Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2022)Volume 13, Issue 2
Introduction: Teledermatology (TD) allows the delivery of timely and quality care.
Although the implementation of local systems has shown to provide good levels of resolvability, the implementation of a single system at the national level allows reaching all geographical areas in a uniform and timely manner.
Objective: To describe the results of the implementation of a unified national TD system in Chile.
Methods: Observational-retrospective study of electronic interconsultations (EIs) resolved by TD specialty in national teledermatology system from December 1st, 2018, to December 31st, 2020.
Results: A total of 49,211 electronic interconsultations from all geographic areas of Chile. From these, 57.55% received a diagnosis and treatment that could be delivered in a Primary Health Care (PHC), thus, preventing the inadequate referral of 28,321 patients to the secondary level. The most frequent specific diagnoses were: melanocytic nevus 8.86% (n:4364), Non-melanoma skin cancer 8.73% (n:4294) and irritant contact dermatitis 8.2%(n:4037). From the sample, female sex accounted for 29,942(60.8%) of the consultations. Age and latency in the resolution of median EI/interquartile range were 43/24 years and 3.5/6.4 days respectively. Finally, the diagnostic agreement between the TD specialist and the PHC physician was 71.03%.
Conclusion: The implementation of a single national TD system, which incorporates a high volume of IE and all the geographical areas of Chile, has shown to have high levels of resolvability, low waiting times, and a high level of resolution canters of origin. This could be an alternative to optimize healthcare attention in the public system of low to middle-income countries.
Teleinterconsultation; Telemedicine; Teledermatology
Teledermatology (TD) is a branch of telemedicine that, from its beginnings in the 1990s to the present, has been consolidating as a valuable tool in specialized medical practice [1]. Several studies suggest that TD is a cost-effective tool that allows decreasing waiting times, making efficient use of specialized resources, optimizing the relevance of referrals to face-to-face consultation, and improving access to the population living in rural or hard-to-reach areas [2-6]. Chile has unique geographical and demographic distribution, being one of the longest countries in the world with 4,329 km in length, poor land connectivity among cities, 15% of its territory being islands, and a rurality index of 12.2%, with high variations in population density in its different regions [7,8]. Furthermore, most of the specialized resources are densely concentrated in the central regions, with little to no access to specialized healthcare in the far regions of the north and south respectively. All of the above make Chile an ideal candidate for the implementation of a TD program at the national level.
As mentioned before, one of the difficulties derived from the geographic extension of the national territory is the gap of specialists and the distributive inequity of them. In the public health system, there are 2907 hours per week destined for dermatology, with a total of 142 professionals that work in the public health care network on a national level [9]. This translates into long waiting lists and long waiting times to access specialty care [10]. In addition, the demand for dermatological care varies between 4.8% and 19% in primary health care [11- 14]. Thus, it is necessary to increase the resolvability of Primary Care by bringing the specialist's opinion closer to the patient, without necessarily transferring care to the specialist; which can be achieved through the use of information and communication technologies [15].
In Chile, until 2017, more than 80,000 ITs were performed [3]. However, this early implementation depended on each Health Service and its respective care centres and referrers [16], which generated significant differences between different regions of Chile. Nevertheless, in December 2018, the Digital Hospital Project (DHP) was implemented, which integrated all regions into a single TD platform, available for all professionals of the public system, including all the Primary Health Care Centres (PHC centres) of the country [17]. The aim of this study is to characterize the early implementation of this platform on a nationwide level from 2018 to 2020.
Observational-retrospective study of 49,211 Electronic Interconsultations (EIs) from all geographic areas of Chile resolved by TD specialty in the national teledermatology system from December 1st of 2018, to December 31st of 2020.
Type of study
Cross-sectional study conducted from anonymized data obtained from IT generated through asynchronous telemedicine using the unified digital platform for the specialty of Dermatology during December 2018 through December 2020. The requirements of this study were reviewed according to the latest recommendation for effectiveness in reporting telemedicine systems [18]. Referral and counter-referral flow using the digital platform: The referral starts with the general practitioner at a PHC or low complexity hospital, prior consent of the patient, logs in to the digital platform and records the patient's socio-demographic data, images, medical history, previous treatments, and diagnostic hypothesis. Once the electronic consultation has been entered, it arrives in the inbox of a teledermatology specialist, who makes a diagnostic hypothesis, assigns priority (low, medium, or high, depending on the clinical and diagnostic suspicion), and determines the place of resolution (PHC or referral to a specialty center), treatment and follow-up. Finally, the patient is notified at the center of origin, the action agreed by the specialist and the PHC physician, and the TD process is considered completed.
Software used
The software utilized corresponds to the hospital digital online platform (available at: www.hospitaldigital.cl) and the consultation has no cost for the patient. The digital platforms comply with cyber security requirements according to national regulations. The information from the IT records is stored in the Ministry of Health (MoH) (Minsal) servers and the database is managed by the Data Analytics team, who anonymize and process the information then be displayed, which allows access to online information with an hourly update process.
Database
Anonymized database with the consultations recorded in the referral and counter-referral process carried out through the aforementioned telemedicine digital platform from December 1st, 2018 to December 31st, 2020.
For each electronic consultation resolved, the following was recorded: Geographic region of origin, age, sex, time to resolution, the priority assigned by the teledermatology professional, diagnosis recorded by the interconsultant and PHC physician, the diagnostic agreement between the two, and suggestions in management. These suggestions included: Need for referral for face-to-face evaluation, resolution in the centre of origin (PHC), or other, including referral to another specialty or non-relevant consultations. On the other hand, patients with incomplete data or unresolved interconsultations were excluded.
Statistical analysis
Descriptive analysis of demographic variables and by region was performed. Analysis of pathologies detected using Stata statistical software (Stata/SE 16.0 for Windows, Copyright 1985-2019 StataCorp) is included.
49,218 TIs were analysed from December 1st, 2018 to December 31st, 2020. Of these, 7 unanswered or incomplete data interconsultations were excluded, resulting in a total of 49,211 interconsultations resolved by teledermatology professionals.
Descriptive analysis of the teleconsultations
Teleconsultations by sex and age range: Of the total of 49,211 TI answered, 60.8% (n= 29,942) corresponded to female patients, while 39.2% (n= 19,269) corresponded to male patients, being female consultations higher in all group ages (Figure 1). Concerning age, median age and Interquartile Range (IQR) was 43 years, IQR: 46.
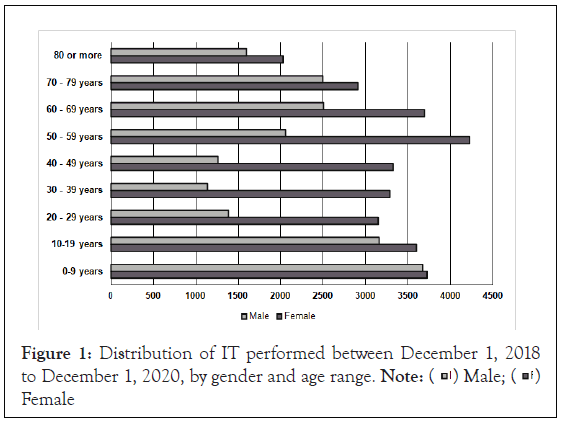
Figure 1: Distribution of IT performed between December 1, 2018
to December 1, 2020, by gender and age range.  Female
Female
TI and geographic location: The greatest number of TI received were in the Metropolitan Region (MR) (n=10,259; 20.85%). The regions with the lowest number of consultations were the Aysén Region (n= 392; 0.8%) in the south of the country; Coquimbo (n=826; 1.68%) located in the north and Arica and Parinacota (n= 839; 1.7%) located in the extreme north of the territory (Figure 2a). However, as shown in Figure 2b, when contrasting the number of consultations according to the population of each respective region, it can be observed that the regions with the highest number of consultations per 1,000 inhabitants are the Atacama, Libertador Bernardo O'Higgins, and Los Lagos Regions, with 7.33, 6.7 and 6.6 TI per 1,000 inhabitants respectively. On the other hand, the regions with the lowest TI are the Araucanía, Coquimbo, and Metropolitan Region, with 0.8, 1.09, and 1.44 TI per 1,000 inhabitants respectively.
Figure 2: Geographical distribution of IT by region in Chile (a) total IT per region. (b) IT per 1000 inhabitants of the region. Note: + Arica y Parinacota Region, Atacama Region , □ Coquimbo Region, Metropolitan Region, ● Libertador Bernardo O’Higgins Region, ▲ Bío-Bío Region, Araucanía Region, ○Aysén Region, Los Lagos Region
Platform use over time: Regarding the evolution over time, a significant increase is shown in the first months of implementation, up to a peak in July 2019 reaching 3,751 consultations. During 2020, there was a significant drop in April 2020 (n=312), with a subsequent progressive increase, which was then maintained in the last months of 2020 (Figure 3a).
Figure 3a: Temporal progression of the number of IT from the implementation of the Hospital Digital (marked with arrow) until December 2020.
IT response times
At the beginning of the implementation, there were long response times, with an average response time of 8.79 days (210.9 hours) during 2019; however, a decrease was noted during 2020, with an average response time of 3.28 days (79.66 hours). The median (IQR) response rate for the entire period was 3.5 (6.4) days (Figure 3b).
Figure 3b: Average response time in days per month since the implementation of Digital Hospital.
Diagnostic agreement
The overall diagnostic agreement between the PHC physician and the teledermatology specialist t was 71.03%. This agreement varied considerably according to the diagnostic group of the pathology involved (Table 1).
| Diagnostic group | Frequency | % of the total | Agreement | Treatment in PHC | Face to face referral |
|---|---|---|---|---|---|
| Infectious diseases | 6456 | 13.12% | 74.09% | 60.55% | 39.45% |
| Viral | 3158 | 6.42% | 82.68% | 37.68% | 62.32% |
| Mycotic | 2119 | 4.31% | 68.52% | 86.55% | 13.45% |
| Bacterial | 494 | 1.00% | 60.53% | 67.81% | 32.19% |
| Prurigo, insect stings or bites | 384 | 0.78% | 56.25% | 77.60% | 22.40% |
| Parasitic | 301 | 0.61% | 68.11% | 83.72% | 16.28% |
| Acne, rosacea, folliculitis and disorders of eccrine and apocrine sweat glands. | 5355 | 10.88% | 86.22% | 78.06% | 21.94% |
| Malignant tumors | 4985 | 10.13% | 80.18% | 7.18% | 92.82% |
| Psoriasis and other erythematous desquamative disorders | 3991 | 8.11% | 74.49% | 70.01% | 29.99% |
| Other unclassified diagnoses | 1744 | 3.54% | 54.64% | 58.72% | 41.28% |
| Hair and nail disorders | 1582 | 3.21% | 78.82% | 60.56% | 39.44% |
| Hypochromias and vitiligo | 1568 | 3.19% | 81.25% | 67.54% | 32.46% |
| Tumors, malformations and other vascular disorders | 1531 | 3.11% | 68.58% | 40.69% | 59.31% |
| Non-dermatological diagnoses | 1329 | 2.70% | 40.33% | 53.42% | 46.58% |
| Autoimmune, blistering, deposit and granulomatous diseases | 1152 | 2.34% | 57.03% | 32.12% | 67.88% |
| Hyperchromias | 755 | 1.53% | 68.21% | 68.48% | 31.52% |
| Hypertrophic and atrophic diseases | 748 | 1.52% | 76.20% | 37.83% | 62.17% |
| Trauma, wounds and radiation-induced injuries | 288 | 0.59% | 64.58% | 49.65% | 50.35% |
| Total | 49211 | 100% | 71.03% | 57.55% | 42.45% |
Table 1: Frequency, diagnostic agreement, and therapeutic suggestions by diagnostic group.
Diagnostic groups and specific diagnosis according to frequency
The most frequent diagnostic groups were: dermatitis and urticaria, and others with 18.4% (n: 9054), benign tumors and cysts 17.62% (n: 8673), and infectious diseases 13.12% (n: 6463). Nevertheless, suspected malignant tumor pathology stands out at 10.13% (n: 4985). From a total of more than 200 different diagnoses, the 10 most frequent were selected and are summarized in Table 2. The first 3 were: Melanocytic nevus accounting for 8.86% (n:4362); Non-melanoma skin cancer with 8.73% (n:4294) and Irritant contact dermatitis with 8.20% (n:4037).
| Speciific diagnosis | Frequency | % of the total | Agreement | Treatment in PHC | Face to face referral |
|---|---|---|---|---|---|
| Melanocytic nevus | 4362 | 8.86% | 66.48% | 47.02% | 52.98% |
| Non-melanoma skin cancer | 4294 | 8.73% | 90.10% | 7.24% | 92.76% |
| Irritant contact dermatitis | 4037 | 8.20% | 80.88% | 79.74% | 20.26% |
| Psoriasis | 2617 | 5.32% | 94.38% | 69.58% | 30.42% |
| Seborrheic keratosis | 2305 | 4.68% | 78.22% | 59.24% | 40.76% |
| Warts | 2296 | 4.67% | 92.64% | 36.89% | 63.11% |
| Acne | 2256 | 4.58% | 95.57% | 80.23% | 19.77% |
| Atopic dermatitis | 2170 | 4.41% | 86.59% | 83.96% | 16.04% |
| Rosacea | 1852 | 3.76% | 95.30% | 90.33% | 9.67% |
| Vitíligo | 980 | 1.99% | 95.61% | 63.57% | 36.43% |
Table 2: Frequency, diagnostic agreement, and therapeutic suggestions by most common specific diagnosis.
Treatment and follow up
In most TIs, treatment was indicated at the same center from where the interconsultation was made (n: 28,321; 57.55%), the remaining consultations (n: 20,890; 42.45%) were destined for face-to-face evaluation at nearby referral center or other destination such as referral to another specialty or labeled as non-relevant, as can be seen in Tables 1 and 2.
A successful single national teledermatology system has been established in the Chilean Public Healthcare system. From its implementation in 2018 to 2020, it has made it possible to integrate and classify the high volumes of referrals, deliver a rapid response to PHC physicians and adjust the number of patients for care in specialized centers. In total 49,211 electronic consultations were resolved, excluding 7 with missing information, embracing a system where the loss of information is minimal. To date, this is the study with the largest number of patients published in Chile [3,7,10,16,19-21] and globally [22]. The mean age of the population was 41.63 ± 26.53, with a predominance of 60.8% female sex, similar to other studies reported in Chile both in TD [3,7,10] and face-to-face dermatologic consultation [23,24]. There is a greater gender gap in the middle ages (20-69 years), with a smaller gap in the ages of 0-19 years and 70 years and over. This difference could be due to an occupational factor, greater interest for dermatological attention, increased awareness, or a greater prevalence of dermatologic pathology in the female sex in comparison to the male counterpart; however, these factors could be analysed in-depth in later studies. In absolute terms, most of the TIs performed were in the Metropolitan Region (Figure 2a). This is to be expected since this region concentrates 42% of the total population of the country (8). However, when analyzing the consultations regarding the population, it is possible to observe that the distribution of IT per 1000 inhabitants increases in the North and South of the country. This phenomenon could be explained due to the known gap between the demand for attention and the limited supply of dermatologist specialists in the most extreme areas of the country [3]. In addition to this, it is worth mentioning that the north and south of Chile have limitations regarding land connectivity; mostly due to the geographical distribution of its territory. These are the Atacama desert in the North part of Chile, the driest desert in the world [25], and the archipielago in the South, both of which greatly impact connectivity and access to more complex healthcare centers [26], making teledermatology a remarkable tool to bring specialized healthcare to these isolated communities.
Regarding the number of IT, in the first months of the implementation, a marked increase in the number of consultations can be observed. This can be explained since the early implementation of the Hospital Digital project only included a few centers of the health care network and as the project progressed the rest of the centers were integrated, nowadays including the entire health care network, with more than 700 associated centers. There is a decrease in April 2020 (Figure 3a), which coincides with the beginning of the Quarantine in Chile, after the first case of coronavirus 19 (COVID-19) reported in Chile, in March 2020 [27], a pandemic that worldwide has reduced outpatient care [28]. Despite this, it is expected that reactively, the number of IT will increase exponentially during 2021 since, in the same way, the pandemic has implied notable limitations of face-to-face dermatological care, and it is in this context the TD plays a key role in supplying the population's demand remotely [29]. Concerning the average response times, these show an increase during 2019 (Figure 3b), with an acme in October 2019, with a subsequent decrease during 2020. The longer waiting times in 2019 were possibly due to the recruitment of more centers to the implemented in the network, with the subsequent decrease due to the incorporation of more professionals in TD. The median Institute of Clinical Research (ICR) response time for the whole period was 3.5 (6.4) days, lower than other published experiences which range from 4.6 hours to even 50 days [6, 30-32]. In all the above cases and given the Chilean healthcare context, having a range of 3 to 7 days of waiting response time is an excellent standard of opportunity in teledermatology care as compared to the waiting times for face-to-face attention.
Regarding diagnostic agreement between the PHC physician and the dermatologist via teledermatology, the overall agreement for this study is 71.03%. This is similar to other reports in Chile, with agreements that range from 63% (3) to 65.3% (16).For the diagnoses made, the type of pathology involved with greater frequency will vary in the literature according to the diagnostic classification used, however, most of the experiences place with greater frequency the inflammatory pathology, followed by the benign or infectious tumor pathology and the malignant tumor pathology accounting for a 5.6 to 11% [16,33,34] of the diagnoses. Furthermore, in the diagnostic agreement by pathology, the results from this study are similar to other studies published in Chile [11], especially in pathologies such as acne, rosacea, infections, psoriasis, alopecia, and dermatitis. However, as to malignant tumor pathology, previous Chilean studies show a diagnostic agreement lower than the global average, being this 65.8% specifically for epidermal malignant tumours [16]. Despite the above, this study shows a concordance of 80.18% for malignant tumor pathology, showing an even higher agreement than the global concordance. This difference could be due to a greater experience in the use of teledermatology in both PHC professionals and dermatologists and the optimization of photographic resources, which allows for a more accurate diagnosis.
The most frequent specific diagnoses were non-melanoma skin cancer, irritant contact dermatitis, and melanocytic nevus. Nevertheless, non-melanoma skin cancer and melanocytic nevus are relevant and require a high degree of face-to-face evaluation, as shown in Table 2. On the other hand, Tele-dermoscopy can probably increase diagnostic agreement, allow patients in this subgroup to be prioritized, and optimize referral in patients with the differential diagnosis of melanocytic nevus [35,36]. Note that a high concordance is shown for acne, psoriasis, and warts. It is important to highlight this since training and education programs for general medicine should probably be oriented to these pathologies in order to increase their resolution and optimize its treatment in PHC. As mentioned before, 57.55% (n:28,321) of the consultations continued treatment in the centre of origin, while 42.31% were referred for face-to-face referral of 42.31%; similar to what is observed in other studies published in Chile with a resolution of 64% of the pathologies in the PHC and a face-to-face referral in 30.1% of the cases [10]. However, the slight differences could be due, to the greater amount of malignant tumor pathology found in this study, therefore, a greater need for a referral to face-to-face attention, among other factors. Given this context, it is key to break down the causes of why an electronic interconsultation should go to the secondary level. For the cases of both malignant and benignant tumor pathology, these cannot be solved in PHC, together with the diagnostic confirmation and management of severe dermatological pathologies. This will be evidenced in further research since these factors are now being acknowledged and registered in the referral process in the new platform. In contrast, the experience published in Spain [33] showed a resolution by teleconsultation of 50.82% and a faceto- face referral of 49.01%. These differences could be in the context that, unlike Spain, the supply of specialists in Chile is smaller; therefore, in general, the criterion per dermatologist is to reduce the need for referral, which is an important bias when determining the real need for face-to-face care. Finally, the advantages of this study include the high number of patients seen in a short period. A database that allows a minimum loss of information, good internal validity, with results similar to previous experiences in the country. This is endorsed by the fact that the TD project in Chilean Public Health Institute (ISP) has been in place for more than 10 years, with professionals already experienced, both referrers and specialists, and that more than 80,000 previous TD interconsultations had already been performed in 8 years (2010 to 2018). Concerning the limitations of this study, it is important to note that perception of quality of care by the users, the PHC physician, and the teledermatology professional were not evaluated and could be a niche for further research on the subject.
TD has shown an important leap in dermatologic care in the last decade. In the Chilean context, TD is still an incipient program, however, in a short time, with a unified platform, more than 50,000 interconsultations have been solved, covering the entire health network in all the geographical areas of the country, with low response times, high resolution in centers of origin and high degrees of diagnostic agreement between professionals.
The most-reported pathology was inflammatory pathology, followed by benign and infectious tumor pathology. Note that the use of this tool allowed for malignant tumor pathology to be diagnosed in a short period of time standing out at 10.13%. There is a high rate of cancer referrals, with non-melanoma skin cancer being a frequent diagnosis, which highlights the importance of implementing teledermatology in the resolution of tumor pathology, in order to generate diagnostic algorithms and prioritized referral in the hospital digital care network, when needed. Finally, about 28,321 patients avoided going to the secondary level and were able to follow their treatment in PHC, which highlights the role of teledermatology as a public health tool that has a great impact on the resolution of low complexity pathology, thus optimizing the face-to-face resource, avoiding unnecessary traveling, work permits, and resources and hours spent by the patients, destined to receive specialized attention when it was not necessary. This experience could serve as a pioneer project for low to middle-income countries, showing that the implementation of a unique system, as part of the public health system, is a viable and effective strategy to improve accessibility, providing timely and quality care to their users.
This study was approved by the Ethics Committee of the Servicio de Salud de Antofagasta, Antofagasta, Chile, ID: CECSSA0014.
[Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [ Google scholar]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [ Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
Citation: Luis GMJ, Ignacio GIA, María L, Vezna S Rodrigo L, Hector F, et al. (2022) Teledermatology in Chile: Implementation of a Single National System. J Clin Exp Dermatol Res. 13:605.
Received: 28-Mar-2022, Manuscript No. JCEDR-22-16379; Editor assigned: 31-Mar-2022, Pre QC No. JCEDR-22-16423; Reviewed: 14-Apr-2022, QC No. JCEDR-22-16423; Revised: 21-Apr-2022, Manuscript No. JCEDR-22-16423; Published: 28-Apr-2022 , DOI: 10.35248/2155- 9554.22.13.605
Copyright: © 2022 Luis GMJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.