Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2020)Volume 9, Issue 6
Background: Worldwide, primiparous is the common cause of breathing difficulty of newborns which leads numerous complications of neonatal health. In Ethiopia, the association of primiparous and breathing difficulty is not well studied. Therefore, proving that primiparous is the cause of breathing difficulty and provision of great attention for first pregnancy in Ethiopia has great role to reduce neonatal mortality.
Methods: Institution based unmatched case control study was employed. All newborns delivered at the selected Gedeo Zone Public Hospitals, southern Ethiopia during the study period were included in the study. A total of 354 (119 cases and 235 controls) neonates with their index mother were included in the study. Newborns with unable to cry immediately after delivery were diagnosed as cases. Any delivery with congenital anomaly were excluded from the study and systematic random sampling method was employed. Data was analyzed using descriptive statistics and logistic regression model to identify factors associated with the outcome variable and result was presented using the AOR with the corresponding 95% CI.
Results: A total of 119 neonates who are unable to cry (cases) with their mothers/care takers and 235 newborns who cry (controls) with their index mothers were included. Primiparous (AOR=2.051, 95%CI: 1.129, 3.727) is the commonest cause for breathing difficulties of the newborn. Additional predictors for breathing difficulty during child birth were: No amniotic fluid status checkup during time of pregnancy, C/S mode of delivery, prolonged labor, prolonged rupture of membrane and meconium stained amniotic fluid (MSAF).
Conclusions and Recommendations: Breathing difficulty is a serious problem in Ethiopia which leads neonatal morbidity and mortality. Since, primiparous is the major predictor due to the fact that prim-parous individuals are often unaware of the demands of pregnancy and often lack routine antenatal care, great emphasis has to be given for women with first pregnancy during antenatal and intra natal periods. Therefore, attention should be given in the provision of antenatal risk assessment and intra-natal skillful birth attendance.
Primi-Parous, Breathing Difficulties, Case-Control, Ethiopia
AF: Amniotic Fluid; ANC: Antenatal Clinic; APH: Antepartum Hemorrhage; DURH: Dilla University Referral Hospital; EDHS: Ethiopian Demographic and Health Survey; FMOH: Federal Ministry of Health; ICD: International Classification of Disease; LBW: Low Birth Weight; MCH: Maternal and Child Health; MDG: Millennium Development Goals; MSAF: Meconium Stained Amniotic Fluid; NICU: Neonatal Intensive Care Unit; NMR: Neonatal Mortality Rate; PA: Perinatal Asphyxia; PMR: Perinatal Mortality Rate; PROM: Prolonged Rupture of Membranes; SDG: Sustainable Development Goals; SNNPRE: South Nations Nationalities Peoples of Ethiopia; UNICEF: United Nation Children’s Fund; WHO: World Health Organization
Globally, breathing difficulty is a common and serious neonatal problem and it significantly contributes to both neonatal morbidity and mortality in which above 130 million infants born every year and about four million neonatal deaths occurred each year [1-3]. A newborn with unable to cry is categorized as a newborn with breathing difficulties [4]. A baby diagnosed with breathing difficulties may have bluish or very pale skin, a low heart rate, poor muscle tone or be experiencing seizures a few hours after birth [5,6]. Primiparous is a woman who has been pregnant and given birth once which most of the time, leads to breathing difficulties of the newborn during delivery [7,8]. Breathing difficulty is defined as a failure to initiate, establish and sustain breathing at birth. It can also be defined as placental or pulmonary gas exchange impairment leading to hypoxemia and hypercarbia [9,10]. Based on WHO report, breathing difficulties (birth asphyxia) is the third leading cause of under-five child deaths which accounts 11% [2,11,12].
Different studies conducting in both developed and developing countries revealed that maternal characteristics (including parity) and obstetric histories including mother’s Age less than 20, Education (illiteracy), multiple Pregnancy, primi Parity, history of bad pregnancy outcome and gestational age were the determinant factors for the occurrence of breathing difficulties [13,14,15]. In Africa, and other developing countries, a small number of data were available on risk factors associated with birth asphyxia. Few evidences showed that both maternal and neonatal factors play an important role in the occurrence of birth asphyxia, as they do in high income and resource rich countries [13,16,17]. According to the report of breathing difficulties as the major complication in the newborns, it can lead to physical, mental and social incompatibility due to severe hypoxic ischemic organ damage in newborns [18].
Regardless of improvements in diagnosis and management of breathing difficulties through an organized and well equipped resuscitation program in recent years, breathing difficulties (birth asphyxia) become a leading cause of admission and death in neonatal units especially in developing countries [11]. Currently, the neonatal mortality rate (NMR) has revealed significant reduction from the 2011 EDHS report [19,20]. In Ethiopia, the reduction in neonatal mortality was comparatively low in which an international community was in agreement on new framework, the sustainable development goals (SDGs) to reduce neonatal mortality to at least as low as 12 deaths per 1000 live births by 2030 [21]. Neonatal deaths account for almost 40% of under-five deaths and 29/1000 neonatal death occur in Ethiopia [22,23].
There are confirmed predictors of breathing difficulties in different studies. However, there are also some factors which are not verified particularly in our setting and to prove primiparous is the cause of breathing problems of newborns [24]. Hence, to reduce the impact of breathing difficulties on neonatal morbidity and mortality, it needs further study in diverse setting. Therefore, this study is aimed prove that primiparous results breathing problem in Southern Ethiopia.
Setting and design of the study
Study setting: The study was conducted in Gedeo zone public health institutions from February 2018-July-2018. Gedeo zone is located in Southern Ethiopia 360 Km far from Addis Ababa the capital city of Ethiopia. Gedeo zone is in the Southern Nations Nationalities and Peoples’ Region (SNNPR) of Ethiopia with administrative center of Dilla town [25]. Gedeo zone is bounded by Sidama in the South, Abaya in the North, H/Mariam in the East and Kericha in the West and the total population is 1, 086,768 with 532,516(49%) male and 554, 225(51%) female with an area of 1,210.89 square kilometers and it has a total of 179,677 households. And in the zone there are 6 districts and two town cities with 164 kebeles with 31 urban kebeles and 133 rural kebele with the total of 276 health facilities from this one referral hospital, three district hospital,38 health center,146 health posts, five NGO clinics,36 private clinics and 47 drug venders [26,27].
Study design: Institution based unmatched case control study was employed in Gedeo zone public Hospitals of SNNPR, Ethiopia from January 2020-April-2020 to prove primiparous is the cause of breathing difficulties [26,27].
Characteristics of participants
Newly delivered newborns with their index mothers who diagnosed as breathing difficulties in hospitals during the study period were considered as cases and those diagnosed with no breathing difficulties in that area and period were taken as controls. The sample size was determined using a formula for two population proportions and calculate by Open Epi version 7 statistical software package by considering that the percent of controls exposed (newborns who are able to strongly cry and/or adequate breathing) among the controls is 5.05%, percent of cases with exposure is 14.2% which was estimated from another study done in Nigeria, 95% CI, 80% power of the study and control to case ratio of 2:1 with 3.11 odds ratio [14] (Figure 1).
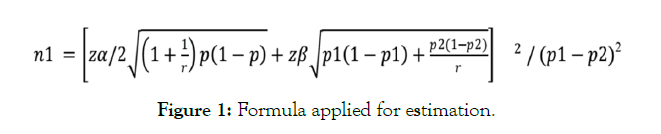
Figure 1: Formula applied for estimation.
Applying the formula, a sample of 342 newborns (114 cases and 228 controls) was needed. Adding 10% nonresponse rate, the final sample size of 377 (126 cases and 251 controls) was planned to conduct the study. Data was collected by using observational and client interview method of data collection by structured questionnaire filled by the data collectors. It was collected from the study subjects (the mother of the newborn) after all procedures had been completed immediately after delivery. Actually, a total of 119 neonates who had birth asphyxia (cases) with their index mothers and 235 newborns who had no birth asphyxia (controls) with their index mothers were included making a response rate of 93.9%.
To assure the quality of data, training was given for data collectors on how to observe deliveries, APGAR scoring, clinical sign of breathing difficulties and filling data, and on each data collection day some percent of the collected data were examined by the principal investigator, any problem forwarded had got immediate solution. Data was collected from study subjects using pre-tested (5 % of the total sample size (19 newborns with their index mothers)) structured questionnaire. The questionnaire was developed in English and translated in to Amharic and then back to English to check for its consistency. The instrument was adopted from different literatures developed for similar purpose by different authors [14-29].
Data processing and analysis
The collected data was entered to and analysed by using SPSS version-24 computer software. Frequency distribution tables and statistical graphs were used to describe variables. Cross-tabulation and logistic regressionwere done to examine association between dependent and independent variables and a significant variables were entered in to multivariable analysis and adjusted odds ratio (AOR) was seen to check confounding factors. A 95% confidence level and p-value of less than 0.05 was considered to get statistically significant.
Maternal characteristics and obstetric history
A total of 119 cases and 235 controls were included in this study. The median age of mothers included in the study was 27 years (IQR=27). More than 80% of index mothers, 86 (24.3%) of cases and 198 (55.9%) controls were in the age group ranging from 22- 34 years. Previous pregnancy status of index mothers was analyzed and the report showed that about 68 (19.2%) cases and 129 (36.4%) controls were experienced singleton pregnancy. Forty nine (13.8%) mothers who were delivered baby with breathing difficulty (cases) and seventy three (20.6%) who were delivered baby with no breathing difficulty (controls) were primi-gravida (Table 1).
| Variables | Category | Cases n=119 (%) | Controls n=235(%) | Total n=354 (%) |
|---|---|---|---|---|
| Age of index mother | ≤21 years | 17 (4.8) | 24 (6.8) | 41 (11.6) |
| 22-34 years | 86 (24.3) | 198 (55.9) | 284 (80.2) | |
| ≥35 years | 16 (4.5) | 13 (3.7) | 29 (8.2) | |
| Maternal educational status |
Unable to read and write | 53 (15.0) | 64 (18.1) | 117 (33.1) |
| Primary | 31 (8.8) | 59 (16.7) | 90 (25.4) | |
| Secondary | 12 (3.4) | 51 (14.4) | 63 (17.8) | |
| College/University | 23 (6.5) | 61 (17.2) | 84 (23.7) | |
| Pregnancy status | Singleton | 68 (19.2) | 129 (36.4) | 197 (55.6) |
| Multiple (≥2) | 51 (14.4) | 106 (29.9) | 157 (44.4) | |
| Parity | Primi | 49 (13.8) | 73 (20.6) | 122 (34.5) |
| Multi | 70 (19.8) | 162 (45.8) | 232 (65.5) | |
| Duration of current pregnancy (GA) |
≤37 weeks (pre-term) | 49 (13.8) | 76 (21.5) | 125 (35.3) |
| 38-42 weeks (Term) | 59 (16.7) | 120 (33.9) | 179 (50.6) | |
| ≥42 weeks (Post-term) | 11 (3.1) | 39 (11.0) | 50 (14.1) | |
| History of bad pregnancy outcome |
Miscarriage | 37 (10.5) | 91 (25.7) | 128 (36.2) |
| Still birth | 57 (16.1) | 82 (23.2) | 139 (39.3) | |
| Child death | 24 (6.8) | 62 (17.5) | 86 (24.3) |
Table 1: Maternal characteristics and Obstetric History of mothers of newborns Delivered at Gedeo Zone Public Health Institutions, SNNPR, Ethiopia 2018/19 [n=354].
Factors which has contribution during pregnancy
Among mothers with their newborns participated in the study, 25 (7.1%) cases and 39 (11.0%) controls were encountered any illness during current pregnancy. At the time of pregnancy, more than half index mothers were checked their amniotic fluid status. On the other hand, 68 (19.2%) cases and 80 (22.6%) controls didn’t have any checkup of their amniotic fluid status during their current pregnancy. Among mothers included in the study, Ninety two (26.0%) cases and two hundred three (57.3%) controls have ANC visit during their current pregnancy (Table 2).
| Variables | Category | Cases n=119 (%) | Controls n=235(%) | Total n=354(%) |
|---|---|---|---|---|
| Is there any Illnesses during pregnancy? |
Yes | 25 (7.1) | 39 (11.0) | 64 (18.1) |
| No | 94 (26.6) | 196 (55.4) | 290 (81.9) | |
| Illnesses during pregnancy | Hypertension | 10 (15.4) | 20 (30.8) | 30 (46.2) |
| Anemia | 7 (10.8) | 15 (23.1) | 22 (33.8) | |
| Others* | 8 (12.3) | 5 (7.7) | 13 (20.0) | |
| ANC visit during current pregnancy | Yes | 92 (26.0) | 203 (57.3) | 295 (83.3) |
| No | 27 (7.6) | 32 (9.0) | 59 (16.7) | |
| Ultrasound check up during time of pregnancy? |
Yes | 59 (16.7) | 156 (44.1) | 215 (60.7) |
| No | 60 (16.9) | 79 (22.3) | 139 (39.3) | |
| Amniotic fluid status checkup during time of pregnancy? |
Yes | 51 (14.4) | 155 (43.8) | 206 (58.2) |
| No | 68 (19.2) | 80 (22.6) | 148 (41.8) | |
| Status of your amniotic fluid | Normal | 46 (22.3) | 126 (61.2) | 172 (83.5) |
| Abnormal | 5 (2.4) | 29 (14.1) | 34 (16.5) |
*: Chronic illnesses, bleeding during pregnancy
Table 2: Antepartum characteristics of breathing difficulties among newborn who were Born at Gedeo Zone Public Health Institutions, SNNPR, Ethiopia, 2018/19 [n=354].
Intra-partum factors
Presentation of the fetus was observed that one hundred two neonates (28.8%) cases and two hundred twenty nine neonates (64.7%) controls were delivered with cephalic presentation. About 75 (21.2%) and 44 (12.4%) cases were delivered vaginally and cesarean section respectively. As described in the table below (Table 3), thirty seven (58.7%) cases and 17 (27.0%) Controls were delivered by emergency cesarean section.
| Variables | Category | Cases n=119 (%) | Controls n=235(%) | Total n=354 (%) |
|---|---|---|---|---|
| Presentation of the fetus | Cephalic | 102 (28.8%) | 229 (64.7%) | 331 (93.5) |
| None-cephalic | 17 (4.8) | 6 (1.7) | 23 (6.5) | |
| Mode of delivery | Vaginal | 75 (21.2) | 216 (61.0) | 291 (82.2) |
| C/S | 44 (12.4) | 19 (5.4) | 63 (17.8) | |
| Vaginal Mode of delivery | Spontaneous | 53 (18.2) | 200 (68.7) | 253 (86.9) |
| Assisted (forceps/vacuum) | 22 (7.6) | 16 (5.5) | 38 (13.1) | |
| C/S Mode of delivery | Emergency | 37 (58.7) | 17 (27.0) | 54 (85.7) |
| Elective | 7 (11.1) | 2 (3.2) | 9 (14.3) | |
| Duration of labor | > 12 hours | 64 (18.1) | 51 (14.4) | 115 (32.5) |
| < 12 hours | 55 (15.5) | 184 (52.0) | 239 (67.5) | |
| Duration of rupture of membrane | > 12 hours | 47 (13.3) | 32 (9.0) | 79 (22.3) |
| < 12 hours | 72 (20.3) | 203 (57.3) | 275 (77.7) | |
| Complication during intra-partum period | Yes | 47 (13.3) | 35 (9.9) | 82 (23.2) |
| No | 72 (20.3) | 200 (56.5) | 272 (76.8) | |
| Convulsion | 13 (15.9) | 9 (11.0) | 22 (26.8) | |
| Types of complications faced | Fever | 13 (15.9) | 15 (18.3) | 28 (34.1) |
| Excessive Bleeding | 13 (15.9) | 6 (7.3) | 19 (23.2) | |
| Others* | 8 (9.8) | 5 (6.1) | 13 (15.9) | |
| Status of amniotic fluid | Clear | 45 (12.7) | 201 (56.8) | 246 (69.5) |
| Meconium stained | 64 (18.1) | 22 (6.2) | 86 (24.3) | |
| Bloody stained | 10 (2.8) | 12 (3.4) | 22 (6.2) |
*: Breech presentation, Cord abnormality, NRFHRP.
Table 3: Intra-partum factors of breathing difficulties among newborn who were Born at Gedeo Zone Public Health Institutions, SNNPR, Ethiopia, 2018/19 [n=354].
Nutrition related factors
Nutritional status of index mothers were assessed at the time of actual data collection period and the report shown in the table below (Table 4),114 (32.2%) cases and 229 (64.7%) controls have had their meal ≥3 times per day.
| Variables | Category | Cases n=119 (%) | Controls n=235(%) | Total; n=354 (%) |
|---|---|---|---|---|
| Frequency of meal per day | <3 times per day | 5 (1.4) | 6 (1.7) | 11 (3.1) |
| ≥3 times per day | 114 (32.2) | 229 (64.7) | 343 (96.9) | |
| The commonest food every day | Meat and meat products | 42 (11.9) | 47 (13.3) | 89 (25.1) |
| Vegetables | 36 (10.2) | 91 (25.7) | 127 (35.9) | |
| Shiro and Misr | 38 (10.7) | 95 (26.8) | 133 (37.6) | |
| Other* | 3 (0.8) | 2 (0.6) | 5 (1.4) | |
| Do you know a balanced diet? | Yes | 40 (11.3) | 111 (31.4) | 151 (42.7) |
| No | 79 (22.3) | 124 (35.0) | 203 (57.3) | |
| What is your favorite food? | Meat and meat products | 71 (20.1) | 122 (34.5) | 193 (54.5) |
| Vegetables | 35 (9.9) | 72 (20.3) | 107 (30.2) | |
| “Shiro and Misr” | 13 (3.7) | 41 (11.6) | 54 (15.3) | |
| Do you think that some foods are recommended during pregnancy? |
Yes | 41 (11.6) | 121 (34.2) | 162 (45.8) |
| No | 78 (22.0) | 114 (32.2) | 192 (54.2) | |
| Do you think that some foods are NOT recommended during pregnancy? |
Yes | 37 (10.5) | 43 (12.1) | 80 (22.6) |
| No | 82 (23.2) | 192 (54.2) | 274 (77.4) |
*: Any food
Table 4: Nutritional factors of breathing difficulties among newborn who were Born at Gedeo Zone Public Health Institutions, SNNPR, Ethiopia, 2018/19 [n=354].
Factors associated with breathing difficulties
Variables with p-value of <0.2 (ten of the total variables) in binary logistic regression were candidate to multivariable analysis to control confounding factors. This variables were: parity, age of the index mother, educational status of the index mother, ANC visit status, ultrasound check up status, Amniotic fluid status checkup during time of pregnancy, mode of delivery, duration of laborand color of amniotic fluid.
Among variables listed above, some variables were statistically significant in multivariable logistic regressions analysis model. These are; parity, Amniotic fluid status checkup during time of pregnancy, mode of delivery, duration of labor and color of amniotic fluid. Neonates delivered from primiparous were 2 times more likely to develop breathing difficulties than those who were from multiparous, (AOR=2.051, 95%CI: 1.129, 3.727). Mothers who have a history of amniotic fluid status checkup during their time of pregnancy were 3.5 times more likely to deliver neonates with breathing difficulties than mothers who have no amniotic fluid status checkup, (AOR=3.583, 95%CI: 1.048,12.250).
Neonates delivered with C/S mode of delivery were 4 times more likely to be asphyxiated compared to those with vaginal, (AOR=4.706, 95%CI: 2.132, 10.386). Neonates delivered from mothers with the occurrence of prolonged labor (labor>12 hours duration) were 2 times more likely develop breathing difficulties than those delivered from mothers with normal duration of labor (labor<12 hours duration), (AOR=2.224, 95%CI: 1.117, 4.430). Neonates who were delivered with no clear amniotic fluid were 5 times more likely to have breathing difficulties when compared to those neonates delivered with clear amniotic fluid, (AOR=4.991, 95%CI: 2.609,9.547) (Table 5).
| Variables | Category | Cases n=119 (%) |
Controls n=235(%) |
COR (95%CI) | AOR (95% CI) |
|---|---|---|---|---|---|
| Age of index mother | ≤21 years | 17 (4.8) | 24 (6.8) | 1.124 (0.330,3.824) | 0.599 (0.130, 2.759) |
| ≥35 years | 16 (4.5) | 13 (3.7) | 2.747 (1.407,5.363) | 0.963 (0.382,2.429) | |
| 22-34 years | 86 (24.3) | 198 (55.9) | 1 | 1 | |
| Maternal educational status | Literate | 66 (18.6) | 171 (48.3) | 1 | 1 |
| Illiterate | 53 (15.0) | 64 (18.1) | 2.146 (1.352, 3.405) | 1.420 (0.755,2.669) | |
| Parity | Primi | 49 (13.8) | 73 (20.6) | 1.553 (0.983,2.455) | 2.051 (1.129,3.727) |
| Multi | 70 (19.8) | 162 (45.8) | 1 | 1 | |
| ANC visit during current pregnancy | Yes | 92 (26.0) | 203 (57.3) | 1 | |
| No | 27 (7.6) | 32 (9.0) | 1.862 (1.055,3.287) | 0.767 (.343,1.713) | |
| Ultrasound check up during time of pregnancy? |
Yes | 59 (16.7) | 156 (44.1) | 1 | 1 |
| No | 60 (16.9) | 79 (22.3) | 2.008 (1.281,3.149) | 0.489 (0.140,1.705) | |
| Amniotic fluid status checkup during time of pregnancy? |
Yes | 51 (14.4) | 155 (43.8) | 1 | 1 |
| No | 68 (19.2) | 80 (22.6) | 2.583 (1.643,4.061) | 3.583 (1.048,12.250) | |
| Mode of delivery | Vaginal | 75 (21.2) | 216 (61.0) | 1 | 1 |
| C/S | 44 (12.4) | 19 (5.4) | 6.669 (3.665,12.137) | 4.706 (2.132,10.386) | |
| Duration of labor | > 12 hours | 64 (18.1) | 51 (14.4) | 4.198 (2.610,6.754) | 2.224 (1.117,4.430) |
| < 12 hours | 55 (15.5) | 184 (52.0) | 1 | 1 | |
| Complication during intra-partum period |
Yes | 47 (13.3) | 35 (9.9) | 3.730 (2.231,6.236) | .803 (0.374,1.724) |
| No | 72 (20.3) | 200 (56.5) | 1 | 1 | |
| Color of amniotic fluid | Clear | 45 (12.7) | 201 (56.8) | 1 | 1 |
| Not Clear | 74 (20.9) | 34 (9.6) | 9.722 (5.785,16.336) | 4.991 (2.609,9.547) |
Note: The symbol (*) indicated that these factors had statistically significant association with breathing difficulties
Table 5: Bivariate and Multi variable logistic regression among factors of cases and controls attending at Gedeo Zone Public Health Institutions, SNNPR, Ethiopia, 2018/19 [n=354].
This study was aimed to assess predictors of breathing difficulties and to prove primiparous as a predictor. It has tried to identify the predictors of breathing difficulties by incorporating as many predisposing factors as possible in addition to parity. Unable to cry was the pertinent indicator to diagnose breathing difficulties of the newborn during delivery in this study [5]. In general, maternal characteristics & obstetric history, antenatal factors, intra-partum factors and nutrition related factors associated with breathing problems were entertained in this study.
This study showed that parity was highly significant with birth asphyxia. Neonates delivered from primi-gravida mothers were 2 times higher to be suffered by breathing difficulties than those who were from multi-gravida mothers. This study is consistent with a study conducted in Central Zone of Tigray region in Ethiopia and Bangladesh [30,31]. This may be due to the fact that primiparous are usually do not have care their pregnancy or have less interest the demand to have pregnancy and often neglect antenatal booking.
On the other hand, there are variables significantly associated with breathing difficulties in which most of them are due to being primiparous. These are: Amniotic fluid checkup at antenatal period, mode of delivery, Duration of labor, meconium stained amniotic fluid.
Amniotic fluid checkup at antenatal period have also a significant association with birth asphyxia. Mothers who have a history of amniotic fluid status checkup during their time of pregnancy were 3.5 times more likely to deliver neonates with breathing difficulties than mothers who have no checkup. This may have a direct relation with an antenatal booking and follow-up which minimizes the risk of fetal distress associated with meconium stained amniotic fluid.
This is in lined with a study conducted in India, Cameron and Brazil and this could be because of the reason that, amniotic fluid check-up helps to diagnose abnormalities of AF. One of the most common problems of amniotic fluid is being meconium stained which is a response of acute hypoxic event resulting leakage of plasma protein in to the airways from areas of epithelial disruption. This study is consistent with previous studies conducted in a tertiary care center, India, antenatal and intra-partum risk factors for perinatal asphyxia in India and a finding from a low-resource setting in Cameron [15,18].
Regarding intra-partum related problems, mode of delivery was highly significant with birth asphyxia. This study showed that neonates delivered by cesarean section mode of delivery was 4 times higher to be asphyxiated than those with vaginal mode of delivery. This is inconsistent with a study conducted in Dilchora Referral Hospital, in Dire Dawa, Eastern Ethiopia and India [30-33]. This could be due to the fact that the study conducted in India was focused on neonates admitted in pediatrics ward and they were considered home vaginal mode of delivery. But, in our context, we were considered neonates delivered in health institutions.
On the other hand, in our study, delivery was mostly by emergency caesarean section, similar to what was reported in Nigeria [19]. This could be explained by the fact that indications for the caesarean sections were mostly due to prolonged obstructed labor or eclampsia.
Duration of labor was statistically significant in our study. Neonates delivered from mothers with the occurrence of prolonged labor (labor>12 hours duration) were 2 times higher to develop breathing difficulties than those delivered from mothers with normal duration of labor (labor<12 hours duration). This is consistent with several studies conducted in Ethiopia [34-36]. The may be explained by prolonged labor implies maternal fatigue and oxygen deprivation leads to inadequate breathing of both the mother and neonate.
On the other way, this study was conducted at referral and district hospitals where laboring mother might arrive after a long journey in which clients spent much time to reach there. Therefore, this may lead to breathing difficulties while birth.
In our study, amniotic fluid status was found to be a significant factor for birth asphyxia. Neonates who were delivered with no clear amniotic fluid (like MSAF or BSAF) were 5 times higher to have breathing difficulties when compared to those neonates delivered with clear amniotic fluid. This study is similar with several previous studies conducted in both developed and developing countries [20- 39]. In healthy, well oxygenated fetuses, this diluted meconium is readily cleared from the lungs by normal physiological mechanism, however in few cases meconium aspiration syndrome occurs.
This could be also explained by the fact that color of amniotic fluid may be meconium or bloody stained due to prolonged labor and/ or prolonged rupture of membrane which leads fetal distress.
The major predictor of breathing difficulties of the newborn in southern Ethiopia is primiparous. Breathing difficulty is one of the worldwide problem of neonatal mortality and morbidity. It arises several complications of health, if the cases left untreated and leads to death. Since, the case is highly preventable, attention should be given in the provision of antenatal risk assessment and intra-natal skillful birth attendance.
The authors designed, performed analysis, interpretation of data, and wrote manuscript and prepared the manuscript. Both authors were read and approved the final manuscript.
I am grateful to Gedeo zone health office for their cooperation to provide the necessary data about the study area. My appreciation also goes to the data collectors who showed the utmost effort in acquiring the appropriate data.
Citation: Melaku G, Mergia G (2020) The Association of Primiparous and Breathing Difficulties of the New Born in Southern Ethiopia: A Case Control Study. J Women's Health Care 9:508. doi:10.35248/2167-0420.20.9.508.
Received: 21-Sep-2020 Accepted: 13-Nov-2020 Published: 20-Nov-2020 , DOI: 10.35248/2167-0420.20.9.508
Copyright: © 2020 Melaku G, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.