
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Mini Review - (2022)Volume 13, Issue 6
Osteochondromas are benign bone tumors that mainly affect the metaphysis of long bones. We describe a 50-year-old patient who presented with a ventral scapular osteochondroma that limited her shoulder movement and induced paresthesia during sleep. The swelling was accompanied by pain and an inability to execute her professional obligations for the preceding four months. There were no neurological abnormalities. CT scan revealed a mushroomshaped mass with cortical and medullary components near the scapula's lateral angle. We carried out the surgery using the lateral decubitus position, general anesthesia, and the axillary approach.
We describe a unique location and age range in which osteochondroma manifests. Because the risk of malignancy grows with age, we underline that osteochondroma should be considered a differential diagnosis in both unusual locations and age groups. Secondly, patients should be monitored clinically and radio graphically following excision.
Osteochondroma; Scapula; Paresthesia; Trauma
Osteochondromas, which typically affect the metaphysis of long bones, account for more than forty percent of benign bone tumors [1]. Ninety percent of osteochondromas are located on the proximal humerus or in the vicinity of the knee joint. It rarely involves flat bones like the pelvis and scapula [2]. The mass effect, compression of adjoining neurovascular structures, mechanical irritation of overlying muscles and tendons, malignant transformation, fracture, and bursa development are all potential complications of a scapular osteochondroma [3].
Osteochondromas often begin in childhood and are asymptomatic. We report a case of a 50-year-old patient who came with a ventral scapular osteochondroma that restricted shoulder movement and elicited paresthesia. We explained the procedure to the patient and obtained written informed consent to publish the case report and photographs.
A 50-year-old female computer engineer reported to our institution with a swelling on the anterior part of her right shoulder. The swelling was accompanied by diffuse pain around the shoulder and an inability to fulfill her job obligations for the preceding four months. There was no history of trauma, fall, lifting heavy weight or cervical pain. It produced pins and needle sensation from the axilla to the fingers while sleeping and pain during adduction. The patient experienced the inability to sleep in the supine position due to paresthesia.
The pain gradually increased over time and posed a substantial impediment to her daily activities from the past four months. The patient did not have any family history significant for osteochondroma. Fever or weight loss did not accompany this swelling. The anterior aspect of the right axilla exhibited a 3.5 cm × 3.5 centimeters smooth, tender, immobile, non-compressible firm swelling located around eight centimeters from the tip of the acromion during the clinical examination and the cartilaginous cap shown in Figure 1. There was no sign of the central punctum, redness, scar, sinus, or fistula.
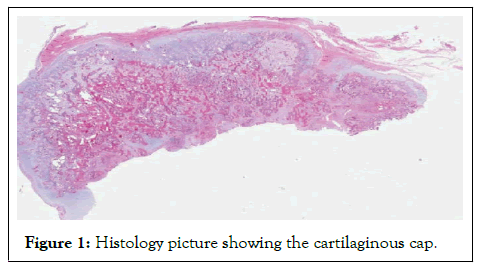
Figure 1: Histology picture showing the cartilaginous cap.
The right shoulder was lower than the left shoulder. The right shoulder displayed a 15-degree restriction in external rotation compared to the left, and adduction was normal but uncomfortable. The Empty can, Hawkin, Bear-hug, and Yergason tests were negative, indicating no rotator cuff involvement. There were no neurological abnormalities [4].
Diagnosis
The right shoulder X-ray suggested a mass protruding from the ventral scapula with a normal shoulder joint, consistent with osteochondroma. CT scan confirmed the presence of a mushroom-shaped mass with cortical and medullary components near the lateral angle of the scapula (Figure 2).
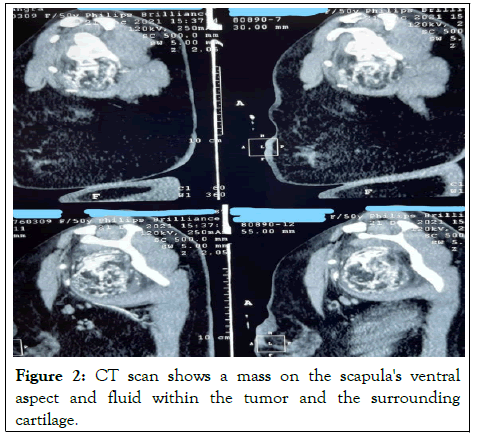
Figure 2: CT scan shows a mass on the scapula's ventral aspect and fluid within the tumor and the surrounding cartilage.
We planned to conduct the surgery under general anesthesia and in the lateral decubitus position.
Surgical technique
We chose the axillary approach due to the tumor's position, despite the proximity to underlying neurovascular structures. The right upper limb was abducted, flexed, and externally rotated. An incision was made over the axilla anterior to the posterior axillary folds. The plane was established between the conjoined latissmus dorsi and teres major tendons and the subscapularis muscle.
The axillary neurovascular bundle was meticulously dissected and retracted superiorly. An encapsulated bony mass, along with the flat base and thick periosteum, was removed from the anterior surface near the lateral angle of the scapula. After resection, a tennis ball-sized skeletal mass measuring roughly 7.5 cm by 5 cm was obtained, with flecks of cartilage surrounding its base. We took special precautions to protect the pleura throughout the surgery, and a postoperative chest scan revealed bilateral fully enlarged lungs. We diagnosed the tumor as osteochondroma. Histology corroborated the diagnosis, showing a hyaline cartilage cap resembling an unstructured growth plate encircled by perichondrium.
The patient's range of motion improved considerably following surgery, and her pain and paresthesia also subsided. After ten days, we performed the suture removal, and the subsequent follow-up was uneventful.
Osteochondroma can occur in any bone that undergoes endochondral ossification. The majority of osteochondromas is asymptomatic and is diagnosed in the first or second decade of life [2]. Our patient, on the other hand, appeared in her sixth decade of life with discomfort and paresthesia in her right upper limb. Because of physeal centers at medial and lateral angles, the osteochondroma is more prevalent at these angles in the scapula [5]. Osteochondromas can manifest as a solitary tumor or as part of a constellation of inherited exostoses.
Hereditary Multiple Exostosis (HME) can affect all human body's bones except the skull. It occurs due to the inactivation of the EXT gene located on chromosomes [2]. HME has a higher risk of malignant transformation. The patient's age, genders, the location of the tumor on the scapula, and radiological characteristics have been attributed to the malignant transformation of osteochondroma.
Following features on imaging suggest malignant transformation:
1. Growth of a previously unchanged osteochondroma in a skeletally mature patient
2. Irregular margins
3. Focal regions of radiolucency in the interior of the lesion
4. Erosion or the adjacent bone
5. A significant soft-tissue mass, mainly containing scattered or rare cells.
Fractures may arise due to external trauma but heal by sclerosis. Osteochondroma-related vascular concerns include artery displacement, stenosis, occlusion, thrombosis, and pseudoaneurysm formation. It is possible to diagnose these complications with Doppler ultrasound CT/MRI angiography. Neurologic complications have been reported with both peripheral and central osteochondromas. MRI is the modality of choice to rule out any neurological involvement Osteomyelitis, muscular impingement, and hemarthrosis are some uncommon sequelae of osteochondroma. Scapular osteochondromas can produce snapping scapula syndrome due to skeletal anomalies, pseudo winging due to one end of the scapula being more prominent, and bursa formation above the tumor [1]. Microscopically, the cartilage cap fuses with the underlying bone. The capsule encases the tumor analogous to the perichondrium. The cartilage serves as a growth plate, with chondrocytes contributing to the tumor's growth and maturation identical to that of endochondral ossification. Mechanical stress and trauma act as stimulators of chondrocyte proliferation. These chondrocytes in osteochondroma are similar to the normal cartilage generating cells. Osteochondroma is treated by surgically removing the tumor. Clinical examinations and radiography should be carried out on patients following the excision. Any onset of new symptoms, increase in pain, neurological features, and recurrence of swelling may indicate malignant transformation.
The case demonstrates the importance of maintaining osteochondromas as a differential diagnosis because atypical presentation can arise late in life. With increasing age, the likelihood of the tumor being malignant increases exponentially. Thus, with a careful clinical examination and imaging, scapula cancers can be accurately detected and treated surgically with excellent outcomes.
We did not receive any specific support from funding agencies in the public, commercial, or not-for-profit entities.
We described the technique to the patient in her native language and obtained her approval to submit the article and accompanying photographs for publication.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Makkar D, Sauhta R (2022) Scapular Osteochondroma; A Unique Site in a Fifty Year Old: An Unusual Case. J Anesth Clin Res. 13:1068.
Received: 02-Jun-2022, Manuscript No. JACR-22-18455; Editor assigned: 06-Jun-2022, Pre QC No. JACR-22-18455 (PQ); Reviewed: 22-Jun-2022, QC No. JACR-22-18455; Revised: 28-Jun-2022, Manuscript No. JACR-22-18455 (R); Published: 05-Jul-2022 , DOI: 10.35248/2155-6148.22.13.1068
Copyright: © 2022 Makkar D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.