Journal of Thyroid Disorders & Therapy
Open Access
ISSN: 2167-7948
ISSN: 2167-7948
Case Report - (2025)Volume 14, Issue 1
Background/Objective: This case report aims to discuss the treatment journey of a patient with increasing thyroid eye disease-related proptosis, who has responded teprotumumab after failre with other available treatment modalities.
Case presentation: The patient was initially seen and diagnosed elsewhere with IGG4-related orbital inflammation and treated with systemic steroids. Later, he became hyperthyroid and his orbital inflammation worsened. Systemic steroids helped the inflammation slightly, but as his condition worsened, he received a cycle of 4 doses of tocilizumab, followed by another cycle of 4 doses of tocilizumab. After a prolonged period of stability, he underwent bilateral rehabilitative lateral orbital wall decompression. Unfortunately, the patient's condition relapsed again. The patient commenced an eight-dose course of teprotumumab, with each dose administered at three-week intervals. Remarkably, with each successive dose of teprotumumab, the patient demonstrated a consistent improvement in proptosis and remained free from relapse.
Discussion: Treatment with teprotumumab has resulted in favourable clinical outcomes for recurrent and severe thyroid eye disease.
Conclusions and importance: Teprotumumab played a crucial role to reverse and stabilize the condition that relapsed after systemic corticosteroid treatment, two cycles of tocilizumab and bilateral lateral orbital decompression surgery.
Thyroid eye disease; Proptosis; Orbital decompression surgery; Relapse; Teprotumumab
Thyroid Eye Disease (TED), also known as graves ophthalmopathy or graves' orbitopathy, is an autoimmune condition affecting orbital tissues. Ocular inflammation (during active disease), subsequent tissue remodelling and fibrosis (during inactive disease) are hallmarks of Thyroid Eye Disease (TED). Although patients may sometimes experience hypothyroidism or have normal thyroid function, TED is more commonly associated with graves' hyperthyroidism. Endocrine symptoms may manifest prior to, at the same time or later in the course of thyroid eye disease.
The prevalence of thyroid eye disease is estimated to be around 2.9 per 100,000 males and 16 per 100,000 females within the population. The important risk factors include smoking, age, Radioactive Iodine Therapy (RAI) and female gender.
Symptoms of TED are variable and can be mild, moderate or severe. Thyroid eye disease can result in varying degrees of facial disfigurement and decreased quality of life. In approximately 5% of the cases, the condition can lead to loss of vision due to optic nerve compression, corneal ulcer and elevated intraocular pressure [1].
Treatment of thyroid eye disease has evolved over the past decade. In the past, systemic corticosteroids have been the mainstay of active TED. Systemic steroids have been combined with other immunosuppressant agents, surgery and radiotherapy. Recently biologics, including teprotumumab and tocilizumab, have been introduced to treat different stages of TED. In this report, we will discuss a case of an unusual TED whose condition relapsed following maximal treatment with systemic steroids and two cycles (8 doses) of tocilizumab followed by rehabilitative orbital wall decompression. He responded well to teprotumumab treatment.
A 38-year-old male patient was referred to Sheikh Shakhbout Medical City in February 2018 with 3 weeks’ history of left-sided proptosis and a presumptive diagnosis of orbital myositis. On presentation, he was already on oral steroid treatment. Initial eye examination revealed a visual acuity of 6/6 in both eyes and diplopia in the up and left gaze. Extraocular movements examination showed limitation in bilateral lateral and up gaze. Hertel exophthalmometry showed 22 mm in the right eye and 26 mm in the left eye. Posterior segment examination was normal [2].
Laboratory findings revealed elevated C-Reactive Protein (CRP) and Immunoglobulin G4 (IgG4) levels, while the thyroid panel was within normal limits. Computed Tomography (CT) showed bilateral enlargement of the extraocular muscles, primarily involving the medial rectus muscle insertion site. The patient refused to undergo a muscle biopsy [3].
The patient was advised to taper the oral steroid and he was referred to the rheumatology team for further investigation.
Approximately ten months after the initial diagnosis, the patient presented with symptoms of foreign body sensation, eyelid swelling and redness, worsening diplopia and headache. Exophthalmometry was stable at 24 mm OD and 27 mm OS. Laboratory investigations confirmed a hyperthyroid status. He had low Thyroid-Stimulating Hormone (TSH) and higher thyrotropin receptor antibody (TSI). CT scan was repeated for the patient which showed further enlargement of most of the recti muscles and hazy intraconal orbital fat consistent with TED. He was referred to the endocrinology team, who started the patient on antithyroid medication. Despite the normalization of his thyroid status, the patient experienced a gradual worsening of his eye disease between March and May 2019. His clinical activity score was 7, with visual acuity of 6/6 in both eyes, with normal colour vision, but his exophthalmometry was progressively increasing (28 mm in the right eye and 30 mm in the left eye). A decision was made to initiate tocilizumab therapy for the patient. He received 4 doses of 8 mg/kg of tocilizumab monthly between May 2019 and September 2019. He responded well to the first 4 doses of 8 mg/kg tocilizumab in terms of proptosis reduction and improvement in CAS. His condition remained stable for nearly 9 months. His exophthalmometry reading was 28 at the end of the treatment in both eyes with minimal CAS. Starting in March 2021, he had a second relapse of disease activity (Figure 1). His thyroid function tests were unstable and he underwent a total thyroidectomy (May 2021). At this point, his exophthalmometry values were 32 mm in both eyes and his clinical activity score was 7 [4].
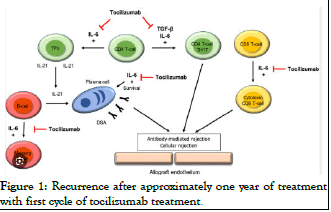
Figure 1: Recurrence after approximately one year of treatment with first cycle of tocilizumab treatment.
The patient received a second cycle of 4 doses of tocilizumab 8 mg/kg between August 2021 and January 2022. After the second cycle, the final exophthalmometry value was 31 mm in both eyes.
From January to December 2022, his CAS was stable. He was scheduled for orbital decompression and underwent right and left deep lateral orbital decompression combined with fat decompression in December 2022 and January 2023. The preoperative exophthalmometry values were 31 mm, decreasing to 24 mm postoperatively in both eyes [5].
In May 2023, there was a recurrence of his condition characterized by a deterioration in proptosis, worsening of clinical activity score and experiencing pain behind the eyes. His hertel exophthalmometry measurements revealed values of 27 mm in the right eye and 26 mm in the left eye.
Subsequently, the patient was initiated on teprotumumab. The first dose was administered on the 10th of May 2023. He had a total of 8 doses. By the end of the 8th dose, the patient's CAS improved to minimal with exophthalmometry values of 24 mm in both eyes (Figure 2). The patient has been stable since his last visit. Besides temporary muscle fatigue, he did not develop any other side effects from the medication [6].
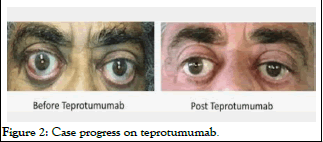
Figure 2: Case progress on teprotumumab.
Treatment of thyroid eye disease has evolved over the recent years. Depending on the stage of the disease, treatment may include observation only, supplements, systemic steroids, immunosuppression and biologics. Recurrence of the disease is a very well-known entity, occurring in 15-22% of all cases. There is no benchmark for the treatment of recurrences in TED and the treatment options may include any of the aforementioned modalities.
Recent advancements have shed light on the pathophysiological mechanisms underlying thyroid eye disease. The evolving treatment strategy for TED is also placing increased emphasis on biological drugs. Precise immune regulation makes biologics safer and more effective than traditional methods. It has been shown in multiple studies that there are increased levels of insulin-like Growth Factor-1 Receptor (IGF-1R) and Thyrotropin Receptor (TSHR) in the affected tissues of patients suffering from TED [7].
Though both TSHR and IGF-1R are two independent receptors, there is physical and functional interconnection between the two receptors, the nature of which is being under intense investigation [8].
Teprotumumab is a monoclonal antibody designed to target and inhibit the Insulin-like Growth Factor 1 Receptor (IGF-1R). This mechanism of action is crucial as IGF-1R plays a significant role in the inflammation, adipogenesis and fibrosis observed in thyroid eye disease. By blocking IGF-1R, teprotumumab aims to mitigate these pathological processes, ultimately alleviating symptoms and potentially halting disease progression in TED. Teprotumumab has been granted approval by the United States Food and Drug Administration (FDA) for the management of TED. It has been shown to lower proinflammatory cytokines, hyaluronan secretion and orbital fibroblast activation in TED patients by blocking the IGF-1R/TSHR signalling pathway. Treatment with teprotumumab has resulted in favourable clinical outcomes for different stages of TED [9].
Our case is interesting in the way that the patient initially responded partially to systemic steroids. Later, his condition stabilized with the two cycles of (8 infusions in total) tocilizumab. After a relatively long period of stability (approximately 1 year), he underwent rehabilitative bilateral lateral orbital wall decompression with good results. However, his CAS started to increase again after the surgeries. Recurrence after systemic steroids, other immunosuppressants, tocilizumab and orbital decompression surgery is very well documented in the literature. He responded favourably to 8 doses of teprotumumab infusions. Our reported findings are in keeping with the positive reported outcomes of teprotumumab in cases of moderate-to-severe TED highlighting teprotumumab’s potential in treating complex and recurrent cases of active thyroid eye diseases. Though there are documented cases of successful treatment of recurrent TED with teprotumumab, but to our best knowledge there has not been any report of successful use of teprotumumab following the use of tocilizumab, systemic steroid and surgery for recurrent TED [10].
This report represents a unique documented case of successfully treating recurrent TED with teprotumumab after exhausting other treatment modalities, including systemic steroids, tocilizumab and surgery. After conducting a comprehensive literature review on May 24, 2024, utilizing PubMed and Google Scholar with the keywords "tocilizumab," "teprotumumab," "active thyroid eye disease," "orbital wall decompression," "thyroid eye disease treatment failure," and "therapeutic advances," no prior reports were found in this regard. Further research is warranted to compare the efficacy of different modalities in the treatment of thyroid eye disease.
The IRB approval was not needed for this case.
A written informed consent was obtained from the patient himself.
The authors would like to thank RAY-CRO for their editorial support in developing this manuscript.
The authors state that they have no known competing financial interests or personal relationships that could have influenced the work presented in this article.
No funds, grants or other support was received.
The data that support the findings of this study are available on request from the corresponding author.
All authors attest that they meet the current ICMJE criteria for authorship.
The authors state that they have no known competing financial interests or personal relationships that could have influenced the work presented in this article.
No funds, grants, or other support was received.
A written informed consent was obtained from the patient himself.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Eatamadi H, Almazrouie O, AlQattan N (2025) Teprotumumab's Efficacy for Recurrent Severe Thyroid Eye Disease Post-Tocilizumab and Steroid Therapy. Thyroid Disorders Ther. 14:339.
Received: 26-Aug-2024, Manuscript No. jtdt-24-33649; Editor assigned: 29-Aug-2024, Pre QC No. jtdt-24-33649 (PQ); Reviewed: 12-Aug-2024, QC No. jtdt-24-33649; Revised: 11-Jan-2025, Manuscript No. jtdt-24-33649 (R); Published: 18-Jan-2025 , DOI: 10.35841/2167-7948.25.14.36
Copyright: © 2025 Eatamadi H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.