Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Review Article - (2020)
Introduction: Keratosis Pilaris (KP) is a harmless condition of the skin.it is may be a secret on your skin for a few times. There are several types of keratosis pilaris and it has been associated with pregnancy, type 1 diabetes mellitus, obesity, dry skin, allergic diseases (e.g., Atopic dermatitis) and rarely cancer.
Often the lesions can appear on the face, which may be mistaken for acne.
Aim: The aim of this review was to present this condition of the skin and increase information about keratosis pilaris.
Methods: A detailed electronic search was carried out on the authentic databases. Review authentic data on websites/ following patients comments for correct realization their belief form keratosis pilaris and study journals about this common skin condition.
Results: In most cases, the condition gradually improves before age 30. However, it can persist longer. Physician can often diagnose keratosis pilaris simply by examining the skin; tests are not needed.
Physicians will often consider family history and the presence of symptoms when making the diagnosis.
Conclusion: This review suggests that
• Use the soaps with suitable pH
• Limit your time in the water
• Avoid tight clothes
You should follow the suggestions above and be patient.
Keratosis pilaris; Chicken skin; Hard bumps; Sandpaper; Follicular keratosis
Keratosis Pilaris (KP) (also follicular keratosis, lichen pilaris or colloquially ″chicken skin″ [1-3]) is a common skin condition. It causes small, hard bums that may make your skin feel like sandpaper [4,5]. It most often appears on the outer side of the upper arms, (the forearms can also be affected), thighs, face, back and buttocks [6]. KP can also occur on the hands and tops of legs, sides or any body part except glabrous (hairless) skin (like the palms or soles of feet) [7].
There are several subtypes of KP:
• Keratosis pilaris alba: Grayish with papules without surrounding redness.
• Keratosis pilaris rubra: Marked redness surrounding an area of KP.
• Keratosis pilaris rubra faciei: KP located on the face.
• Keratosis pilaris atrophicans: A set of related disorders described be KP followed by atrophy (thinning and depression of the upper layers of skin with wrinkling). This type can cause scarring.
• Keratosis pilaris atrophicans faciei: Also known as ulerythema ophryogenes.
This is a very uncommon form of KP atrophicans located on the face especially the cheeks. This type can cause scarring and hair loss in the area [8].
Keratosis pilaris occurs when the human body produces excess amounts of the skin protein keratin resulting in the formation of small, raised bumps in the skin often with surrounding redness [9]. The bumps in the skin can occasionally be itchy [9].
Though people with keratosis pilaris experience the condition year-round, the problem can become exacerbated and the bumps are likely to look and feel more pronounced in color and texture during the color months when moisture levels in the air are lower [10]. The symptoms may also worsen during pregnancy or after childbirth [3]. Keratosis pilaris is the most common disorder of the hair follicle in children [1]. Like acne, keratosis pilaris is a lot more common around puberty with half or more of all teen affected. Often, it goes away as a person grows older. It also tends to come and go, for example, someone might notice it more in winter that in summer [11]. Keratosis pilaris or lichen skin is an autosomal dominant genetic condition of the skin [6].
All study types were considered eligible. This review focuses primarily on introduction of KP. All articles deemed clearly relevant were examined in full text.to be included, studies had to include of relevant term about keratosis pilaris or even natural ways for elimination keratosis pilaris. Reading and analyze the patients' comments on the websites. Although keratosis pilaris is a harmless condition of the skin, but it had a high influence on the patients' life. For more perception, this research subject and their suffering from this condition, it was necessary to spend time on this work. one of used way in this article was encourage to have happy life with KP.
Keratosis pilaris on the world
Although keratosis pilaris may manifest in persons of any age, it usually appears within the first decade of life and is more common in young children [12]. Worldwide, KP affects an estimated 30%- 50% of the adult population and approximately 50%-80% of all adolescents. It is more common in woman than in men and is often present in otherwise healthy individuals [13]. Both sexes are affected by keratosis pilaris but female may be affected more frequently than males (Figures 1 and 2) [14].
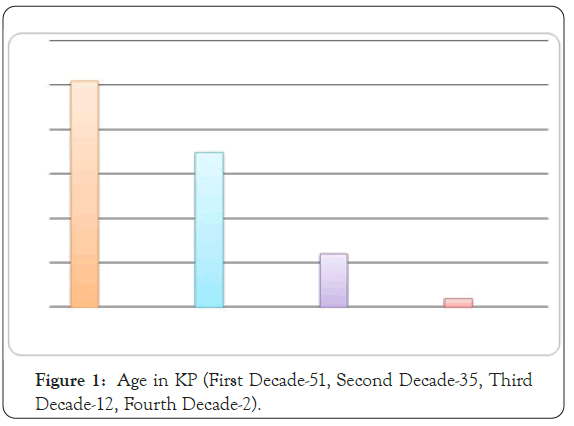
Figure 1: Age in KP (First Decade-51, Second Decade-35, Third Decade-12, Fourth Decade-2).
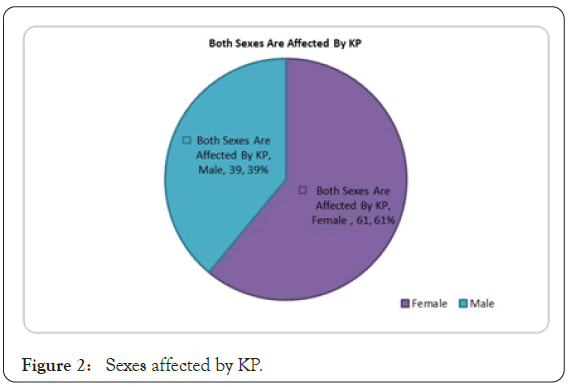
Figure 2: Sexes affected by KP.
How do you diagnose keratosis pilaris?
The most prominent symptom of keratosis pilaris is small, dry bumps that can feel a bit like sandpaper or goosebumps. The Bumps are usually white, but sometimes they appear red or a reddish-pink color may develop around the bumps. The number of bumps in one location varies, as a person can develop 10, 50 even 100 small bumps in one area (Figure 3) [15].
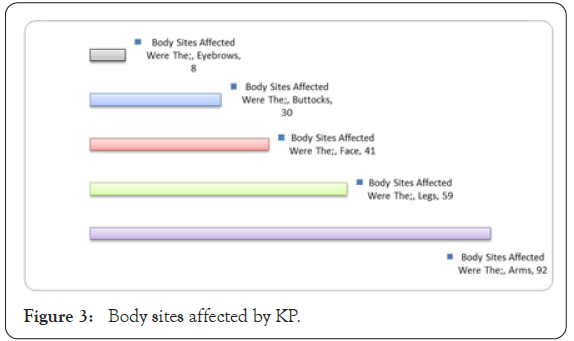
Figure 3: Body sites affected by KP.
Family history
Physicians will often consider family history and the presence of symptoms when making the diagnosis. Research suggests that keratosis pilaris is genetic and it may be associated with genetic skin conditions, like atopic dermatitis, a type of eczema. In a 2015 study involving 50 patients, 67 percent of them had a family history of keratosis pilaris (Figure 4) [4].
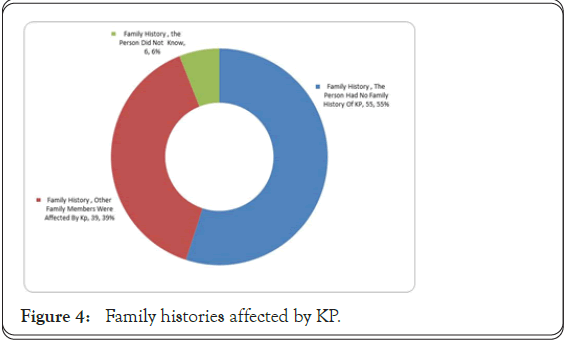
Figure 4: Family histories affected by KP.
Weather
Seasonal variation is sometimes described with improvement of symptoms in summer months. Dry skin in winter tends to worsen symptoms for some group of patients. Overall, keratosis pilaris is self-limited and again, tends to improve with age in many patients. Some patients have lifelong keratosis pilaris with periods of remission and exacerbations. More widespread atypical cases may be cosmetically disfiguring and psychologically distressing [16]. A seasonal variation in the severity of KP was noted in 80% of patients (Figure 5).
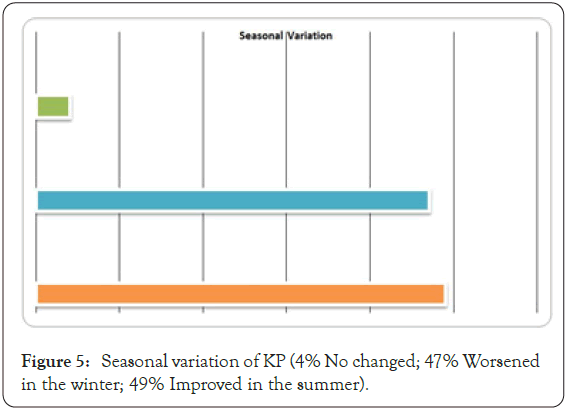
Figure 5: Seasonal variation of KP (4% No changed; 47% Worsened in the winter; 49% Improved in the summer).
Diet
Dietary manipulations such as gluten-free or dairy-free anti- inflammatory, sugar-free, paleo or various autoimmune diet protocols are often implemented. A variety of ″gut healing″ regimens are also prescribed, but as with most therapies surrounding keratosis pilaris, there is no evidence to support or refute them. If you have celiac disease or gluten sensitivity you theoretically might suffer from keratosis pilaris flare-up if you are consuming gluten and have ongoing inflammation or malabsorption. There is no study including a direct correlation between gluten ingestion and keratosis pilaris [17].
Skin care
Keratosis pilaris has no effect on health.it doesn`t hurt and usually doesn’t itch. Some natural ways for treatment of keratosis pilaris:
Baking soda: Baking soda is not just for baking your cookies. It also has excellent exfoliating properties for your skin, removing dead cell and opening pores. Mix 2-3 tablepoons of baking soda and water to form a paste, gently scrub the affected area for 3-5 minutes and rinse.
Sour cream: Leftover sour cream from taco tuesday? Use it to help treat your KP! The lactic acid naturally found in sour cream helps to remove keratin buildup that can irritate your skin. Alone or with a little white or brown sugar, gently rub in a circular motion for a few minutes and then rinse. You can also use other ingredients from your fridge that contain lactic acid, such as yogurt or buttermilk [18].
Contagious: Keratosis pilaris is not contagious. People do not give it to someone else through skin contact and do not catch it from anyone else.
Some people are simply more prone to developing keratosis pilaris because of genetics and skin type.
Laser treatment
Laser Hair Removal (LHR) has been used in keratosis pilaris to decrease hair growth in affected areas.
Some cases of keratosis pilaris have been successfully treated with laser therapy, which involves passing intense bursts of light into targeted areas of the skin. Theoretically, LHR may help decrease the portion of bumps in keratosis pilaris caused by small, coiled, ingrown hair. There is no study showing a cure of keratosis pilaris with LHR.
Does keratosis pilaris improve with age?
This common skin condition isn’t harmful but it has influence on social life. For some people, the bumps go away on their own or become less noticeable by about age 30. The mean age of improvement was 16 years (Figure 6).
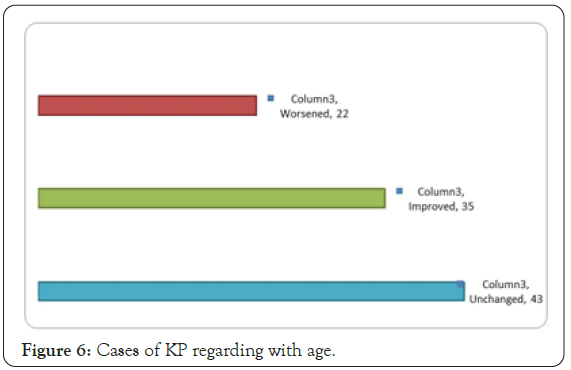
Figure 6: Cases of KP regarding with age.
Time to compare
Two harmless condition characterized by tiny bumps: Many people often confuse keratosis pilaris and milia, two conditions which are characterized by small hardened bumps on the skin. Fortunately, KP bumps are seldom painful, itchy or detrimental to one`s health.
Keratosis pilaris bumps form when fine flakes of dead skin cell clog one`s hair follicles, creating a rough ″plug″. Milia are small dome- shaped bumps or cysts that often appear in clusters and which occur as a result of dead skin becoming trapped in pockets on the skin`s surface. Yellow or white in color, they are seldom itchy or painful to the touch, although they may be easily irritated rough clothing and sheet. Teenagers tend to develop keratosis pilaris on their upper arms, whereas babies tend to have keratosis pilaris on their cheeks.
Milia can appear in people of any age or gender. However, it is most commonly seen in newborn children. It tend to appear on the cheeks, eyelids and face in small clusters in children, whereas adults often see milia appear on their faces and on parts of the body which are swollen, inflamed, irritated or injured. Newborns are seldom treated for milia, as the condition typically resolves itself after a few weeks. It is important that you don`t scratch, pinch or scrub milia in children, as this may lead to further irritation or an infection.
Milia, in order, children and adults will typically resolve itself independently as well. However, in the cases that your milia are painful or will not disappear, there are several treatment options available. Laser ablation and diathermy are both used to destroy milia cysts, whereas topical retinoid and chemical peels are also commonly employed to remove milia. However, the most common means of eliminating milia cysts in via cryotherapy, or freezing the cysts. Although keratosis pilaris and milia are both characterized by small, hardened bumps, both conditions are generally harmless to sufferers.
Keratosis pilaris and a common skin condition (Ichthyosis vulgaris): Ichthyosis vulgaris (also known as ″autosomal dominant ichthyosis″ and ″ichthyosis simplex″) is a skin disorder causing dry, scaly skin. The condition gets its name from the Greek word for fish, because the skim look like fish scales. It is the most common form of ichthyosis affecting around 1 in 250 people. For this reason, it is known as common ichthyosis.
The symptoms of the inherited form of ichthyosis vulgaris are not usually present at birth but generally develop between 3 month and 5 years of age. The symptoms will often improve with age, although they may grow more severe again in old age. Ichthyosis vulgaris is a skin condition resulting in scaly skin, especially on the arms and legs.
Ichthyosis vulgaris can be a trait passed on in families (hereditary) or it may develop later in life as a result of certain exposures (acquired). The hereditary type, also called congenital ichthyosis vulgaris, first appears in early childhood and accounts for more than 95% of cases of ichthyosis vulgaris. The acquired type usually develops in adulthood and results from an internal disease or the use of certain medications. Hereditary ichthyosis vulgaris is fairly common. The most common locations for ichthyosis vulgaris include fronts (extensor surfaces) of the legs, scalp back (extensor surfaces) of the arms, back, forehead and cheeks, especially in younger children, the scales of ichthyosis vulgaris range in size from 1-10 mm and in color from white to gray to brown, with darker-skinned people often having darker scales, the legs are usually affected more than the arms.
Over 50% of people with ichthyosis vulgaris have some type of atopic disease such as allergies, eczema or asthma. Another common condition associated with ichthyosis vulgaris is keratosis pilaris. Hereditary ichthyosis and acquired ichthyosis look similar and both are usually itchy. However the acquired form occurs in people with many internal condition, including poor nutrition, infections such as leprosy or HIV/AIDS, glandular diseases, such as thyroid or parathyroid problems, sarcoidosis, cancer such as lymphoma or multiple myeloma, Use of certain medications, such as nicotinic acid, cimetidine and clofazimine. Hereditary ichthyosis vulgaris tends to improve after puberty, while acquired ichthyosis vulgaris requires treatment of the medical condition before it will improve.
This compare was design for your information and a simple point. All the condition skin that was in this compare is common. There is another common skin condition likeness of keratosis pilaris .they influences on your life, but amount this influence it depend on yourself. Never give up.
The review suggest be kind with your skin. You are always perfect, KP can`t hurt you. In addition, KP is medically harmless. You can have a good life with high quality even with KP. You shouldn`t be embarrassed about your skin. Don’t hide your KP, be relaxed and explain to your family, friend and your partner smoothly about keratosis pilaris. I use a word in full text over and over, yes! ″The common condition″ I said over and over, because I want to eliminate fear of KP. Someone is afraid of KP and embarrass a lot. KP is a common skin condition.
Citation: Shahrosvand S (2020) Study of Secret on your Skin. J Clin Exp Dermatol Res. 11:543.
Received: 26-Oct-2020 Accepted: 09-Nov-2020 Published: 16-Nov-2020 , DOI: 10.35248/2155-9554.11.s7.543
Copyright: © 2020 Shahrosvand S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.