Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Case Report - (2021)Volume 12, Issue 7
Localized pericarditis due to ST elevation in local leads might be mimic myocardial infarction and this is a important scenario that need to early evaluation to rule out of myocardial infarction.we describe a patient who presented chest pain and ST elevation after primary PCI that after workup the localized pericarditis was confirmed.
Regional pericarditis; Myocardial infarction; Primary percutaneous intervention
Pericarditis is the most common cause of chest pain following MI, but the frequency of post infarct pericarditis is unclear and ranges from 7 to 41% [1]. Regional pericariditis has been described in several settings, but ocuures most frequently after transmural myocardial infarction [2]. While the diagnosis remains elusive, it must be considered in all patients with recurrent chest pain following acute MI. Pericarditis classically presents with positional chest pain, a pericardial friction rub, diffuse ST segment elevation and PR depression, but regional ECG changes associated with infarction-associated pericarditis sometimes exist. There are no ECG criteria to diagnose regional pericarditis and only a few publications have addressed this condition. While there are no ECG criteria to diagnose infarct is associated regional pericarditis, 2 a typical T wave patterns is the evolution have been described with a sensivity and specifity of 100% and 77%, respectively [3,4]. In contrast to the normal pattern seen during AMI in which there are tall, peaked T wave during the hyperactive phase that become inverted within 48 hours and reamin inverted for days, weeks, or even indefinitely, is post-infarct regional pericarditis is associated with the following 2 atypical T wave patterns: Persistently positive T waves for 48 hour after symptom onset, and 2. Premature and gradual reversal of inverted T waves to persistently upright T waves. In the this paper we aimed to report a case with localized pericarditis that mimic inferior myocardial infarction.
A 53 year old female with known hypertension and diabetes mellitus and diarrhaea from 1 month ago that became worse and with new epigastric pain referred to emergency department from a medical clinic with abnormalities in ECG as ST elevation in inferior leads. The patient had no chest pain complaint. Her ECG was suggestive of an inferior infarct. The patient was taken emergently to catheterization lab. Coronary angiography revealed a complete occlusion of the mid RCA. The patient underwent successful RCA percutaneous coronary intervention. The patient was also treated with antiplatelet therapy. Lab results of the patients are as following: troponin (qualitative rapid method)=positive, WBC=10200/micL, Hb=12.5 g/dL, those are platelet=150000/micL, hematocrit=36.2%, MCV=83.8 fL, fiction BUN=23 mg/dL, creatinine=1.1 mg/dL (Figure 1).
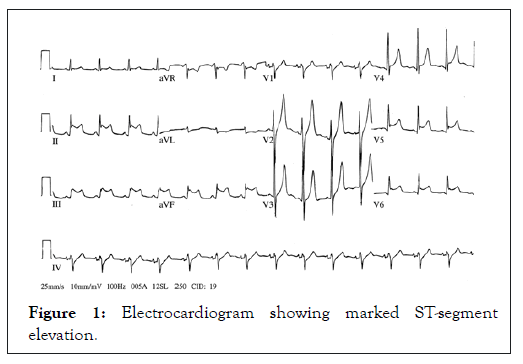
Figure 1: Electrocardiogram showing marked ST-segment elevation.
Within 24 hours of her admission, the patient began experiencing severe chest pain with persistent ST segment elevation in the inferior leads. Repeat coronary angiography was done and had no change from the previous study; and the RCA stent remained patent. But her chest pain remained with no response to treatment. Transthoracic Echocardiography (TTE) in revealed hypokinesis of the inferior and posterior walls, mild left ventricular dysfunction, no pericardial effusion and EF=40%. Its her cardiac enzymes had no reelevation. According to these are to symptoms, ECG changes and TTE findings, angiography friction restudy, a diagnosis of regional pericarditis was made despite the absence of a pericardial rub, which is fleeting in nature and they frequently overlooked. So she received aspirin with antiinflammatory doses and NSAID. In next day’s her chest pain relieved and she became asymptomatic and ECG changes had normalized.
Early assessment of electrocardiographic findings remains the basic evaluation for diagnosis of patients suspected to myocardial infarction [5]. ST elevation has several diferential they diagnosis including myocardial infarction and pericardiatis that myocardial infarction presents with localized STelevation while pericarditis presents with diffuse STelevation [6] in contrast to classic pericarditis that documented with diffuse ST elevation, regional pericarditis appear with focal STelevation and this feature can be difficult to differentiate from myocardial infarction [7]. Post infarction regional pericarditis is the most common cause of regional pericarditis that occurred in our case while in some cases regional pericarditis occurred after cardiac ablation and abdominal surgery [8,9] in similar in our case the diagnosis of pericarditis was difficult because the ECG showed the reciprocal changes in high lateral leads and this finding is more in favor of myocardial infarction the second challenge of diagnosis is that two other criteria for diagnosis of pericarditis including pericardial effusion and friction rub was absent thus the diagnosis was made only based on chest pain and ECG findings of course these two presentation are often not present in acute pericarditis. This should not diminish our doubts about diagnosis of acute pericarditis. To date there is no specific ECG criteria for diagnosis of regional pericarditis and some proposed criteria are not common in clinical setting thus the strong clinical suspicion can be helpful to diagnosis of this problem.
The authors sugesst that it is important to cardiologists to familiar with various pericardial presentations and considered in patients with recurrent or persistent chest pain in the setting of atypical T wave evolution and persistent ST segment elevation. It is also rational to do catheterization to rule out myocardial infarction in these patients.
Citation: Mohamadi A (2021) Regional Pericarditis Mimicking Remyocardial Infarction after Primary Percutaneous Intervention. J ClinExp Cardiolog. 12:689.
Received: 09-Jun-2021 Accepted: 23-Jun-2021 Published: 30-Jun-2021 , DOI: 10.35248/2155-9880.21.12.689
Copyright: © 2021 Mohamadi A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.