International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Case Report - (2021)Volume 9, Issue 6
Traumatic Brain Injury (TBI) endocrinopathy have been reported previously in the literature. The pathophysiology of post TBI endocrinopathy remains elusive as many studies reveal the high prevalence of pituitary disruption post TBI. We present a case of a 39 years old male previously healthy who was involved in a road traffic accident which resulted in multiple skull fractures expressed on CT brain resulting in severe traumatic brain injury with an initial Glasgow Coma Scale (GCS) of 6/15 upon presentation in the hospital. He concurrently developed a pituitary dysfunction that lead to multiple endocrinopathies including diabetes insipidus, adrenal insufficiency, secondary hypothyroidism and central hypothermia. Which required hormone replacement therapy and multiple dietary requirements? The case is an example of the significant effect of post traumatic brain injury endocrine dysfunction on the patient's general wellbeing and his rehabilitation process. These findings emphasize the importance of early endocrine intervention and high vigilant care during the rehabilitation course. His rehabilitation program needed a multidisciplinary approach with physiatrists, endocrinologists, physical therapists, occupational therapists, neuropsychologists and dieticians. Functionally the patient reached Functional Independence Measure (FIM) of 6/7 requiring more time in feeding, grooming and dressing both upper and lower bodies. In other activities of daily living the patient needs minimal assistance with a FIM score of 4/7. Further progression of rehabilitation program was limited due to the cognitive impairment and the associated visual impairment from the trauma. We recommend further research to create a standardized endocrine screening protocol to detect the endocrinopathy early.
Endocrinopathies; Brain injury; Hypothyroidism; Rehabilitation; Dysfunction
Traumatic Brain Injury (TBI) is one of the leading causes of morbidity and mortality in the World. TBI could lead to varying degree of psychological, social and physical disabilities [1]. Severity if TBI differs from mild to moderate and severe, in which the clinical presentation can range from slight transient state of confusion in a mild TBI or a coma in severe TBI [2]. Most common causes of TBI are motor vehicle accidents and falls. It is estimated that TBI affect 69 million patients in the world each year [3,4]. Data about the incidence of TBI in Saudi Arabia are scarce.
Endocrinopathy post TBI initially been reported in the literature by Cyran, E in 19185. A systematic review showed pooled prevalence of hypopituitarism is 27.5% after TBI [5,6]. Convenien t anatomical position and the vulnerability of the pituitary gland vasculature are the proposed reasons of pituitary dysfunction [7]. Although the pathophysiology of post TBI endocrinopathy remains elusive as many studies reveal the high prevalence of pituitary disruption post TBI.
Deficiency in growth hormone is the most frequent endocrinopathy in the literature [8]. Concurrent anterior and posterior pituitary had reported by Takala, R·S·K in 2006, a case of young man with severe TBI and extended Intensive Care Unit (ICU) stay. We report the rehabilitation course of a patient with similar panhypopituitarism.
A 39 years old Saudi male medically free was driving a vehicle alone in peripheral area in Saudi Arabia. A camel was crossing the road leading to a direct impact on the vehicle windshield. He was found unresponsive and intubated by the paramedics and managed in a peripheral hospital before transferring him to a tertiary care hospital in Riyadh, Saudi Arabia. Immediate ICU admission with initial Glasgow Coma Scale (GCS) of 6/15. Patient was sedated with fentanyl and requiring high concentration of oxygen. The frontal impact of the accident was evident on the patient bruised face and head.
Computed Tomography (CT) of the brain showed multiple contusional hemorrhages mainly the in the frontal lobes causing mass effect with subarachnoid and intraventricular hemorrhages.
Also the CT showed multiple skull and base of skull fractures associated with subcutaneous edema, the fractures were as the following: Left temporal transverse fracture, Chipped fracture of the left occipital condyle, fracture line over the right temporal squamosal bone with displaced fragment, extensive comminuted fragmented fracture of the right sphenoid, comminuted fragmented fractures of the right zygomatic bone involving the temporal process, arch and zygomatic frontal process, omnidirectional comminuted fracture of the right orbital walls, fracture extension into the right frontal bone, nasal bone comminuted extensive fractures involving the nasal septum with evidence of central defect, right maxillary comminuted fracture involving the anterior wall and posterior as well as the maxillary plate bilaterally, left sided maxillary fracture line over the anterior wall, disruption of the ethmoid ostium with comminuted depressed dislocated fracture of the ethmoid bone and plate, fracture line over the right side of the frontal bone extending to the right orbital displaced roof, bilateral displaced fracture of both pterygoid plates and bilateral styloid fractures (Figure 1).
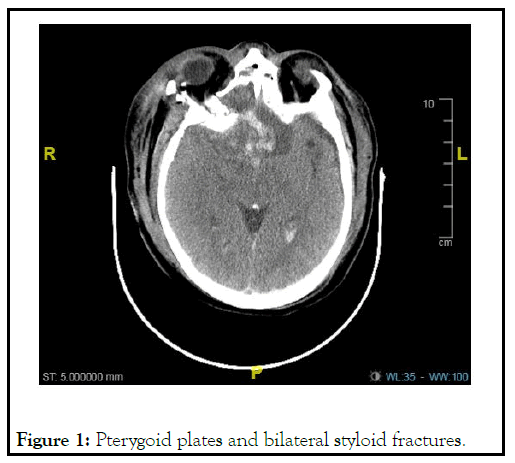
Figure 1: Pterygoid plates and bilateral styloid fractures.
Patient was managed conservatively with no surgical intervention from Neurosurgery team with applying high Intracranial Pressure (ICP) measures.
During the patient 6 months ICU stay, he developed multiple complications. On the first day in the ICU, the patient was tachycardic and requiring more oxygen. High resolution CT of the chest which showed an acute pulmonary embolism. Patient was stable and started on anticoagulation with Inferior Vena Cava (IVC) insertion.
Later in the first two weeks of ICU, the patient’s electrolytes showed hyponatremia with euvolemic status, managed with fluid restriction with the impression of Syndrome of Inappropriate Anti Diuretic Hormone (SIADH) and was managed accordingly. Subsequently the urine output increased with time, measuring more than 4 liters with hypernatremia and associated urine osmolality less than 300 mOsm/kg which led to the diagnosis of Diabetes Insipidus (DI). Desmopressin therapy was started until the patient high urine output subsided with the sodium level correction. Unfortunately his DI continued throughout the rest of his ICU stay and remained as a chronic condition.
Rehabilitation team was involved early in his care with the plan to prevent complications of immobility and intimate early range of motion exercises by Physiotherapy (PT) daily. Finally the patient was transferred to the rehabilitation unit for full cognitive and physical rehabilitation program.
Rehabilitation program
The patient rehabilitation program was challenging since he is the first patient with these multiple endocrinopathies combined with cognitive and visual impairments in our rehabilitation unit. Our initial assessment of the patient is severe traumatic brain injury with cognitively impairment and dependent in all Activity of Daily Living (ADLs). Short term goals of the patient rehabilitation program were to teach his caregivers how to take care of him and asses for any further improvement. Patient was showing improvement day by day even with his severe TBI. Cognitively the patient was still in post-traumatic amnesia. With neuropsychology cognitive therapy sessions we achieved some degree of cognitive function that assessed the patient in ADLs. The visual acuity was hand motion only with no color vision, further more in the rehabilitation program with visual stimulation patient started to recognize colors and simple objects like fruits. Physically, the patient was initially bedbound after his long ICU stays with weak hyportrophied upper and lower limbs bilaterally. With PT patient reached an unexpected stage which was gait training with mild assistance to supervision. Functionally his dependence in ADLs decreased until he reached modified independent in feeding, grooming, and dressing and requires mild assistance in toileting and bathing and other ADLs. Finally he was discharged to his family house and to be taken care of by his family [8-11].
Panhypopituitarism of our patient was evident clinically and in laboratory results. MRI of the pituitary gland was planned to visualize the effect of the trauma, however the caregivers refused the MRI.
Active rehabilitation program demand a patient’s participation in a lengthy one hour sessions of PT and OT which was difficult in our case. Chronic DI of the patient meant that we needed to do daily input/output chart and electrolytes to follow the sodium level. Endocrinology plan was to give desmopressin 1 mcg when the sodium level is at or above 137 mEq/L. Family meeting with the patient and caregiver after discussing the discharge plan which was to do weekly sodium level in primary care clinic and instructed that incase of changes in patient behavior or increase in urine output to go the nearest Emergency Room (ER). Feeding the patient every 4 hours affected the patient sleep hygiene which is a key for neurorecovery. Prednisolone 5 mg daily with the frequent meals managed the adrenal insuffiency.
Asymptomatic hypothermia episodes during the rehabilitation stay was investigated to rule out un underlying cause, however no clear cause for his hypothermia and our impression was central hypothermia and managed with blankets and holding the therapy sessions for the day. Frontal impact of the trauma resulted in bilateral optic nerve injury. His vision improved slightly as we reported and our goal was to teach patient how to use his limited vision in aiding in his short distance ambulation with supervision.
As evident in our patient the disabling effects of his hormonal imbalance on his functional level. Endocrinopathy screening protocol in TBI is not yet established. Previous published studies recommend a hormonal panel at 3 and 12 months after severe TBI.
We recommend further research to develop a standardized endocrine screening protocol to offer the best care for TBI patients and prevent incidental findings of endocrine dysfunction that could have been diagnosed and managed earlier if had been part of the general investigations of the patient.
Citation: Alghaiheb A (2022) R ehabilit ation of a P atient with P anh ypopituit arism P os t T r aumatic Br ain Injur y : A Case R epor t. Int J Ph y s Med Rehabil. 9: 613.
Received: 24-Dec-2021 Accepted: 07-Jan-2022 Published: 14-Jan-2022
Copyright: © 2022 Alghaiheb A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.