Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2024)Volume 15, Issue 1
Objective: To systematically evaluate the safety and efficacy of traditional Chinese medicine in the treatment of psoriasis using the theory of blood syndrome.
Methods: Cochrane Library, Embase, PubMed, Chinese Science and Technology Journal Full Text Database (VIP), Wanfang Database and China Journal Full Text Database (CNKI) were searched by computer from establishment to January 2022. Randomized controlled trials of psoriasis treated by traditional Chinese medicine under "blood syndrome theory" were included for systematic review based on inclusion and exclusion criteria; the literature quality of the included literatures was evaluated according to the Cochrane Reviewer's Handbook 5.1.0 evaluation criteria and tools. The Cochrane Collaboration provided RevMan5.1 software, which was used as to perform meta-analysis is on all of the selected data.
Results: The "blood based treatment" of psoriasis offers certain advantages in terms of improving clinical efficacy, reducing adverse reactions, and reducing recurrence rate. However, due to methodological problems of included studies and possible publication bias, these limitations should be considered before drawing conclusions.
Blood syndrome theory; Traditional Chinese medicine; Systematic review; Meta-analysis
Evidence-based medicine research is frequently utilized to find the best treatment plan when clinicians or medical students conduct clinical research or medical experiments, the homogeneity problem can be taken into account in meta-analysis and multiple combinations can be used to examine authenticity and reliability of experiments. Studies from the same qualitative source at the same time can propose effective programs based on the results, and the data is more convincing. Psoriasis is a common autoimmune disease in which the basic skin damage is erythema with multiple layers of silvery-white scales. Psoriasis affects less than 100 million individuals worldwide. Beata, et al. [1], found that patients generally have moderate acceptance of the disease, with low life satisfaction and moderately deteriorating quality of life. Among them, the duration of the disease significantly affects patient’s life satisfaction, stigma and quality of life. Studies have found that it typically takes 8-10 years from topical treatment to mild and higher intensity treatment, namely systemic treatment [2]. The prevalence of psoriasis is rising every year in China as a result of the country's accelerating urbanization, environmental pollution, heightened social rivalry, and other causes. Western medical treatments have relatively serious side effects and little safety. According to studies, traditional Chinese medicine has a long history in the treatment of psoriasis, and in recent years, it has been successful in curing 77% of cases [3,4]. The current state of traditional Chinese medicine supports the use of "blood based treatment" as one of the most significant therapeutic modalities for psoriasis. The ineffectiveness of traditional Chinese medicine has been confirmed by several researches, nevertheless, and the disease will worsen if traditional Chinese medicine is used erratically [5]. Of course, every doctor has their own perspective on this disease, but the generally recognized belief is that it has something to do with blood. Some Chinese medicines have the effect of promoting blood circulation and removing blood stasis, which can produce obvious results in the treatment of psoriasis [6]. It is also mentioned in related books that Angelica sinensis, Radix rehmannia and safflower can inhibit epidermal cell proliferation when they reach high concentrations [7]. Relevant studies have proved that traditional Chinese medicine can regulate the blood of psoriasis patients and help in treatment [8]. In addition, Marwa, et al. [9] also found that the level of plasma gelin in patients with psoriatic arthritis was lower than the normal level, suggesting that plasma gelin was closely related to psoriasis. Human monocytes are encouraged to differentiate into highly pro-inflammatory macrophages that resemble psoriasis-related phenotypes by IFN-γ [10]. von Willebrand Factor (vWF) is a marker of angiogenesis, hypercoagulability, and inflammation, and serum vWF can be a better marker of psoriasis severity than PASI [11]. Hillary, et al. [12], found that patients with psoriasis had a higher incidence of venous thrombosis. There are many arguments for implementing the "blood based treatment".
Psoriasis is also called "white mange" and "psoriasis", and the blood treatment is divided into three types: Blood heat, blood dryness and blood stasis. The most frequent type of blood heat requires treatment primarily for blood cooling, nourishing blood and promoting blood circulation. Mopane bark, locust flower, raw Rehmannia, and other medications for lowering blood pressure and enhancing blood circulation are used in the "treating from blood" theory [13]. Although traditional Chinese medicine is widely used in the treatment of psoriasis, there are many clinical trials, but the original reports rarely describe the trial design in detail. Based on this, many studies have a tendency to evaluate the effectiveness while ignoring the observation of adverse reactions. Therefore, this study starts from the "blood based treatment", summarizes and analyses some cases of current Chinese medicine treatment, and determines the objective, safe and effective view of "blood based treatment" in order to serve as a guide for the clinical treatment of this disease and assist in the selection of the best program.
Data source
Start with "1 MeSH descriptor: Psoriasis explode all trees, 2 MeSH descriptor: Medicine, Chinese traditional 1 and 2 "for Cochrane search.
Search with "1: Nail psoriasis/or experimental psoriasis/or "psoriasis area and severity index"/or pustular psoriasis/ or psoriasis vulgaris or psoriasis severity index/or psoriasis/ or guttate psoriasis/or erythrodermic psoriasis/or scalp psoriasis/(78808) “2: Chinese medicine/(44749)” “3: Randomized controlled trial/ (683261)” “4: 1, 2 and 3 (30) "Search embase for retrieval”. Search PubMed for "(psoriasis) and (Chinese medicine) and (randomized controlled trial)".
Take "title or keyword=psoriasis+psoriasis+psoriatic+pinoderma+ psoriasis+nuchalsore+psoriasisvulgaris+neurodermatitis+chronic simple lichen+psoriasisvulgaris+psoriasisvulgaris+chronic simple lichen and title or keyword=Chinese medicine+Chinese traditional medicine+traditionalChinese medicine and pharmacy+Chinese medicine+traditional Chinese medicine+traditional Chinese medicine+traditional Chinese medicine+traditional Chinese medicine and title or keyword=RCT+randomizedcontrol+rand omized+control " is a searchable search for Chinese science and technology journal full-text database (VIP).
Take "title or key words: (Psoriasis or psoriasis or white mange) and title or key words: (Chinese medicine or Chinese medicine or Chinese medicine or Western medicine) and title or key words: (Randomized control) not all: (Systematic review or meta-analysis or quality evaluation) not All: (rat or rabbit or dog) " was searched for Wanfang database.
Take "(subject: Psoriasis (accurate)) or (subject: psoriasis (accurate)) or (subject: White mange (accurate)) and (subject: Chinese medicine (accurate)) and (subject: Randomized control (accurate)) not (subject: Systematic review (accurate)) not (subject: Meta- analysis (accurate)) not (subject: Meta-analysis (accurate)) not (subject: Mouse (accurate)) "was used to search the China Journal Full-Text Database (CNKI). Each database was searched from the earliest time of inclusion in the database to January 2022.
Inclusion and exclusion criteria
Inclusion criteria: Patients with primary and recurrent psoriasis, whose diagnosis was confirmed by examination and met the criteria of Chinese clinical dermatology (Jiangsu Phoenix Science and Technology Publishing House 2017) and clinical diagnosis and treatment guide-dermatology and venereal diseases (People's Medical Publishing House, 2006).
Intervention measures: Carbertriol and other non-traditional Chinese medicines were used to treat the control group. In the experimental group, the drugs in blood classification of TCM decoction should be greater than or equal to five flavours or greater than or equal to half of the total number of drugs. For the classification and judgment of the efficacy of TCM, refer to the fifth edition of the new century in Chinese pharmacy (China traditional Chinese Medicine Press 2021).
Outcome indicators: Effective rate, Psoriasis Area and Severity Index (PASI) score, adverse reactions, etc. Type of study: Randomized controlled trial, regardless of country, region, time, and other restrictions, whether blind or not. All literatures reported complete data, including the number of observers, male to female ratio, drug composition, drug duration, observation index and other indicators.
• Irrelevant literature and duplicate literature.
• Literature on other psoriasis medications or treatment regimens, such as UV exposure.
• Basic research such as animal experiments, in vitro cell tests, etc.
• Literature quality evaluation and information extraction.
• The quality of the included literature was assessed according
to the Cochrane reviewer's handbook 5.1.0 evaluation criteria
and tools. When it was necessary to extract critical information,
the two researchers worked separately to do so independently,
and they then collaborated when they disagreed. Information
extracted included the researcher's name, publication date,
level of literature, and other factors.
Data collation and analysis
All the selected data were collated using Excel 2016 and Meta- analysis was performed using RevMan5.1 software provided by the Cochrane collaboration. Some of the data were counted using efficacy analysis statistics. Each effect size was estimated at 95% CI, and the data were measured by mean difference and 95% CI. The X2 test was performed to determine whether the results were heterogeneous. Each study needs to be statistically rigorous (p>0.1, 50%) [12], clinically homogeneous, and use a fixed effects model before merging and evaluating the data. On the contrary, the source of heterogeneity is studied, and all factors that may cause the problem are taken into account and analyzed. The random effects model is utilized directly if the data are homogeneous. Descriptive analysis will be used if the clinic's heterogeneity is too great or visible (Figure 1).
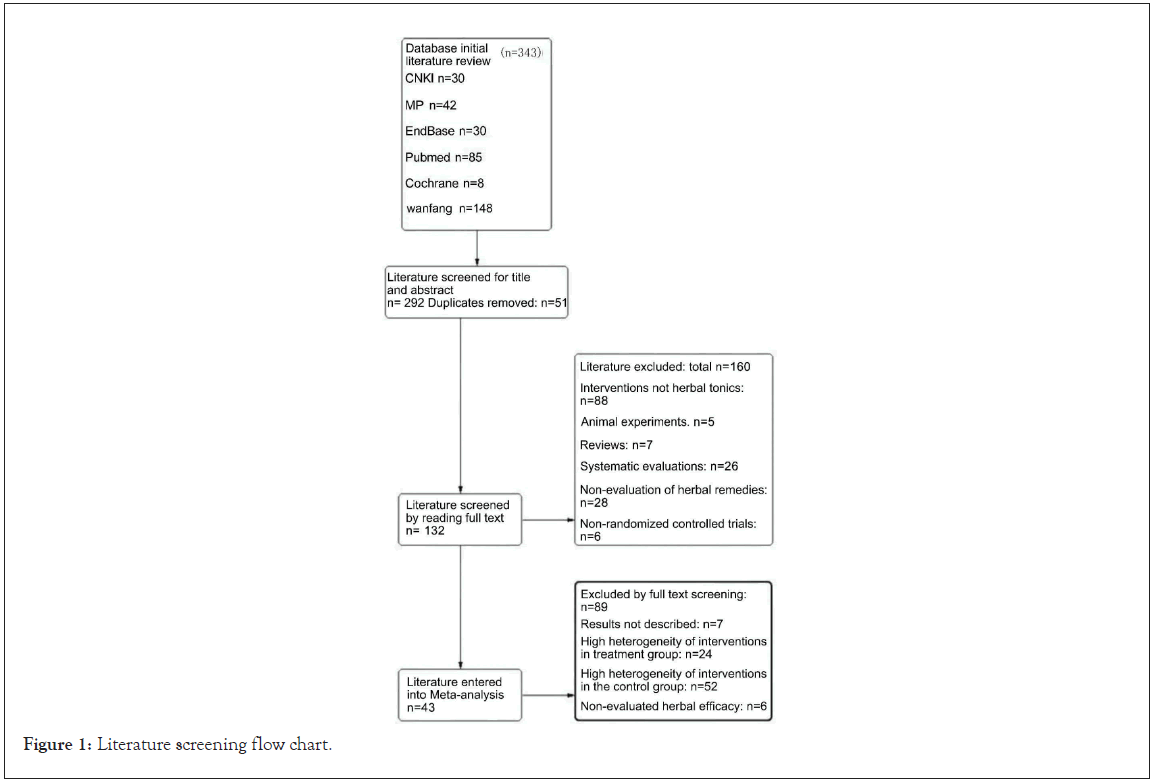
Figure 1: Literature screening flow chart.
A total of 4150 subjects were included in 43 studies, with 2336 cases in the experimental group and 1814 cases in the control group. There were 238 cases in the largest sample and 21 cases in the smallest sample. 30 studies were compared with Western medicine, and 13 studies added traditional Chinese medicine prescriptions on the basis of Western medicine, as shown in Table 1.
| Sample size | Age (average) | Sex (m/f) | Drug procedures | Drug composition | Comparator | Medication regimen | Observation index |
|---|---|---|---|---|---|---|---|
| 40/40 | I: 35.24 ± 2,14 C: 35.19 ± 2.45 | T: 26/14 C: 25/15 |
Nourishing blood and eliminating pimple soup, compound glycyrrhizin, vitamin A capsules | Chicken blood vine, hu ma ren (Sesame (black) Seeds) 30 g each, Angelica sinensis, paeoniae alba, rhizoma Dioscoreae, rhizoma Ligustici Chuanxiong, poria cocos, Tribulus terrestris, cortex Pseudostellariae, Glycyrrhiza uralensis. | Glycyrrhiz in complex, vitamin A capsules | 8 weeks | Time to resolution of lesions, time to resolution of itching, PASI score, body temperature, total lesion area, anxiety |
| 32/32 | T:30.42 ± 8.57 C: 33.34 ± 8.21 | T: 18/14 C: 17/15 |
Activating blood and dispersing blood stasis and eliminating silver soup | Sanguisorba, Atractylodes, Macrocephala, peach kernel, saffron, cinchona berry ghost arrow feather e-flowering, Salvia officinalis, Pericarpium ternatum, Snake tongue, Salvia miltiorrhiza, pericarpium citri reticulatae. | Vitamin A tablets | 8 weeks | PASI scores, blood rheology tests, and conventional physiologic markers |
| 60/60 | T:35.20 ± 2.21 C: 34.90 ± 1.98 | T: 29/31 C: 28/32 |
Developmental stage-Sophora japonica drink stationary stage-Tao Hong Si Wu Tang 3 decline stage Angelica sinensis drink | Developmental stage-tu Sophora Drink: Tu fu ling, cicada molt, Angelica, red peony, Tribulus terrestris, white fresh skin, silver flower, licorice. Stationary phase I-tao hong si wu tang: Peach kernel, safflower, Atractylodes macrocephala, poria, ijutsu, Saponaria, Lupinus, Angelica sinensis, rhizoma ligustici chuanxiong, quanchuan snail, motherwort, Forsythiag. Receding period-dang gui drink: Dang gui, fenghuang, rhizoma ligustici chuanxiong, jing mustard, Paeonia lactiflora, Tribulus terrestris, Polygonum multiflorum, Rehmanniae, rhizoma Glycyrrhiza uralensis. | Vitamin A capsules | 8 weeks | Criteria for diagnosis and efficacy of Chinese medicine diseases, PASI Score |
| 317/90 | 13-64 | 245/162 | Anti-silver pill | Dandelion, white seaweed, comfrey, red peony, honeycomb, raw earth, ginseng, green dai, whole snail, snake, cicada slough, windbreak, large centipedes. | Biketazin | 4 weeks | 4-week efficiency, recurrence rate |
| 33/32 | T:37.73 ± 111 .711 C: 39.34 ± 15 485 |
I: 21/12 C: 22/10 |
Add flavor to cool blood and eliminate wind | Buffalo horn powder, rhizoma Dioscoreae, peony, pi, lien coarse, stiffener, Dirofilaria, Zingiber officinalis, Morus alba, rhizoma Glycyrrhiza uralensis uralensis uralensis uralensis, Rhizoma Glycyrrhiza uralensis, rhizoma ginseng, and rhizoma chasteberry. | Vitamin A capsules | 8 weeks | PASI score, clinical efficacy determination, itchiness score, dermatologic quality of life score |
| 54/57 | T:38.96 ± 1 0.68 C: 41.12 ± 1 0.17 | T: 45/9 C: 42/15 |
Psoriasis 1 formula | Poriacocos, Bupleurum chinense, rhizoma cyanocarpae snake tongue, Sempervirens, peak fungus, sichuan peony, zedoary plantago ovata, dictyostelium pseudostellariae, rhizoma dandelion, rhizoma rheum, Glycyrrhiza uralensis, dee silver tablet, basic treatment | Di-Silver tablets, basic treatment | 4 weeks | PASI score, Chinese medicine efficacy, quality of life, safety assessment |
| 17/16 | T: 38.8 ± 4.6 1 C: 37.5 ± 5.3 | T: 10/7 C: 9/7 |
Clearing away heat and activating blood circulation, pou Lien poultice bath | Rehmanniae praeparata, rhizoma Cymbopogonis, poriacocos, rhizoma zizoma ginseng, Salvia miltiorrhiza, Mu dan pi, Angelicae sinensis, paeoniae alba, Angelicae sinensis | Vitamin A capsules, poulien poultice baths | 4 weeks | PAS I score |
| 100/10 | T: 27 ± 5.1 C: 25 ± 3.7 |
T: 43/57 C: 4 |
Internal herbal medicines Developmental stage tuhuai drink. Stationary stage-JiaweiSiwu Tang. Waning stage Paeonia lactiflora and zaijutsu tang. External Chinese herbal medicine: Wet compresses, packs, or medicated baths |
Internal herbal medicines developmental stage: Poriacocos, Sophora japonica, Glycyrrhiza uralensis, Glycyrrhiza Glycyrrhiza Glycyrrhiza glabra. Static phase: Rehmanniae praeparata, Paeonia lactiflora, Angelicae sinensis, rhizome ligusticic huanxiong, rhizoma Atractylodis macrocephalae, rhizoma dampiflora, Rhizoma Glycyrrhiza uralensis, Rhizoma chai hu. Receding stage: Zaijiao, sanleng, yanhuisuo, paeoniae alba, Angelicae sinensis. |
Compound glycyrrhizin | 4 weeks | Refer to the efficacy criteria for psoriasis in the diagnostic and therapeutic criteria for TCM Dermatology Diseases to determine the efficacy of the disease |
| 50/50 | T: 27.9 ± 3.9 C: 28.6 ± 4.2 |
T: 27/23 C: 28/22 |
Blood-heat syndrome: Tu-Wui-Tang. Blood-dryness syndrome Tia-Wei Si Wu Tang. Blood stasis syndrome: Red Paeonia lactiflora and RhizomaAtractylodisMacrocephalae plus compound licorice acid glycoside injection, topical tacalcitol ointment herbal baths |
Blood-heat syndrome: TuSuo Tang: Tu Fu Ling, Sophora japonica, Glycyrrhiza uralensis, Blood-dryness syndrome Jia Wei Si Wu Tang: ChuanXiongLigustici, Angelica sinensis 15 g, Paeoniae alba, Pseudostellariae alba, rehmanniae praeparata, Scutellariae fructus, Pseudostellariae Chinese yam, Atractylodes macrocephala, Atractylodes macrocephala, jujube. Blood stasis: Red peony and myriad arts soup with the addition and subtraction of: Sanguisorba, Atractylodes macrocephala, Ligusticum, chuanxiong aroma lanceolata, Paeonia lactiflora, Andrographis paniculata, peach kernel, guizhiporia cocos, paeoniae alba, Hyssop, rhizoma Scrophulariae, leeches, fructus Araceae. |
Compound glycyrrhizin | 3 weeks | According to the efficacy criteria for acute psoriasis in the diagnostic efficacy criteria for Chinese medicine diagnosis of medical cases |
| 60/60 | 30.3 ± 8.6 | 70/50 | Anti-silver and detoxification soup, with 10% sulfur ointment | Buffalo horn tablet, Panax quinquefolium, Meng xiu, bai xian pi and poria cocos, honeysuckle, dampy, rhizoma sheng di, paeoniae alba, rhizoma ginseng. | Vitamin A capsules | 4 weeks | Efficacy determination, psoriasis serum IFN-1 TNF-Ot and IL-1 levels |
| 24/24 | T: 32.0 ± 8.5 C : 34.0 ± 7.8 |
T: 10/14 C: 12/12 |
Anti-scar drink, chloramphenicol dexamethasone cream | raw white peony, Angelica, ravchigou, asparagus, Ophiopogon, chasteberry, morusofficinalis, morusofficinalis semen euryale, semen nigrum, Atractylodes macrocephala, Coix lacryma, cortex alba, rhizoma polygonati odorati, rhizoma polygonatium vulgaris. | Vitamin A capsules, oxytetracyclinedexamethason cream | 8 weeks | Determination of efficacy |
| 64/62 | 36.0 ± 13.5 | 71/55 | Five roots soup for cooling blood | Blood-heat evidence prescription: Bupleurum officinale, radix rhizoma shengdi, Sinensis, rhizome Ziziphi, rhizoma, radix, minus the rad18. Glycyrrhiza, Glycyrrhiza glabra, blood stasis evidence, radix Salviae miltiorrhiza: Blood dryness evidence add radix rhizome Polygonatum. | Vitamin A capsules | 6 weeks | Effective rate in 5 weeks, according to the efficacy standard for psoriasis in the diagnostic efficacy standard for dermatologic diseases in traditional Chinese medicine |
| 56/56 | 35.8 ± 3.9 | 60/52 | Qingying tang, vitamin A capsules | Buffalo horn, rehmanniae praeparata, rhizoma, ginseng, bamboo leaf heart, Ophiopogon, Salviae miltiorrhizae, rhizoma, polygonati odorati, honeysuckle, Forsythiae. | Vitamin A capsules | 1 month | Effective rate in 1 month, with reference to the diagnostic and therapeutic efficacy criteria for Chinese medicine certificate |
| 35/35 | 41 | 48/22 | Chinese herbal soup, compounded, Glycyrrhiza uralensis, Glycyrrhiza glabra capsule, vitamin soft gels A | Rehmanniae praeparata, comfrey, Bupleurum, Sophorae, Glycyrrhiza uralensis, rhizoma Glycyrrhiza uralensis, Rehmanniae and Forsythiae | Compound glycyrrhizin | 8 weeks | 2-month effectiveness rate |
| 30/30 | 19-63 | T: 19/11 C: 16/14 |
Anti-silver soup | Sambucus root, Sempervirens, red vine, Phalaenopsis cornu-cervi, pantotrichum, rehmanniae praeparata, mudan pi, Sophora Japonica, gentianamacrophyllae, poriacocos, poria cervipantotrichum, escargot, centipedes, pseudostigmata, ghost arrow feather, red peony | Dipyridamol | 8 weeks | PASI score, 2- month effective rate |
| 38/38 | T: 18-76 C: 16-60 |
T: 22/16 C: 20/18 |
Five roots soup for cooling blood | Comfrey, dandelion, rhizoma Dioscoreae, rhizome Cymbopogonis, herba Cuspidatae, Paeoniae lactiflorae, Daphne, and snake wushu, Angelica sinensis, licorice for blood dryness, add bamboo; for blood stasis, on the basis of this formula, reduce leucocephala root and adddanshen. | Vitamin A capsules | 4 weeks | PASI score |
| 30/23 | T: 18-67 C: 16-60 |
T: 20/1 0 C: 15/8 |
Chinese medicine soup, di yin tablets | Comfrey root, demerara, Paeoniae alba, dandelion, Ginkgo biloba, buffalo horn, danpi, niulaozi, ban yi root, yuan ginseng | Dipyridamole | 1 month | 1-month effectiveness rate |
| 22/20 | 37.6 A ± 15.1 | 12632 | Topical lotion, skin methotrexate, salicylic acid cream | Panax quinquefolius, Artemisia argyi, semen Aristolochiae, Paeoniae, fetidis macrocephalae, Salviae miltiorrhizae, folium Cyperus rotundus, fructus Schisandrae chinensis, fructus Momordicaulis | Methotrexate, lactacycline salicylate | 6 weeks | 6-week efficiency, PASI score |
| 35/30 | T: 3-18 C: 4-17 |
T: 13/22 C: 10/20 |
- | Buffalo horn, Poria, cocos, rhizoma glycineae, Scutellariae, rhizoma polygonati odorati, rhizoma Dendrobium, rhizoma Dioscoreae, rhizoma Cymbopogonis, rhizome Platycodonis | Penicillin (Antibiotic) | 4 weeks | 1-month effectiveness rate |
| 85/45 | T: 11-70 C: 15- 56 |
T: 40/45 C: 35/10 |
Cleansing silver detergent | Rehmanniae praeparata, honeysuckle, poria, thorny bush, ume fenghuang, safflower, Paeonia lactiflora, san leng, mejiao, Tribulus terrestris, Rhizoma lappalianshi. | Salicylate soft tone | 20 days | Efficient |
| 40/34 | 52 | 40/37 | - | Scutellaria baicalensis, rhizoma ginseng, Mentha piperita, Scrophulariae praeparata, rhizoma Ophiopogonis, rhizoma Psoralea, rhizoma Polygoni multiflori, rhizoma lianzhi | Compound glycyrrhizi acid, topical allantoin emulsion | 4 weeks | 1-month effectiveness rate |
| 200484/38 | T: 18-67 C: 22-68 |
T: 54/30 C: 23/15 |
Bath No. 1, proposed bath No. 2 | One, raw rhubarb, cypress, bitter ginseng, tiger nut, snakebite, dandelion, Angelica dahurica, chrysanthemum, shilupu, saffron, Mentha piperita, Mangosteen Withered alum Second, the large. raw ground, the whole Angelica, chicken blood vine, prickly five plus skin, the skin of the bones, seven leaves of the flower of one branch, hsu changqing, sedgewick quinoa, hang baichu, weiling xian, broussonetiakasumiga leaves, sapindales, Salvia miltiorrhiza, peppercorns | Anthralin soft drug | 8 weeks | 2-month efficiency, PASI score |
| 44/16 | T: 47.36 A ± 12.02 C: 49.27 A ± 13. 88 |
T: 28/16 C: 10/6 |
Silver chip joint soup compound | Poria, cocos, grass moss, raw earth, terrestris, Angelica, geode, Acacia, white fresh peel, Tribulus windbreak, danshen, red peony, white peony, lonicera japonica, Saxifrage, maitake, dan shi, xuan shen, licorice and many others. | Leflunomide methotrexate | 12 weeks | Laboratory score, 12-week |
| 30/26 | 37 | T: 38/18 | Praeparata, Pseudostellariae, fructus Ophiopogonis, fructus Rehmanniae, fructus Cynanchum, fructus bone skin, fructus Turbinatus, Salviae miltiorrhizae, rhizoma saffron, Angelicae sinensis, rhizoma ginseng, semen Aristolochiae, fructus beehive. | Vitamin A capsules, dexamethasone urea cream | 4 weeks | 4-week efficiency | |
| 60/40 | T: 27.9 A ± 3.9 C: 28.6 A ± 4.2 |
T: 27/33 C: 22/28 |
Cooling blood and clearing silver education. Soup, compound glycyrrhizin, tacalcitol soft |
Tang plus reduction. herbal external washing: Raw lateral cypress leaves, tu Sophora soup, Jia wei si wu tang, red peony I shu, Turbinaria, white fresh skin, large Saponaria, diagnosis and addition and subtraction: Blood-heat type plus Amaranthus, Septoria, dandelion; blood dryness type plus bitter ginseng, dicotyledonous, blood stasis type plus mudanpi, raw mugwort leaf. | Xia fang Glycyrrhizin | 6 weeks | 6-week efficiency rate |
| 30/30 | T: 45 C: 43 |
T: 18/12 C: 16/14 |
Clear yin and detoxify poisonous soup | Poria, cocos, Cynanchum, honeysuckle, Salvia miltiorrhiza, Panax notoginseng, cornu cervi pantotrichum, dijin cao, sheng shiyu, Scutellaria baicalensis, rhizoma Dioscoreae, semen aesculi, semen bianchi, Curcuma longa, fructus Psoralea. | Dipyridamole | 8 weeks | 8-week efficiency rate |
| 45/45 | T: 18-57 C: 17-56 |
T: 24/21 C: 26/19 |
Chevron southwest soup | Shouwu, Forsythia, comfrey, dandelion, white fresh skin, raw earth, big green leaf, gold silver flower, salvia, gardenia, Angelica, Licorice. | Vitamin A capsules | 8 weeks | S-week efficiency |
| 84/50 | T: 40 C: 31. 4 |
T: 60/22 C: 30/20 |
Botulinum toxin capsule, Shuanghuanglian powder injection combined with compound danshen injection, traditional Chinese medicine steaming | Cooked Bupleurum, ligusticum ground, danpi, raw chuan xiong, wolfberry, ground, aloe, paeony, purslane, Scutellaria, skin, danpi, honeysuckle, raw ground. | polypeptide | 4 weeks | PASI score, 4-week effective rate |
| 66/66 | T: 39.0 A ± 5 .3 C: 38. 4 A ± 4.9 |
T: 40/26 C: 37/29 |
Clearing heat, cooling blood and removing toxins soup | Rehmarniae Praeparata, Bupleurum chinense, Sophora japonica, fructus Gingivalis, Zizyphus, Paeoniae alba, fructus Bupleurum, rhizome polygonati odorati. | Vitamin E capsules | 6 weeks | PASI score, 6-week effective rate |
| 68/50 | 36 | 461/57 | Blood-heat type: Scutellaria baicalensis, rhizome sheng di, rhizoma dandelionis, rhizoma Dioscoreae, Salviae miltiorrhizae, oyster, Paeoniae lactiflorae, san leng, ljiao, safflower, anemia add motherwort, Angelica. Blood stasis type : Salvia miltiorrhiza, Angelica, chuan xiong 30 g each, mother-of-pearl, stone, chaihu, peach kernel, safflower, umeboshi, dandelion, red peony, Hyssop, ripened earth, yujin. | Dee silver tablets, avi A. Some loyalists depending on the condition, topical beta-carotene may be used | 8 weeks | PASI score, 8–week effective rate | |
| 32/30 | 47 12 | 45/17 | Salviae miltiorrhizae, rehmanniae praeparata, rhizoma Ophiopogonis, rhizoma polygonati odorati, rhizoma Cinnamomum cassia. | Vitamin A capsules | 12 weeks | PASI score, lesion area score, 4, 8, 12 effectiveness rate | |
| 62/62 | T: 38. 2 A ± 10.3 C: 38.5 A ± 10.1 |
T: 32/30 C: 33/29 |
Cooling blood and removing blood stasis with vegetable wind soup | Comfrey, rehmanniae praeparata, Polygonum multiflorum, poriacocos, Angelicae sinensis, paeoniae alba, rhizoma ginseng, Ophiopogonis paniculata, Angelica dahurica, herba Euphrasiae, fenghuang. | Calcipotriol betamethasone ointment | 4 weeks | PASI score |
| 40/40 | T: 35.3 C: 37.8T |
T: 22/18 C: 23/17 |
Gramophone I | Rhizoma zizoma, paeoniae alba, rehmanniae praeparata, rhizoma saffron, Angelicae sinensis, rhizome chuan chuan, buffalo horn powder, centipedes, Scutellaria baicalensis, Forsythia. | Vitamin A capsules | 12 weeks | PASI score, 12-week effective rate |
| 41/30 | T: 42.5 C: 37.5 |
T: 21/20 C: 16/14 |
Anti-silver 1 | Rehmanniae praeparata, rhizoma alba, poriacocos, Salviae miltiorrhizae, Sophorae, Glycyrrhiza uralensis uralensis, zizoma Glycyrrhiza uralensis, rhizoma paeoniae alba, Polygala. | Vitamin A capsules | 8 weeks | PASI score, 8- week effective rate |
| 38/37 | 22-51 | 49/26 | - | Blood-heat type: Poriacocos, white fresh skin, Lonicera japonica, Cao he che, rhizoma, pyridium, Paeonia lactiflora, da qing ye, bei dou gen, Sophora japonica, zi cao. Blood- drying type: Rhizoma, Dampyridium, Paeonia lactiflora, Corylus officinalis, Bitter ginseng, Ophiopogon flexuosus, xuanshen, dangshen, Pseudostelloria sinensis, bei dou gen. Blood-attacking type:rhizoma, Dampyridium, Paeonia lactiflora, Dang Gui Tail, ChuanNiuhua, Salvia miltiorrhiza, tiger cane, chicken blood vine, arrow feather, cimicifuga, sanleng, peach kernel, safflower, bei dou gen. | Dipyridamole | 8 weeks | PASI score and efficacy evaluation |
| 50/46 | T: 38.9 C: 37.5T |
T: 27/23 C: 24/22 |
Chamomile | Bai-xian pi, Da qing ye, Honeysuckle, gypsum, rehmanniae praeparata, Mudan pi, paeoniae alba, rhizome zizoma, Salviae miltiorrhizae, Trigonellum, Artemisia, Jiao san xian. | Vitamin A capsules | 8 weeks | 4-week, 8-week efficiency |
| 108/66 | T: 35 C: 34 |
T: 56/52 C: 35/31 |
Dithranol ointment | Rhizoma, honeysuckle 15 g, Sophora, comfrey, Salvia miltiorrhiza, Angelica sinensis, chonglou, poriacocos, dazhongye, chicken blood vine, bitter ginseng, snake. | Dithranol ointment | 4 weeks, 8 weeks | 4-week, 8-week efficiency, PASI score |
| 55/52 | T: 32.5 A ± 8. 23 C: 33.57.89 |
T: 36/19 C: 33/18 |
Kex in Tang, Compound flumet has one ointment | Sanleng, Ijiao, Sophora japonica, Dangpi, Buffalo horn, rhizoma Dioscoreae, Polygoni Multiflori, paeoniae alba, poriacocos. | Flumethasone compound ointment | 4 weeks | DLQI scores, PASI scores and validity rates |
| 30/30 | T: 38.891 ± 10.24 C: 40.17 ± 9.73 |
T: 19/11 C: 18/12 |
Cooling the blood, removing toxins, and transmitting tables | Poriacocos, rhizoma, cortex Eucommiae, rhizoma gigantea, Salvia miltiorrhiza, fructus psoralea, folium honeysuckle, Forsythia, Aristolochiae, rhizoma Bupleurum, folium capsicum, semen ginseng, folium candidum, semen Glycyrrhiza uralensis. | Vitamin A capsules | 8 weeks | PASI score, 8-week effective rate |
| 60/60 | T: 42.1 ± 14.6 C: 42.3 A ± 15.4 | T: 28/32 C: 26/34 |
Anti-silver malaria soup, vitamin A capsule | Buffalo horn powder, rehmanniae praeparata, Paeoniae lactiflorae, poriacocos, Panax quinquefolium, fructus bupleurum, rhizome gastrodiae, rhizome ziziphiella asiatica, cicada Moluccus, Scutellaria baicalensis, fenpao fenghuang, Bupleurum chinense, rhizome Atractylodis macrocephalae. | Vitamin A capsules | 8 weeks | PASI score, 8-week effective rate |
| 30/30 | T: 37.12 ± 8.56 C: 36.98 ± 8.37 | T: 16/14 C: 17/1 |
Anti-mumps soup | Ginkgo biloba, Forsythia, Echinacea purpurea, dandelion, Rehmanniae, cortex Eucommiae, honeycomb, Scutellaria, saffron, peach kernel, leech, Faganxia. | Avicenna capsules | 12 weeks | PASI score, 12-week efficacy rate |
| 36/36 | T: 41. 4 A ± 3 .5 C: 39. 2 A ± 2.4 |
T: 20/16 C: 18/18 |
Chowder | Antelope horn powder, rehmanniae praeparata, thorium cortex, Forsythia, Bupleurum, Paeoniae lactiflorae, Panax quinquefolium, rhizome polygoni multiflori, honeysuckle flower, rhizome dandelionae. | Vitamin A capsules | 12 weeks | PASI score, DLQI score |
| 21 | 48. 52 | ( 14/7 ) | - | Ephedra 6 g, Pseudostellariae, rhizome polygonati odorati, cinnamon dried ginger, antler cream, rhizome dioscoreae, Paeonia lactiflora, Salvia miltiorrhiza, fenugreek, comfrey, Sophora japonica, Glycyrrhiza uralensis uralensis uralensis Glycyrrhiza Glycyrrhiza glabra, Cynanchum officinale. | Methotrexate (A family medicine) | 6 months | PASI score, PGA |
Table 1: Basic information of study parameters.
Quality evaluation
The quality of the original studies included in this systematic review was generally low. All 43 studies described randomization, but only 9 studies used appropriate randomization methods, 3 were inappropriate randomization methods, 9 studies reported selection bias sources, 12 studies reported loss of follow-up, 2 studies reported assignment blindness, and no detection bias was reported in any of the studies. See Figure 2 for details.
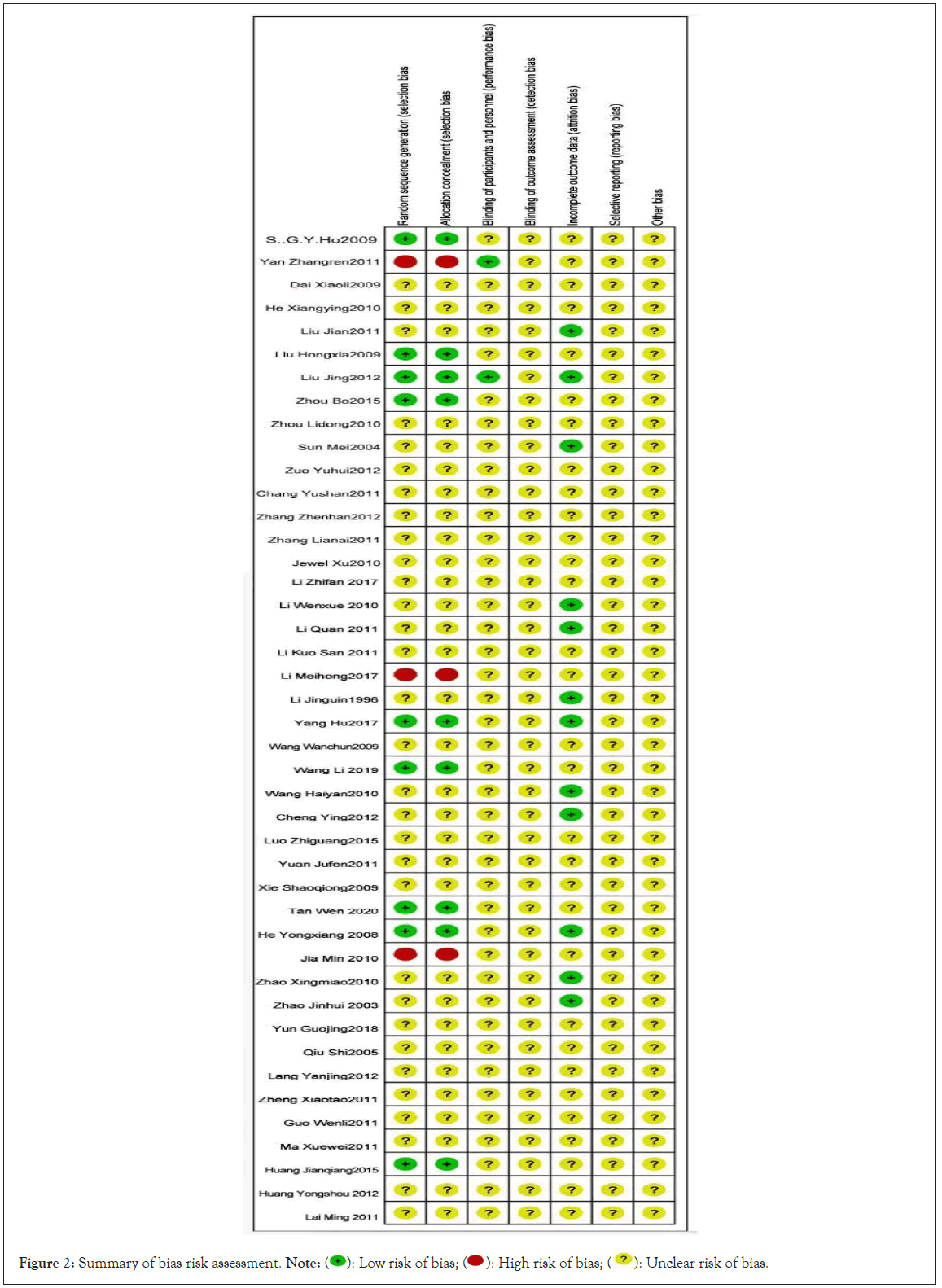
Figure 2: Summary of bias risk assessment. Note: 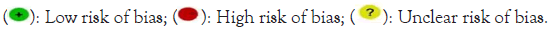
Effectiveness analysis
A total of 30 cases were included in the study, all of which had effective rates. They were divided into groups of 4 weeks, 6 weeks, 8 weeks and 12 weeks, and subgroup analysis was conducted for them respectively. The combined results were four weeks, six weeks, eight weeks, or 95% CI in the order of 1.09(1.04,1.14), 1.16(1.07,1.27),1.12(1.06,1.18),1.13(1.01,1.28), as shown in Figure 3. The one of each time point was <50%, and the results revealed that: The four time points of the two groups were statistically compared. There were 13 literatures on the use of both Chinese and Western medicines in combination, 11 of which discussed the effective rate. The effective rate was divided into three weeks, four weeks, six weeks, eight weeks and twelve weeks, and subgroup analysis was conducted for each result. The results were all <50%, and then the fixed effect model were used for the combination. The results showed that there were statistically significant differences between the two groups at four weeks and eight weeks, and the combined results showed or 95% CI, respectively: 1.23(1.15, 1.32), 1.04(0.95, 1.10), but at three and six weeks, the results showed no statistically significant difference, as indicated by the combined results or 95% CI, which were 1.27(1.06, 1.52), 2.05(1.15, 3.62), as shown in Figure 4.
Figure 3: Efficiency of Chinese medicine group vs. Western medicine groups.
Figure 4: TCM combined with Western medicine vs. Western medicine.
Recurrence rate
Chinese medicine group vs. Western medicine group: Relapse rates were reported in 11 studies, which were divided into 4 weeks, 12 weeks, 24 weeks, 1 year and 2 years according to follow-up time. Subgroup analysis of them showed no statistically a significant difference in recurrence rates between the two groups at 4 weeks and 12 weeks. Or if 95% CI was 0.60(0.22,1.62), 0.08(0.00,1.46), there was no statistically significant difference in the recurrence rate at 24 weeks,1 year and 2 years. The combined results at 24 weeks showed either a 95% CI of 0.46(0.28,0.77), the combined results at one year showed either a 95% CI of 0.18(0.12,0.28), and the combined results at two years showed either a 95% CI of 0.29(0.10,0.82), as shown in Figure 5.
Figure 5: TCM combined with Western medicine vs. Western medicine.
TCM combined with Western medicine vs. Western medicine: A twelve-week anytime visit period was used in a study that discussed the recurrence rate; the findings revealed that there was no recurrence at that time.
PASI score
Figure 6 illustrates a comparison of the clinical effectiveness of Chinese medicine and Western medicine. Ten investigations on PASI scores were conducted with follow-up periods of four, eight, twelve, and six months. The comparison of the two groups' PASI scores is shown in Tables 1 and 2. As you can see, both groups' PASI scores after therapy dramatically decreased from their pre-treatment levels, which were not statistically significant. Four studies showed that the rate of deterioration was slower in the treatment group and faster in the control group. In contrast to those four researches, six studies reported results that showed a faster rate of decline in the treatment group and a slower rate of decline in the control group. In all but one trial, the differences were statistically significant (p<0.05).
Figure 6: Chinese medicine group vs. Western medicine group. Note:  Control group pre-treatment points;
Control group pre-treatment points;  Control group post-treatment points.
Control group post-treatment points.
Comparison of clinical efficacy between TCM combined with Western medicine group and Western medicine group is illustrated in Figure 7. These studies showed that PASI score results could be obtained, and the time points were recorded in the 4th, 8th and 12th weeks. The differences of PASI before and after treatment between the two groups of patients can be seen in Table 1. Before treatment, there wasn't much of a difference between them, and the statistical significance was minimal. After treatment, both the experimental group and the control group's PASI exhibited a significant downward trend. One study showed that the downward trend in the treatment group was much higher than that in the control group, and three studies showed the opposite, indicating that these differences were statistically significant (p<0.05).
Figure 7: Chinese medicine group vs. Western medicine group. Note:  Control group pre-treatment points;
Control group pre-treatment points;  Control group post-treatment points.
Control group post-treatment points.
"Inverted funnel" analysis
The traditional Chinese medicine group was compared with the western medicine group, and the traditional Chinese and Western medicine group was compared with the Western medicine group. Clinical trials were taken to analyze the two groups’ respective effective rates and recurrence rates. It is evident that the clinical effective rate of the two groups' funnel diagrams is symmetrical. The clinical recurrence rate of the two groups is shown to have a significantly asymmetrical funnel plot, indicating a large potential bias. The two funnels are each symmetrical, showing that the bias of their effective rate is minor. See Figure 8-11.
Figure 8: Funnel diagram of effective rate of Chinese medicine group vs. Western medicine group. Note:  6 Weeks
effective rate;
6 Weeks
effective rate;  12 weeks effective rate.
12 weeks effective rate.
Figure 9: Funnel diagram of effective rate of Chinese medicine combined with Western medicine group vs. Western medicine group. Note: Funnel diagram of effective rate of Chinese medicine combined with Western medicine group vs. Western medicine group. Note: 

Figure 10: Funnel diagram of the recurrence rate of Chinese medicine group vs. Western medicine group. Note: 

Figure 11: Funnel diagram of the recurrence rate of Chinese medicine combined with Western medicine group vs. Western medicine group.
Security analysis
The 43 studies that were included in this systematic review conducted safety analysis (see Table 2 for details). 17 studies did not report any Adverse Drug Reactions (ADR), while 26 studies did. There were no significant Adverse Drug Reactions (ADRs) detected, and adverse reactions in the treatment group were generally milder than those in the control group. ADR was identified in 13 out of a total of 21 studies using acitretin as the control medication. In the treatment group, most of the ADRs occurred dry eyes, dry skin and partial pruritus, 20 cases of dry mouth, 14 cases of desquamation, 13 cases of nausea, 12 cases of diarrhoea, 12 cases of gastrointestinal discomfort, 3 cases of dizziness, 2 cases of loss of appetite, 1 case of constipation, 1 case of vomiting, and 1 case of drug rash. In the control group, most ADRs occurred intraocular dryness, skin dryness in 25 cases, skin pruritus in 21 cases, nausea in 19 cases, elevated blood lipids in 14 cases, lip dryness in 12 cases, skin mucous membrane desquamation in 12 cases, gastrointestinal discomfort in 12 cases, dizziness in 7 cases, elevated liver enzymes in 5 cases, elevated alanine aminotransferase in 4 cases, leukocytes is in 4 cases, cheilitis in 3 cases, aspartate aminotransferase in 2 cases. Abdominal pain in 2 cases, BUN1 in one, dizziness in one, tinnitus in one and elevated blood sugar in one. In the treatment group, there were 3 cases of diarrhea, 3 cases of dry skin, 2 cases of cheilitis, 2 cases of desquamation and 2 cases of pruritus. In the control group, 5 cases had skin symptom with itching, 2 with desquamation, 13 with dry skin surface, 21 with dry lip epidermis, and 16 with dry mouth. A total of 6 studies took compound glycyrrhizin as control drug, of which 5 reported ADR, most patients showed dry mouth, dry skin, mild desquamation, and some skin pruritus, including 1 case of nausea, 1 case of drug eruption, 1 case of dizziness, and 1 case of elevated blood pressure in the treatment group. In the control group, there was 1 case of skin irritation, 2 cases of a certain increase in blood pressure, 6 cases of elevated Alanine Aminotransferase (Alt), 3 studies using methotrexate as the control drug, 1 case of alopecia, 1 case of mildly elevated Alt and 1 case of stomach discomfort in the treatment group. In the control group, nausea, vomiting, and raised liver enzyme levels were frequent. One incidence of moderate alanine amino transferase elevation and two episodes of stomach distress also occurred. Only one study out of a total of two that used salicylic acid as the control medication noted any negative effects. Mild alanine transaminase and stomach upset were reported in both groups, and alopecia was also reported in the treatment group. In a total of 1 study using like to zinc as the control drug, there was no adverse reaction in the treatment group, and the white blood cells in 6 cases of the control group dropped below 4000/mm3 during the treatment period, and 4 cases developed oral ulcers. In 1 study with retinoic acid ointment as the control drug, there was no adverse reaction in the treatment group and skin irritation in 1 case in the control group. In a total of 1 study with cream as the control drug, 2 cases of mild dizziness and palpitation in the treatment group, 2 cases of lip dryness, chapping and obvious desquamation. 5 cases of dry lips, chapped, desquamated were present in the control group. Penicillin and compound aminopeptin were used as control drugs in the study, and there were no adverse reactions.
| Number | Control group | Number | Treatment group |
|---|---|---|---|
| 40 | 2 cases of elevated ghrelin transaminase | 40 | 1 cases of nausea, 1 case of drug rash, 1 case of head volume |
| 32 | Side effects mainly include dry mouth, dry lips, dry skin, loss of eyebrows, dizziness, headache, elevated liver enzymes. In 3 cases, 1 case of Increased BUN, elevated lipids in 5 cases | 32 | 2 cases of diarrhea, 1 case of constipation and vomiting |
| 60 | Not have | 60 | Not have |
| 317 | 6 cases of leukocyte drop, 4 cases of mouth stains | 90 | Not have |
| 33 | not have | 32 | 2 cases of loose stools |
| 54 | 5 cases of dry mouth and lips; 1 case of itchy skin | 57 | 2 cases of diarrhea |
| 21 | Nausea, vomiting and elevated liver enzyme levels are common. | 0 | Infections and gastrointestinal side effects have been reported, with a few experiencing liver function abnormalities. |
| 17 | 7 cases of nausea, dizziness, dry and cracked lips, and 3 cases of abnormalities in liver function, kidney function, and lipid analysis in the control group. | 16 | 3 cases of mild nausea, dry mouth |
| 50 | Most patients had dry mouth, dry skin, mild flaking, and some had itching. Two cases had elevated ghrelinase. | 50 | Most patients experienced dry mouth, dry skin, mild flaking, and some experienced itching. No serious adverse reactions were observed in the roup. |
| 35 | 1 cases of skin irritation | 35 | Not have |
| 23 | 5 dry mouth, 4 posterior treatment dryness, 7 dry skin, 4 flaking, 4 cancer itching | 30 | 2 posterior dryness, 3 dry skin, 2 flaking, 2 itching |
| 20 | 1 case of mild elevation of hepatic glutathione ( ALT ); 2 cases of gastric upset with occasional nausea and non - vomiting |
22 | One case of alopecia areata; one case of mildly elevated liver ALT. (500/L), the drug was not stopped during the treatment period, and the liver function was normalized after hepatoprotective treatment such. As hepatoprotective tablets were given, and the examination was still normal one month after the drug was stopped; stomach discomfort 1 case, the drug was not stopped and the dosage was not reduced. Symptoms were relieved after giving symptomatic treatments such as protecting the gastric mucosa. |
| 35 | Not have | 30 | Not have |
| 40 | 2 cases of elevated blood pressure | 34 | 1 case of elevated blood pressure |
| 30 | 6 cases of dry mouth, dry lips, dry skin and generalized dehiscence, severe with fissured lips and mouth. | 30 | 1 case of diarrhea |
| 32 | All patients experienced varying degrees of dry lips with chapped lips, dry eyes, and dry skin, with some patients experiencing present with itchy skin. Two of the cases in the vitamin A group showed mild lipid. The enzyme was elevated in two cases, and alanine aminotransferase and aspartate nitrilotransferase were elevated in two cases. | 30 | All patients had varying degrees of dry lips with chapped lips, dry eyes and dry skin, and some had itchy skin cancer. |
| 30 | 5 cases of mouth shield dryness, delayed cracking, flaking mingyi | 26 | 2 cases of mild dizziness and panic, 2 cases of dry, cracked, flaky lips. |
| 60 | 2 cases of elevated glutathione 45 nil |
40 | No serious adverse reactions |
| 45 | Not have | 45 | Mild diarrhea in 3 cases, mild dry mouth and flaking in 12 case |
| 84 | Not have | 50 | Not have |
| 40 | 3 cases presented with varying degrees of labial inflammation, and seven cases presented with skin Itching, significant flaking of the takedown toe, nausea in 2 cases, abdominal | 40 | Not have |
| 41 | 25 cases of dry skin and mucous membranes, 2 cases of increased liver enzymes, lipid Increased height, headache and tinnitus in 1 case, gastrointestinal discomfort in 2 cases | 30 | Gastrointestinal discomfort 2 cases |
| 50 | 14 cases of itchy skin, 2 cases of elevated lipids, 1 cases of elevated blood glucose | 46 | 4 cases of gastrointestinal discomfort, 1 case of diarrhoea |
| 108 | Not have | 66 | Not have |
| 108 | 10 cases of stomach upset and nausea and vomiting, and 4 cases of leuko-fine cell decline | 60 | 6 cases had mild stomach upset and 2 cases had mild diarrhea |
| 30 | Not have | 30 | 6 cases of nausea, 2 cases of loss of appetite, 2 cases of membrane diarrhea |
Table 2: Summary of adverse reactions between control group and treatment group.
According to the literature [14], many medical scientists still adhere to the treatment principle of "blood based treatment", which is manifested as acute hot air of blood and chronic period of blood stasis, blood deficiency, blood dryness and other syndromes. They utilize the approaches that they believe to be beneficial for treating psoriasis, such as removing heat and cooling blood to dissipate wind, stimulating blood circulation to remove blood stasis, nourishing blood to moisten dryness, etc. Before conducting a thorough review of the literature, we established the inclusion criteria for the "blood based treatment" method, stipulating that the experimental group had to receive a traditional Chinese medicine decoction and that the blood-classified drugs in the decoction should make up at least five or fifty percent of the total amount of drugs. The judgment and classification of drug efficacy were also clearly stipulated, requiring that the fifth edition of the new century Chinese pharmacy, a planning textbook for traditional Chinese medicine in general higher education, be used as a reference basis, on which we evaluated the effect of "blood based treatment" on psoriasis.
The quality of the original literature that was summarized in accordance with the systematic evaluation has to be improved in terms of the included literature's quality. All of the research mentioned above mention randomness, but only nine of them actually use the right randomization technique. Additionally, three of the randomization procedures were incorrect and carried a high risk; nine studies' source selection was skewed; and twelve studies failed to publish their access methods. These flaws in the allocation methods of two of the studies resulted in blind spots. However, the original studies that were included in these papers were already biased, therefore the planned "blood-based" clinical trials for psoriasis have not yet been confirmed. In reality, none of these investigations found bias or any other issues.
Different category indicators, including PASI, response rate, and recurrence rate, were proposed in this study to examine the efficacy of "blood based treatment" for the treatment of psoriasis. Additionally, the therapeutic effect can be separated into two groups based on these factors. The first group compares traditional Chinese medicine and Western medicine, comparing the therapeutic effects of each, while the second group uses a combination of traditional Chinese and Western medicine and compares two different facets of Western medicine. The above plan is based on the premise of treatment effect. Patients in the first group should set a fixed time period to record their treatment conditions respectively, including the time points of 4, 6, 8 and 12 weeks, in which the recorded results show or 95% CI as follows: 1.09 (1.04, 1.14), (1.07, 1.27), 1.16 1.12 (1.06, 1.18), 1.13 (1.01, 1.28). In addition, in the second group, there was no significant difference in treatment at the third and sixth weeks, and there was a large difference between the fourth and eighth weeks, which was of high statistical significance.
Studies showed that there were only a handful of reports on the recurrence rate, among which there were 11 studies on the recurrence rate in the Chinese medicine versus Western medicine group. However, the results showed that the recurrence rate in the two groups at week 4 and week 12 was not statistically significant, with 95% CI was 0.62 (0.22, 1.62), 0.08 (0.00, 1.46). The difference in recurrence rates between the two groups was highly statistically significant at 24 weeks, 1 year, and 2 years. However, there was only one study evaluated the recurrence rate between the Western medication group and the group receiving both Chinese and Western treatment. According to the difference in the recurrence rate between the two groups, there was no statistical significance at the twelfth week, and the combined results showed that the 95% CI was 0.44 (0.28, 0.68).
By comparing PASI as an evaluation index, it is not difficult to see that the difference between the first two groups of Chinese medicine and Western medicine is not statistically significant. After treatment, PASI in both the test group and the control group showed a decreasing trend, among which, four studies showed that the control group was far higher than the treatment group, on the contrary, six studies showed that the treatment group exceeded the control group. Based on the difference, only one study was not statistically significant, while the others were (p<0.05). Additionally, there was no statistically significant difference between the traditional Chinese and Western medicine and Western medicine groups prior to treatment and both the experimental groups and the control group's PASI showed a downward trend after treatment. Three studies showed that the decreasing trend of the control group was significantly higher than that of the treatment group, and one study showed that the treatment group was higher than that of the control group, and the difference in research data was also statistically significant (p<0.05).
The results of the combined analysis above indicate that the "blood based treatment" of psoriasis has certain advantages in improving clinical efficacy, reducing adverse reactions, and reducing recurrence rate. However, due to the methodological problems included in the studies and possible publication bias, these limitations must be taken into account in the conclusions drawn.
The origin of the traditional Chinese medicine theory of psoriasis "blood based treatment" is the belief that the development of psoriasis is closely related to the activation of T lymphocytes and the cytokines produced. This belief may be an important pathological basis for the "blood based treatment" of psoriasis. Psoriasis is often caused by blood heat, a long time to consume Yin blood damage, blood dryness, blood stasis syndrome, manifested in a certain period of clinical patients often to a type, mixed with other types of syndrome. Herbal remedies for cooling blood can remove activated T lymphocytes and cytokines, cool blood and eliminate plaque, herbal remedies for nourishing blood can improve blood concentration, viscosity and aggregation [15], eliminate erythema, and correct epidermal hyperplasia and hypokeratosis [16,17]. The results of this systematic evaluation also fully show that the effect of "treating psoriasis vulgaris from blood" alone or combined with Western medicine is better than that of Western medicine, which provides full proof for our theory.
Future scope
Improve the quality of RCTs, avoid low-level duplication, pay attention to sample size estimation, randomization, blind application, and record and analysis of lost follow-up cases.
• Pay special attention to the effect of long-term treatment and recurrence rate of the disease.
• In order to better transmit the latest systematic evaluation from abroad to our country, so as to promote the better development of domestic medical service, it should be popularized on a large scale, introduce and publicize the effects and benefits of systematic evaluation.
• For most dermatologists, it is necessary to fully analyze and master evidence-based medicine, so as to understand it thoroughly.
• Since most of the literature adopts a one-end treatment method, which is contrary to the nature of Traditional Chinese medicine (TCM) treatment, the most important thing at present is to find out the treatment method that is most in line with the characteristics of TCM, and prepare for future TCM research.
The Chinese medicine in the treatment of psoriasis had less adverse responses than traditional Western medicine, and those that did occur were often modest. This suggests that using Chinese medicine to treat psoriasis is safe. Among them, the adverse reactions produced in the treatment of psoriasis are mainly dry mouth and dry skin, which is fundamentally because of the damage to the body fluid during the treatment of psoriasis. Because of this, psoriasis therapy should not only pay attention to how blood medicines are used, but also to the protection of body fluids, as this has raised the alert for us. Overall, this analysis demonstrates that the "blood based treatment" method to treating psoriasis has yielded excellent results, although further research is necessary because of the relatively low quality of the included trials.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Charles S (2024) Systematic Review and Meta-Analysis of the Curative Effect of Traditional Chinese Medicine on Psoriasis under "Blood Syndrome Theory". J Clin Exp Dermatol Res.15:654.
Received: 01-Dec-2023, Manuscript No. JCEDR-23-28479; Editor assigned: 04-Dec-2023, Pre QC No. JCEDR-23-28479 (PQ); Reviewed: 18-Dec-2023, QC No. JCEDR-23-28479; Revised: 25-Dec-2023, Manuscript No. JCEDR-23-28479 (R); Published: 08-Jan-2024 , DOI: 10.35841/2155- 9554.23.15.654
Copyright: © 2023 Charles S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.