
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 7
Context: Supraclavicular approach gives an effective block of brachial plexus with fast onset and complete block.
Aims: To analyse and compare the efficacy, safety and complications in performing supraclavicular brachial plexus nerve blocks by Peripheral Nerve stimulator (PNS) and Ultra Sound (US) guidance techniques.
Settings and design: A prospective and randomized comparative study.
Materials and methods: Patients were randomized into two groups, Group US and Group PNS consisting of 80 patients each. The amount of local anaesthetic used was 20 ml 0.5% bupivacaine + 10 ml normal saline for both the groups.
Statistical analysis used: The data from the customized proforma was analysed by using t-test, Z-test and Chi-square test. A p-value of less than 0.05 was considered statistically significant.
Results: The time to perform the supraclavicular brachial plexus nerve block was shorter in group US than in group PNS. The onset of sensory and motor block occurred earlier in the group US compared to the group PNS. The duration of block (sensory and motor) and analgesia was longer for the group US than for the group PNS.
Conclusion: Owing to real-time visualization and precise deposition of drug around the plexus, the quality of supraclavicular brachial plexus block was better for the patients in group US than group PNS.
Local anaesthetic; Nerve block; Supraclavicular brachial plexus; Ultrasound guidance; Peripheral nerve stimulator
Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage. Regional anaesthetic techniques provide a standalone method of anaesthesia for intraoperative and postoperative care. Brachial plexus blockade is a time-tested technique for the upper limb surgeries [1]. Depositing local anaesthetic close to brachial plexus temporarily blocks the sensation to disable the movement of upper extremity. There are several techniques for blocking the brachial plexus. These techniques are classified according to level of needle insertion for injecting the local anaesthetic as inter-scalene block, supraclavicular approach, infra clavicular approach and axillary block in axilla. Supraclavicular approach gives an effective block. It is carried out at level of trunks of brachial plexus, i.e. at middle of brachial plexus resulting in homogeneous spread of drug throughout plexus with fast onset and a complete block [2]. The classical approach using paresthesia technique is a blind technique and is associated with a higher failure rate and injury to the nerves, vessels and surrounding structures [3]. For addressing some of these issues, the use of Peripheral Nerve Stimulator (PNS), which allowed better localization of the nerve/ plexus, was started [4-5]. The success rate of block is increased when local anaesthetic is injected at the site of stimulator that evoked finger flexion response [6]. However, this technique is still a blind procedure and has the risk of injury to vessels, surrounding structures, nerves and pleura leading to pneumothorax [7].
Introduction of Ultra Sound (US) has revolutionized the domain of regional anaesthesia as the US procedures are no longer blind and a calculated amount of the drug can be administered at the exact location of nerves/ plexus under real-time observation [7]. In the present studies, we have compared the efficacy of US guided technique with PNS for supraclavicular brachial plexus block in upper limb surgeries.
According to the study done by Singh et al [8]. The success rate reported in US group was 90% and that reported in the Nerve stimulator group was 73.1%. The proportional difference between the two groups was 16.9% (round off to 17%). This difference was used for sample size calculation. Sample size calculation revealed that 78 patients per group will be required to detect a proportional difference of 17% between the success rates of supraclavicular block of two groups, at an alpha of 0.05 with power of 80%. The p values < 0.05 were considered to indicate statistical significance. Hence, we intended to take more than 78 patients per group.
American Society of Anaesthesiologists (ASA) grade I, grade II patients of both genders of age between 18 and 50 years were subjected to the present studies after obtaining their written consent. A customized proforma was used for collecting the data for the present study along with observational method for any additional finding. Patients having allergy to local anaesthetics drugs, coagulopathy, infection at injection site, severe pulmonary pathology, Body Mass Index (BMI) more than 35 kg/m2, pre-existing neuropathy in operative limb, pregnant patients, emergency surgery, cases of failed blocks during study and not willing to provide their voluntary written consent for participation in the study were excluded.
The patients were randomized into two groups of eighty numbers each for group US and group PNS using computer generator numbers.9 The group US patients received the supraclavicular brachial plexus nerve block under the ultrasound guidance and the group PNS patients received the supraclavicular brachial plexus nerve block using peripheral nerve stimulator. All blocks using Ultra Sound (US) guidance and Peripheral Nerve Stimulator (PNS) were performed by the experienced anaesthetist. The details of the study including procedure, risks/ benefits, advantages/ disadvantages of one method over the other were explained to the prospective patient and/ or his/ her legally acceptable representative.
A customized proforma was used for collecting the data for the present study along with observational method for any additional finding. The data was then transferred to Microsoft Excel for analysis and thereafter online statistical software was used for calculating the p-value. Comparison of mean between the two techniques was done using unpaired t-test, within the technique was done using paired t-test. Proportional comparison was done using Z-test for two sample proportions and association of non-parametric data was done using Pearson Chi-square test. A p-value less than 0.05 was considered as statistically significant.
The protocol was submitted before the ethical committee for approval. After due approval from the Ethics Committee, the study was initiated. Preoperative clinical assessment was done for each patient. All the patients were evaluated for any systemic diseases and necessary laboratory investigations were recorded. Patients were advised overnight fasting. If a patient was taking any anti-hypertensive medication or thyroid medication, he/ she was made to take morning dose with sips of water.
In the operation theatre, patients were monitored with pulse oximetry, non-invasive blood pressure, and electrocardiogram. After establishing an intravenous access, the patients received inj. midazolam 1 mg intravenously. No other sedation was given till evaluation of the block was completed. The respective equipment was kept ready and the drugs were loaded maintaining sterility. The drug used was 0.5% bupivacaine. The fixed amount of local anaesthetic injected was 20 ml 0.5% bupivacaine + 10 ml normal saline. The maximum permissible dose of bupivacaine was calculated according to the body weight so as to ensure that it did not exceed the toxic dose (inj. bupivacaine 2 mg/ kg). Mean weight in the present study of all subject was 65 kg and 63 kg for PNS group and USG group respectively. So, the administered dose did not exceed the toxicity limit in all the patients of the two groups. The patient was positioned supine with the arms by the side and head turned to the opposite side. The proposed site of block was aseptically prepared with 10% betadine solution and draped.
Group US
A Sonosite Micro Maxx probe (6-13 MHz) was used for conducting the block in every case. The linear probe was inserted into a sterile plastic sheath so as to maintain sterility. The image of subclavian artery in short axis (cross-sectional view) was obtained. The nerve bundles of brachial plexus appear in groups as 3-4 hypo-echoic (dark) circles anterior and lateral to the subclavian artery. A scan prior to needle insertion help in exact nerve location, and is thus helpful in defining the desired site, angle and path of needle penetration. A 22 G insulated Teflon coated needle (Stimuplex D 50 mm, B. Braun, Germany) was used. Skin was anesthetized at the site of entry with 1% Lignocaine (1-2 mL) and a 22 G, 50 mm needle was connected to a 10 cm extension line and primed with the drug. It was inserted in plane and the needle movement was observed in real time. Once the needle reached the plexus after negative aspiration of blood, drug was injected using single injection technique and thereafter the spread of the drug was observed. The amount of local anaesthetic injected was 20 ml 0.5% bupivacaine + 10 ml normal saline. Initially 10 ml of prepared solution was injected in a graded manner. After visually and confirming the spread of the drug around the nerve bundle with US, remaining 20 ml of the drug was injected. The onset of sensory and motor block of radial, ulnar and median nerves was recorded after intervals of 5 min for 30 min.
Group PNS
A B. Braun Peripheral Nerve Stimulator (PNS) was used for conducting the block in every case. In this group, the positive electrode of the PNS was attached to an ECG lead and was placed on the ipsilateral arm. The subclavian artery pulsation was palpated to avoid a puncture and the inter-scalene groove was palpated to trace the path of the plexus for needle insertion. The block was administered using PNS specific, sterile, Teflon-isolated needles (22 G insulated needle Stimuplex® D 50 mm B. Braun Germany) and the needle was flushed with drug. The PNS was set with pulse duration of 0.15 ms, a current intensity of 1 mA, and a frequency of 2 Hz. Once wrist or hand motion got elicited, the stimulating intensity was reduced to less than 0.4 mA maintaining good twitch. A volume of 30 ml (20 ml of 0.5% bupivacaine + 10ml normal saline) solution was injected after negative aspiration of blood. The onset of the brachial plexus block was recorded in a similar fashion as for Group US. Evaluation of sensory and motor block was performed every 5 min in all nerve territories over a period of 30 minutes.
Block execution time is calculated from the time of initial scanning to the removal of the needle in case of the group US. For the group PNS, it is the time from the time of insertion of the needle to its removal. The onset of sensory block is assessed by pin prick and cold application every 5 min. It was the time from the removal of block needle to the time when the patient first says that he/ she had reduced sensation when compared to the opposite limb. The time of onset of motor block was assessed every 5 min. It was the time from removal of the block needle to the time when the patient had weakness of any of the three joints − Shoulder, elbow, or wrist, upon trying to perform active movements.
In order to avoid the possibility of any bias, the block onset and success were assessed by an independent person who was not involved in the performance of the block. The quality of sensory block was assessed every 5 min after the onset was established. It was assessed using pin prick and application of ice-cold water. At the end of 30 minutes, the quality of sensory block was assessed by the number of dermatomes having a full block. The sensory block in each dermatome was graded as (a) blocked - complete absence of sensation, (b) patchy - reduced sensation when compared to the opposite limb (c) no block - normal sensation. The quality of motor block was assessed every 5 min after the onset was established. It was assessed by asking the patient to perform active movements of each of the three joints − Shoulder, elbow, and wrist. The motor bock at each joint was graded as (i) blocked - no power (ii) patchy - able to move actively (c) no block - full power. A block was graded as (i) grade 1 - excellent (no complaint from patient) (ii) grade 2 - good (minor complaint with no need for the supplemental analgesics) (iii) grade 3 - poor (complaint that required supplemental analgesics).
Postoperatively, pain was assessed using Visual Analogue Scale (VAS). Patients were supplemented with analgesics when they complained of pain or with a VAS score of more than 4, and the duration of analgesia was noted.
In the present studies, observations were made regarding patient profile, block execution time, onset of sensory and motor block, and duration of sensory and motor block, duration of analgesia time in both the groups; US and PNS. As shown in the Table 1, the characteristics such as Body Mass Index (BMI), age, weight and height of the patients in both the groups have p values more than 0.05 making them non-significant. The Block Execution (BE) time within the same group was also found to be non-significant for both the groups as shown in Table 2. Figures 1 and 2 show the BE time within the groups and between the groups respectively. Table 3 compares the results on duration of surgery, BE time, onset of sensory and motor block, duration of sensory and motor block and duration of anaesthesia for the group US and Group PNS. A comparison of complications of block has been made for the group US and group PNS and has been shown in Table 4. The quality of block for the group US and group PNS is summarized in Table 5.
| Patient Profile | Group US | Group PNS | p value | Remarks | ||
|---|---|---|---|---|---|---|
| Mean | Standard deviation (SD) | Mean | Standard deviation (SD) | |||
| Body Mass Index (BMI) | 24.16 | 3.482 | 24.866 | 3.088 | 0.180 | Not Significant |
| Age | 33.28 | 8.022 | 33.32 | 7.737 | 0.968 | Not Significant |
| Weight | 63.94 | 9.212 | 65.64 | 8.126 | 0.218 | Not Significant |
| Height | 162.78 | 6.747 | 162.91 | 6.51 | 0.896 | Not Significant |
Table 1: Group statistics (Unpaired t-test).
| Block execution time (within group) | n | Mean | Standard deviation | T | p value | Remarks | |
|---|---|---|---|---|---|---|---|
| Group PNS |
1-40 | 40 | 11.88 | 1.856 | -0.187 | 0.853 | Not Significant |
| 41-80 | 40 | 11.95 | 1.739 | ||||
| Group US |
1-40 | 40 | 9.15 | 1.762 | 1.415 | 0.161 | Not Significant |
| 41-80 | 40 | 8.68 | 1.185 | ||||
Table 2: Comparison of Block Execution (BE time) within groups (Unpaired t-test).
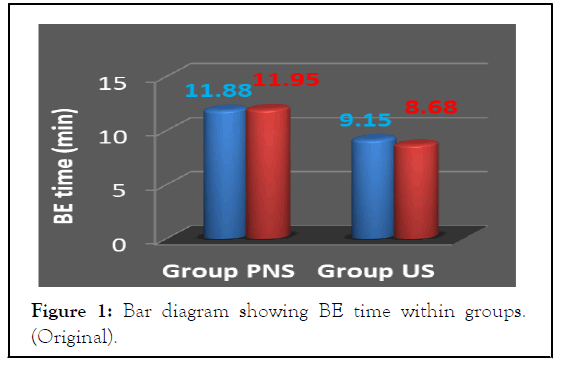
Figure 1: Bar diagram showing BE time within groups. (Original).
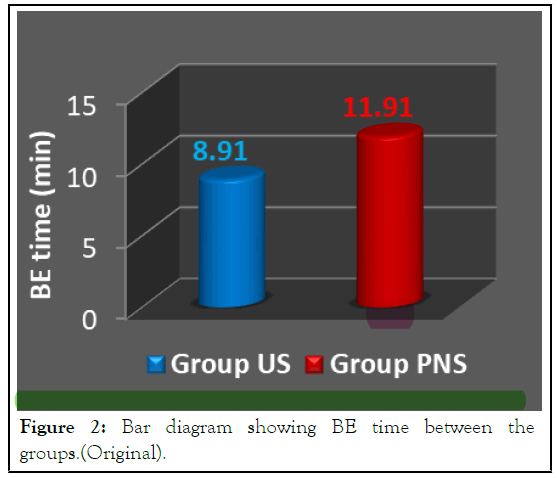
Figure 2: Bar diagram showing BE time between the groups.(Original).
| Parameter | Group | n | Mean | SD | p value |
|---|---|---|---|---|---|
| Duration of Surgery (min) | US | 80 | 69.31 | 19.287 | 0.693 |
| PNS | 80 | 70.56 | 20.654 | ||
| Block Execution time (min) | US | 80 | 8.91 | 1.511 | 0.000* |
| PNS | 80 | 11.91 | 1.787 | ||
| Onset of Sensory block (min) | US | 80 | 12.41 | 2.085 | 0.000* |
| PNS | 80 | 14.56 | 2.261 | ||
| Duration of Sensory block (min) | US | 80 | 404.94 | 74.509 | 0.000* |
| PNS | 80 | 290.81 | 28.523 | ||
| Onset of Motor block (min) | US | 80 | 15.55 | 2.08 | 0.000* |
| PNS | 80 | 19.94 | 3.403 | ||
| Duration of Motor block (min) | US | 80 | 284.81 | 57.498 | 0.000* |
| PNS | 80 | 222 | 30.694 | ||
| Duration of Analgesia (min) | US | 80 | 414.38 | 73.227 | 0.000* |
| PNS | 80 | 298.31 | 28.261 |
*Statistically significant Value.
Table 3: Comparison of duration of surgery, block execution time, onset of sensory and motor block, duration of sensory and motor block, duration of analgesia time in the groups (unpaired t-test).
| Group | Complications | Total | p value | Remarks | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Group US | 80 (100%) | 0 (0%) | 80 100%) | 0.497 | Not significant |
| Group PNS | 78 (97.5%) | 2 (2.5%) (Vessel puncture) |
80 (100%) | ||
Table 4: Comparison of complication of Block (Fisher’s Exact Test).
| Group | Grade of block | p value | Remarks | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| Group US | 79(98.8%) | 1(1.2%) | 0 | 0.005 | Significant |
| Group PNS | 69(86.2%) | 11(13.8%) | 0 | ||
Table 5: Comparison of Grade of Block (Fisher's Exact Test).
In the present study, supraclavicular brachial plexus block was performed by using Ultra Sound (US) guidance and Peripheral Nerve Stimulator (PNS) techniques in the two groups consisting of eighty patients each. The two groups group US and group PNS, were comparable with respect to age, weight, height and BMI. As can be seen from Table 1 there was no statistically significant difference in the demographic profiles of the patients in the two groups (p > 0.05). All the patients had successful brachial plexus block and satisfactory surgical anaesthesia.
The block execution time in the first forty and remaining forty patients of group US and similarly in the first forty and remaining forty patients of group PNS, was calculated and compared within the groups. The results were found to be statistically not significant (p > 0.05). The block execution time between the two groups was also compared. As is shown in Table 3, the mean execution time was 8.91 ± 1.51 min for group US and 11.91 ± 1.78 min for group PNS.This difference was found to be statistically significant (p < 0.05). Similar results were reported in the literature [10-13].
It can be inferred from the present study that the block execution time was shorter in group US than that in group PNS. This may be attributed to real-time visualization of the plexus and precise ultrasound guidance of the needle avoiding the blood vessels and pleura.
The mean onset time of sensory block in group US was 12.41 ± 2.085 min and 14.56 ± 2.261 min in group PNS. The difference was found to be statistically significant (p < 0.05). The mean onset time of motor block in group USG was 15.55 ± 2.08 min and 19.94 ± 3.40 min in group PNS. The difference was found to be statistically significant (p < 0.05). Thus, the onset of sensory and motor block was found to occur earlier in group US than that in group PNS. The earlier onset of sensory and motor block in group US may be attributed to precise deposition of the drug around the plexus/ nerve. There are similar reports available in the literature however with different drug / combinations of drugs [12-14].
As can be seen from Table 3, the mean duration of sensory block was observed to be 404.94 ± 74.509 min in group US and 290.81 ± 28.52 min in group PNS. This difference in duration of sensory block was statistically significant (p < 0.05). The mean duration of motor block in group US, was found to be 284.81 ± 57.49 min and in group PNS, it was 222.00 ± 30.694 min. This difference in duration of motor was statistically significant (p < 0.05). It is evident from the above that the duration of sensory and motor block was longer in group US than that in group PNS. Similar results were reported in the literature [12].
From the present study it can be inferred that longer durations of sensory and motor blocks in group US may be attributed to precise deposition of drug around the plexus leading to prolonged duration of analgesia [15].
In the present study the mean duration of analgesia was 414.38 ± 73.22 min in Group US and 298.31 ± 28.26 min in group PNS (Table 3). The difference in duration of analgesia in the two groups was found to be statistically significant (p < 0.05). The longer duration of analgesia in group US was the result of precise administering of the drug around the plexus.
In group US, 98.8% (79 out of 80) patients experienced no pain whereas only 1.2% (1 out of 80) patients experienced minor pain requiring no analgesic supplementation. In group PNS 86.2% (69 out of 80) patients experienced no pain whereas only 13.8% (11 out of 80) patient experienced minor pain requiring no analgesic supplementation. From the foregoing description it can be inferred that the deposition of drug with precision around the plexus improved the grade of block in group US.
Fisher's Exact Test was applied to compare complications between US and PNS groups. There were two venous punctures in group PNS, but this was found to be statistically not significant. For the group US, as the block were performed under real time visualization, there was no incidence of vascular puncture or any other complications. Thus, it can be inferred from the present study that in group US, all complication like vessel puncture and pneumothorax can be avoided by direct visualization of sensitive anatomy of vessel and pleura.
All the patients recruited under both the groups had successful block and had undergone the respective surgery successfully.
A comparison between Ultra Sound (US) versus Peripheral Nerve Stimulator (PNS) guided supraclavicular brachial plexus block in upper limb surgery revealed the superiority of the former technique. Ultra Sound (US) guided supraclavicular brachial plexus block for patients undergoing upper limb surgeries ensured rapid onset of sensory and motor blockade and longer duration of analgesia as compared to group PNS. The time required to perform the block was shorter for group US as compared to group PNS. Only two (out of 80) cases of vascular puncture occurred in group PNS whereas there was no complication in group US.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Sharma A (2022) Superior Ultrasound Guided Technique for an Effective Supraclavicular Block in Upper Limb Surgery. J Anesth Clin Res. 13:1075.
Received: 20-Apr-2020, Manuscript No. JACR-20-001-PreQc-22; Editor assigned: 27-Apr-2020, Pre QC No. JACR-20-001-PreQc-22 (PQ); Reviewed: 25-May-2020, QC No. JACR-20-001-PreQc-22; Revised: 02-Jun-2022, Manuscript No. JACR-20-001-PreQc-22 (R); Published: 01-Aug-2022 , DOI: 10.35248/2155-6148.22.13.1071
Copyright: © 2022 Sharma A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.