV was shown to be lower in the LMA group in our study. The lack of a gastric drainage canal and inhalation medications utilized for anesthesia maintenance in first-generation classical LMAs could cause this paradox. In our study, we employed propofol (TIVA) to maintain anesthesia in the LMA group, and we used the new generation I-gel LMA with gastric drainage channel as the LMA. As a result, we observed statistically considerably less PONV than the OTE group, where anesthesia was maintained with an inhalation drug. Kranke, et al. [16] also reported that when propofol was utilized for strabismus surgery anesthesia, there was less PONV than inhalation agents.
OCR is identified with a reduction in heart rate of more than 15% or the onset of a new arrhythmia. During the traction and manipulation of the extraocular muscles in strabismus surgery, OCR can develop at rates ranging from 14 percent to 90 percent [17]. OCR was detected at a rate of 33% in our investigation, with no differences between the groups Aydın, et al. [18] presented the results of 86 patients who underwent pediatric strabismus surgery and reported that 34% of OCR developed. The same report also stated that the group utilizing NMA developed statistically more negligible OCR. In our study, the NMA group (OTE) developed quantitatively more minor OCR, although there was no statistical significance.
Study limitations: The most significant limitation of the study is the small number of cases and one-month postoperative followup. The success of strabismus surgery was also assessed in terms of anatomical success in our research. Because the patients were not followed up for an extended period, functional benefits such as binocularity and stereopsis were removed from the evaluation. Thus, randomized controlled studies with a larger sample size and more extended follow-up periods (>12 months) are required.
The study aims to evaluate the effects of Oro Tracheal Intubation (OTE) using a neuromuscular blocking agent (NMA) in strabismus surgery anesthesia and Laryngeal Mask Airway (LMA) application using Total Intra Venous Anesthesia (TIVA) without using NMA on the deviation angles measured following strabismus surgery. In conclusion, the tone changes in the eye muscles with the use of NMA’s in strabismus surgery anesthesia caused no changes in the postoperative deviation angles or the surgical result.
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
[Crossref] [Google scholar] [Pubmed].
Citation: John S, Mons P, Carl G (2022) The Effect of Different Anesthesia Techniques on Strabismus Surgery: A Prospective Observational Study (Anesthesia in Strabismus Surgery). J Anesth Clin Res. 13:1046.
Received: 20-Jan-2022, Manuscript No. JACR-22-15533; Editor assigned: 22-Jan-2022, Pre QC No. JACR-22-15533 (PQ); Reviewed: 07-Feb-2022, QC No. JACR-22-15533; Revised: 14-Feb-2022, Manuscript No. JACR-22-15533 (R); Published: 21-Feb-2022 , DOI: 10.35248/2155-6148.22.13.1046
Copyright: © 2022 John S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.