Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2023)Volume 12, Issue 9
Objective: The pelvic floor muscles (PFM) are essential for structural support for the pelvic organs. Loss of PFM function can lead to urinary incontinence (UI), a common condition in parous women. This study investigated the efficacy of High-Intensity Focused Electromagnetic (HIFEM) compared to conventional pelvic floor muscle training (PFMT) for the improvement of UI in women.
Methods: Thirty-eight women (27-66 years) underwent six treatments scheduled twice a week for three weeks with either a HIFEM procedure or a standardized pelvic floor exercise. Follow-up visits were performed at 1, 3, 6, 9, and 12 months after the final treatment session. Outcome measures included quality-of-life questionnaires (ICIQ-BD, UDI-6, ICIQ-LUTSqol), pad usage, therapy satisfaction, and therapy comfort.
Results: Analysis of ICIQ-LUTSqol at 6 months showed significant UI improvement in the HIFEM group (-15.2 points, 35%, p=4.4∙10-10) but not in the PFMT group (-5.1 points, 13%, p=1.8∙10-1). The HIFEM group maintained significant improvement over baseline at 12 months (24%, p=3.4∙10-2) while the PFMT group’s score regressed (3%, p=9.3∙10-1). ICIQ-BD demonstrated greater improvement in urgency symptoms in the HIFEM vs. PFMT group (32% vs. 5%) at 12 months. 86% of HIFEM subjects reported less leakage at 12 months compared to 71% of PFMT subjects. Pad usage decreased by -1.7/day in the HIFEM group vs. -1.0/day in the PFMT group.
Conclusion: The HIFEM procedure appears to be safe and effective for improving female continence and quality of life to 1-year.
Electromagnetic Procedure, Incontinence, Leakage, Bladder Diary, Pad Usage
Urinary incontinence (UI) is defined as a complaint of any involuntary and uncontrolled leakage of urine occurring more than twice a month, with the most common forms noted to be stress (SUI; loss of urine on effort, physical exertion, or sneezing or coughing) and urge (UUI; the immediate urge to urinate) [1- 3]. The combination of SUI and UUI is present in over 30% of incontinent women and is described as mixed urinary incontinence (MUI) [4-6]. UI symptoms are highly prevalent among adult women (nearly 50% may experience UI2,7), negatively impacts the quality of life, and are associated with considerable personal and societal economic impact [7-9]. The prevalence of UI increases with age but is not a normal part of healthy aging. Significant risk factors include childbirth, hormonal changes, and chronic medical conditions such as diabetes, hysterectomy, obesity, and sedentary behaviour [10-12]. All these factors consequently can result in weakening or trauma to the pelvic floor muscles (PFM), increasing the probability of UI. Pelvic floor muscle training (PFMT), commonly known as Kegel exercises is considered first-line therapy [13-14]. However, the efficacy of PFMT relies on patient compliance and physical ability to perform proper PFM contractions [13,15]. Furthermore, biofeedback training with a physical therapist using a vaginal or rectal probe as well as the addition of passive electrical stimulation (ES) may be more effective than PFMT alone [16]. A novel technology to strengthen and improve the function of the PFM using High-Intensity Focused Electromagnetic Therapy (HIFEM) has recently been developed. HIFEM utilizes an alternating magnetic field passing through the tissue, inducing brain-independent contractions. These contractions are of higher tension and frequency than can be achieved with voluntary contractions or biofeedback during PFMT and are, therefore, defined as supramaximal. Moreover, since the magnetic field penetrates living tissues without attenuation, the induced contractions achieve greater depth and intensity [17,18]. The purpose of this study is to compare the efficiency of PFMT with biofeedback to the HIFEM procedure for the treatment of female UI.
Inclusion and Exclusion Criteria
This study included adult female subjects diagnosed with UI (either SUI, UUI, or MUI). Inclusion criteria were as follows: female aged 25-70 years, voluntarily signed informed consent, abstinence from any additional treatment of UI including a two-week wash-out period from any prior UI treatment. Exclusion criteria were any contraindication to either HIFEM or PFMT, inability to consent to the protocol or inability to comply with the protocol.
Ethical Consideration
The study design and treatment protocol was approved by the Advarra Institutional Review Board (ClinicalTrials.gov identifier: NCT03969368), and the study adhered to the ethical principles of the 1975 Declaration of Helsinki.
Randomization
This is a prospective randomized multi-center open-label (no masking) double-arm study. Subjects were recruited from the Investigators’ existing pool of patients and were randomly distributed into two study groups – HIFEM and PFMT by a computer-generated list.
Treatment Protocol
At the baseline visit, medical history was reviewed and the diagnosis of UI from either SUI, UUI, or MUI was confirmed. Additional causes such as medications, urinary tract infections, and urinary retention were ruled out.
HIFEM Group
Six 28-minute standardized treatments were delivered twice a week, over three consecutive weeks by BTL EMSELLA (BTL Industries Inc., Boston, MA) device. A fully clothed patient was correctly positioned to sit straight in the center of the chair applicator. The device administered an alternating magnetic field of 2.5 Tesla by stimulation coil, to provide non-invasive electromagnetic stimulation of pelvic floor musculature. The stimulation intensity (0-100%) was adjusted according to the patient's feedback based on maximum tolerance.
PFMT Group
A standardized biofeedback protocol adopted from Beth Israel Deaconess Medical Center Physical Therapy department was implemented at all sites. Six treatment visits were delivered twice a week, over three consecutive weeks. During treatment, a vaginal probe was inserted or palpation was performed to monitor therapy and the subject performed the therapy in the supine position with legs straight and slightly abducted.
All patients were required to complete all treatments and five follow-up visits at 1, 3, 6, 9, and 12 months. The occurrence of adverse events was monitored by an investigator while patients were also asked to report any sign of adverse event pain, injury, or discomfort during treatments.
Main outcomes Evaluation and Data collection
Standardized questionnaires were administered to assess symptoms at baseline and at each additional data point. UDI-6 (Urinary Distress Inventory) provided a brief assessment of the impact of symptoms of urinary incontinence (frequency of urination, urine leakage related to physical activity, bladder emptying, and pain or discomfort in the lower abdominal or genital area). ICIQ-LUTSqol (International Consultation on Incontinence Questionnaire Lower Urinary Tract Symptoms Quality of Life Module) evaluated the impact of urinary symptoms on physical activities, social activities/ relationships, and mood associated with the interference of UI with the patient’s everyday life. The evaluation of pelvic floor muscle strength was conducted through the palpation assessment (in the distal onethird of the vagina) according to the Oxford Grading system.
ICIQ-BD (International Consultation on Incontinence Questionnaire–Bladder Diary) was a three-day patient-completed record for documentation of the drinking habits, micturition (to determine urine frequency per 24 hours), bladder sensation (range 0-4; 0-no sensation of needing to pass urine, but passed urine for “social reasons”, 1-normal desire to pass urine and no urgency, 2-urgency but it had passed away before you went to the toilet, 3-urgency but managed to get to the toilet, still with urgency, but did not leak urine, 4-urgency and could not get to the toilet in time so you leaked urine), and pad usage. In addition, a Pad Usage Questionnaire was also utilized to document the number of hygienic pads used by subjects per day. The Subject Satisfaction Questionnaire (SSQ) evaluating patients’ satisfaction with the therapy outcomes was designed as two open-ended questions for summarising the patients' experiences during the therapy and after the treatment. Therapy Comfort Questionnaire (TCQ; 5-point Likert scale) recorded the patients’ comfort during treatments.
Statistical Methods
The descriptive statistic was calculated (mean, standard error of the mean). All data were analysed for normality (Shapiro-Wilk test). Based on the paired and independent variables measured at multiple time points, parametric tests (paired T-test, Oneway Repeated measures ANOVA) and their non-parametric alternatives (Wilcoxon test, Friedman test), were used. The significance level was set to α=0.05 (5%). The analysis was performed using the Microsoft Excel and Real Statistics Resource Pack add-in [19].
Out of the forty-nine patients recruited, thirty-eight (27-76 years old) completed the study, HIFEM (N=23) and PFMT (N=15) as shown in [Figure 1].
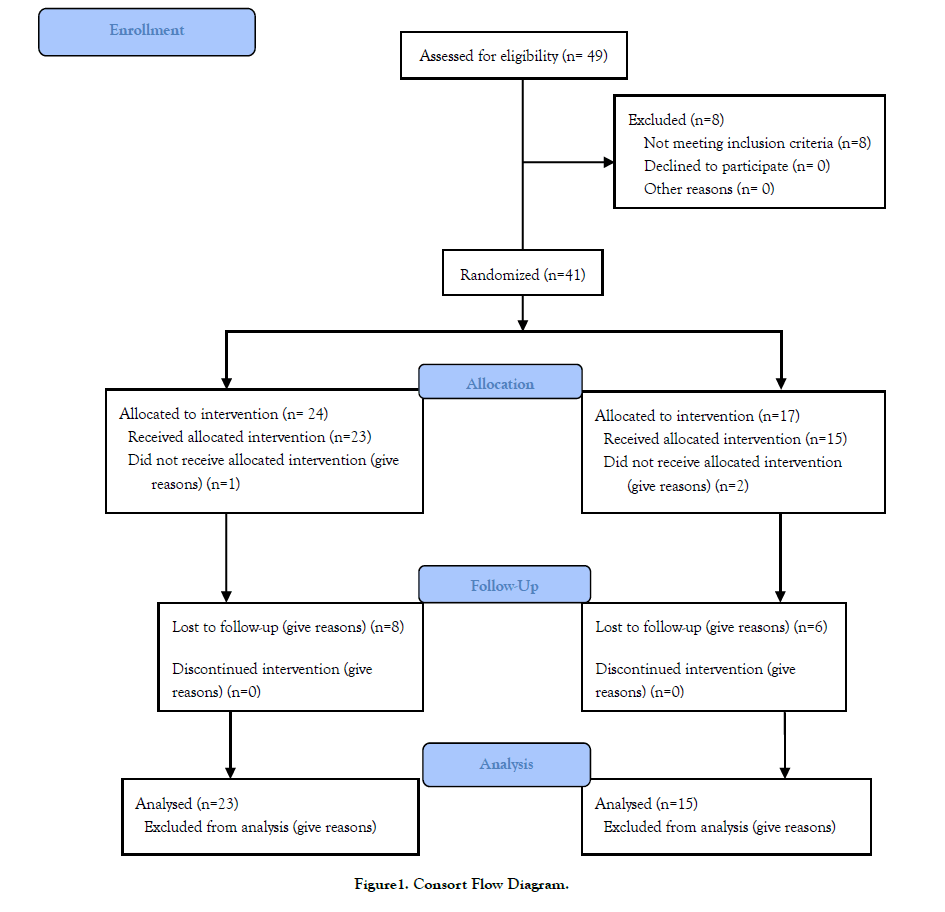
Figure 1:Consort Flow Diagram.
ICIQ-LUTSqol, UDI-6, and Palpation examination
a) HIFEM group
The ICIQ-LUTSqol score improvement [Figure 2] was observed after the last treatment (-8.2 points, p=7.2∙10-3, N=21) compared with ICIQ-LUTSqol baseline value (43.0±2.4 points), and continued improvement to 6-months with improvement of 35% (-15.2 points, p=4.4∙10-10, N=15). Improvement (N=7) was maintained to 12 months with an average value of 27.9±2.7 points (p=3.4∙10- 2). For the ICIQ-LUTSqol questionnaire, the HIFEM group, patients showed a 34% (-32.8 points, p=2.6∙10-3) improvement in bother score immediately after the treatment compared to a baseline of 95.5±10.0 points, and a 68% (-65.1 points, p=1.2∙10-8) improvement at 6 months, which was maintained (43%) with a slight decline at 12 months as well.
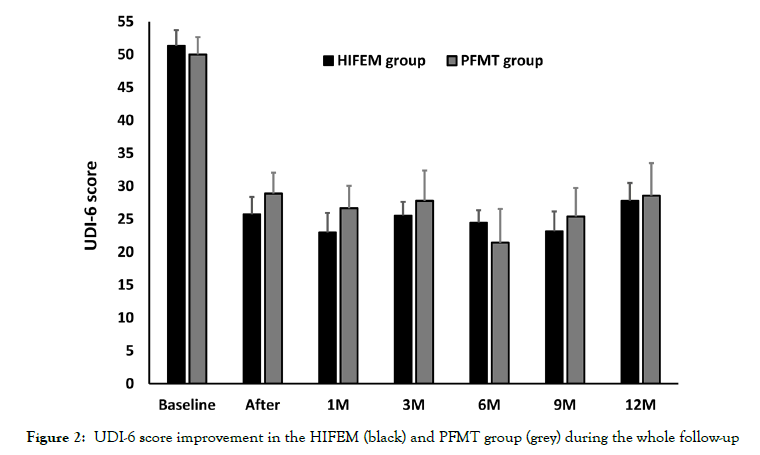
Figure 2:UDI-6 score improvement in the HIFEM (black) and PFMT group (grey) during the whole follow-up.
The UDI-6 [Figure 3] showed an average score of 51.3±4.1 points at baseline which significantly decreased to 25.7±3.7 points (N= 19, p=6.3∙10-5) and was maintained to 6 months (24.5±3.5 points, N=16) with a 52% improvement (p=1.5∙10-6). The improvement in the UDI-6 score was maintained at 12 months (27.8±4.7 points, N=7, p=2.2∙10-2).
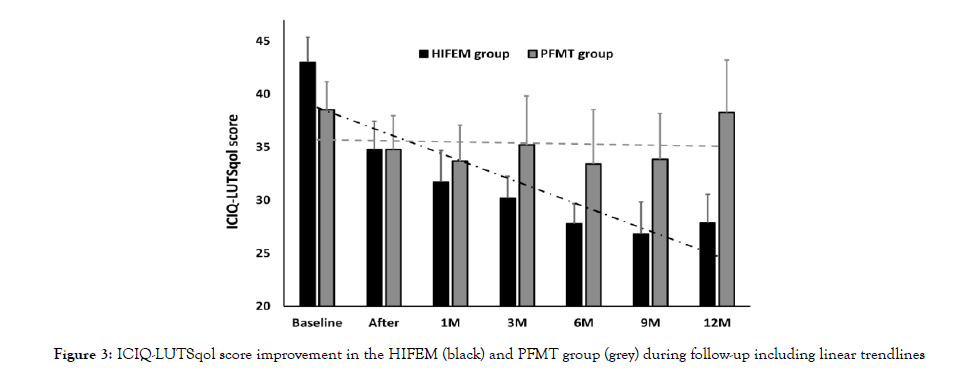
Figure 3: ICIQ-LUTSqol score improvement in the HIFEM (black) and PFMT group (grey) during follow-up including linear trendlines.
The average palpation value using the Oxford scale in HIFEMtreated subjects showed a significant improvement of +1.2 points at the first follow-up (73%, p=6.8∙10-4, N=18).
b) PFMT group
ICIQ-LUTSqol score and bother rate did not show a statistically significant change (p>5.0⋅10-2) at any follow-up period as shown in Fig. 2. The baseline value of 38.5±2.6 points declined the most at 6 months by -5.1 points (13%, N=7). The bother rate decreased immediately after the treatment from a baseline value of 94.2±12.6 points to 59.9±14.3 points and was maintained at 67.0±26.2 points 6 months post-treatment (-27.2 points, 29%, p=8.1∙10-1). The UDI-6 score significantly decreased exact time by -21.1 points (42%, N=15, p=1.9∙10-2), and was maintained to 6 months (-28.6 points, N=7, p=3.0∙10-6). At 12 months, the changes in UDI-6 did not achieve statistical significance. Palpation using the Oxford scale achieved a significant improvement value of +1.1 points at the first follow-up (64%, p=7.4∙10-3, N=15).
ICIQ-BD & Pad usage questionnaire
The micturition frequency (per 24 hours, the sum of day and night urine micturition frequency) and average bladder sensation were assessed from the ICIQ-BD questionnaire showing the improved trends following both investigated modalities. The averaged ICIQBD records for both groups are shown in [Table 1].
| PFMT group | Baseline | After | 1M | 3M | 6M | 9M | 12M |
|---|---|---|---|---|---|---|---|
| Frequency per day | 8 | 7 | 6.8 | 6.8 | 6.9 | 6.9 | 6.9 |
| Frequency per night | 0.8 | 0.5 | 0.5 | 0.3 | 0.5 | 0.5 | 0.5 |
| Frequency 24 hours | 8.8 | 7.5 | 7.3 | 7.2 | 7.2 | 7.4 | 7.4 |
| Average bladder sensation | 1.8 | 1.7 | 1.5 | 1.7 | 1.9 | 1.8 | 1.9 |
| HIFEM group | Baseline | After | 1M | 3M | 6M | 9M | 12M |
| Frequency day | 7.5 | 6.7 | 6.9 | 6.8 | 6.7 | 5.6 | 6.8 |
| Frequency night | 0.9 | 0.7 | 0.3 | 0.4 | 0.5 | 0.4 | 0.5 |
| Frequency 24 hours | 8.3 | 7.4 | 6.9 | 7.3 | 7.1 | 6 | 7.3 |
| Average bladder sensation | 2 | 1.4 | 1.3 | 1.3 | 1.4 | 1.3 | 1.4 |
Table 1: Averaged ICIQ-BD records for HIFEM and PFMT groups. Each visit is an average of the subject's three-day records. The average bladder sensation was counted by dividing the summary score of bladder sensation (assigned to the urgency of each micturition) in a day by Frequency per 24 hours .
The micturition frequency (per 24 hours) decreased in both groups. This was true for both nocturia and daytime micturition. Improvement was observed in both groups from 8-9 voids per day to a normal frequency of 7-voids per day. Nocturia was reduced from 0.8 to 0.5 points (PFMT group) and 0.9 to 0.5 points (HIFEM group).
In the HIFEM group, average bladder sensation decreased from a baseline value of 2.0±0.1 to 1.4±0.1 points after the last treatment (N=15). This level of improvement was maintained to 1 year, peaking at 9 months post-treatment (1.3±0.1, N=7) with a 34% change against the baseline. In the PFMT group, a minor treatment effect on decreasing average bladder sensation improvement was observed as shown in Tab.2. The highest change was achieved at 1 month (N=5) showing a 17% decrease. The effect then regressed at later follow-ups, returning and even exceeding the baseline values.
The number of hygienic pads used for protection during urine leakage was documented by ICIQ-BD and Pad usage Questionnaire. Pad records from ICIQ-BD and Pad usage questionnaires were merged and averaged to obtain usage per 24 hours at respective follow-ups [Table 2]. The number of pads declined after the last treatment in both groups. Baseline values of HIFEM=3.0±0.4 pads and PFMT=2.8±0.6 pads. In the HIFEM group (N=15), 86.7% reported an improvement in pad use at 6 months (p=8.4∙10-3). The average improvement showed a decrease of 1.7 pad/24 hours, and this effect was maintained for up to 1 year (p=1.7∙10-3). In the PFMT group (N=8), 62.5% decreased their pad usage. Significant improvement in the PFMT groups was observed only after 9 months (p=4.2∙10-2) and was maintained up to 1 year (p=4.2∙10-2) with -1.0 pad/24 hours.
| Baseline | After | 1M | 3M | 6M | 9M | 12M | |
|---|---|---|---|---|---|---|---|
| HIFEM group | 3.0±0.4 | 1.9±0.5 | 1.5±0.4 | 1.4±0.2 | 1.3±0.3 | 1.4±0.4 | 1.3±0.5 |
| PFMT group | 2.8±0.6 | 2.3±0.7 | 2.0±0.6 | 2.2±1.1 | 1.8±1.4 | 1.8±1.1 | 1.8±1.1 |
Table 2:Average numbers of hygienic pads (average+SEM) used for protection from urine leakage during the whole study.
Therapy Comfort and Satisfaction evaluation
Therapy comfort questionnaire showed on average 3.0±0.4 points in the HIFEM group and 2.2±0.4 points in the PFMT group. Throughout the subjective experiences from two open-ended questions for satisfaction evaluation, 86.4% of patients from the HIFEM group (N=22) reported less urine leakage and frequency. In addition, 63.6% noted less urgency, and the ease of therapy was appreciated by 54.5% of patients. In the PFMT group (N=14), 78.6% of patients endorsed the effect of PFM exercise, 71.4% noted less urine leakage and its frequency, and 64.3% declared that they are more informed about UI symptoms and treatment than before concerning adjustment of their liquid input.
Minimal Clinically Important Difference (MCID)
A MCID analysis was performed for ICIQ-LUTSqol and UDI- 6. Previous studies identified the MCIDs for the ICIQ-LUTSqol questionnaire as a difference of 4-6 points20 and for UDI-6 as 11 points21. Considering the formerly inferred threshold values, it can be concluded that the improvement achieved in the HIFEM group was clinically significant, due to sufficient differences in both questionnaires (minimal difference of ICIQ-LUTSqol=8.2 points and UDI-6=25.6 points). In the PFMT group, the MCID was achieved for UDI-6 (21.1 points), however, this was not the case for changes in the ICIQ-LUTSqol with a maximum change of 5.1 points.
Pelvic Floor Therapy with or without biofeedback as reported by [22, 23, 24] has traditionally been considered the standard for pelvic floor rehabilitation. This modality, however, has significant limitations. Most women with poor pelvic floor control have, by definition, poor muscle and nerve function. Any therapy requiring the patient to engage neurologically compromised and traumatized muscles can be challenging. Electrical stimulation has been used to overcome this limitation; however, it predominantly stimulates the muscles in close proximity to the electrodes, limiting the efficacy of this method due to the dependence on the electrode placement. The HIFEM technology overcomes this limitation by creating an electromagnetic field encompassing the entire pelvic area and engaging all pelvic floor and accessory musculature. Further, the HIFEM is supraphysiologic, engaging the muscles more intensely and more rapidly than is otherwise possible. Prior single-arm studies have supported HIFEM’s success, demonstrating significant improvement in continence and quality of life to 6 months post-treatment [17,18,25,26] reported on HIFEM compared to electrical stimulation for UI treatment using electromyographic measurements and 3D transperineal ultrasonography of the pelvic floor with the HIFEM group demonstrating superior results. This evidence also provided further insight to support the earlier findings [25, 26].
This study was designed to prospectively compare PFMT with biofeedback to HIFEM for improvement in female urinary continence. The study results demonstrated a significant improvement in the ICIQ-LUTS qol score in the HIFEM group. The improvement achieved statistical significance at the first followup and was maintained to 12 months. A peak improvement of 35% was noted at 6 months. Conversely, the PFMT group subjects did not show a statistical improvement in ICIQ-LUTSqol scores at any follow-up interval. The UDI-6 indicated improvement in both the HIFEM and PFMT groups up to 52% and 42% respectively to 12-month follow-up. Of particular note is the ICIQ-LUTSqol bother rate evaluation. In this analysis, the HIFEM group achieved about 2.4 times higher improvement (P<0.01) in QoL than in the PFMT group (P>0.05) at the 6-month follow-up interval.
Evaluation with the ICIQ-BD indicated the micturition frequency per 24 hours decreased in both groups from 8-9 times per day to 7 times per day. Bladder sensation improvement was seen only in the HIFEM group and was most prominent at 9 months (-34%). PFMT appeared to have minimal effect on bladder sensation.
Regarding pad usage and SSQ, in the HIFEM group, 86.7% of subjects reported an improvement in pad use at 6 months, and 86.4% of patients reported less leakage and frequency. In the PFMT group, 62.5% of subjects reported improvement in pad usage and 71.4% reported less leakage and frequency. Quantitatively, the HIFEM group reduced pad usage by 1.7 pads/24 hours and the PFMT group reduced pad usage by 1.0 pad/24 hours. This was maintained for 1 year. The clinical significance of results was demonstrated in the HIFEM group for the ICIQ-LUTSqol but not in the PFMT group. UDI-6 scores initially demonstrated clinically significant improvement in both groups but the PFMT group did not show significant (P>0.05) improvement at 12 months compared to the HIFEM group.
The strengths of this study were the randomized prospective multicenter design and standardization of both therapy arms. This is the first study to evaluate PFMT and HIFEM in a prospective comparative way. There were also limitations to the study. The most significant was the drop-out rate exacerbated by the COVID-19 pandemic. This may have led to certain aspects of the study being underpowered. Numerous key measures, however, achieved statistical significance.
The HIFEM procedure appears to be a safe and effective modality for improving female continence and related quality of life to 1-year. When compared to the conventional pelvic floor exercise, the HIFEM procedure may be more effective and better tolerated. Larger, higher-powered studies are warranted.
The authors have declared they have no conflicts of interest
None
This IRB-approved study (ClinicalTrials.gov Identifier: NCT03969368) was sponsored by BTL Industries.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Guerette N, Molden S, Gopal M, Kohli N (2023) Randomized Trial of HIFEM Pelvic Floor Stimulation Device Compared with Pelvic Floor Exercises for Treatment of Urinary Incontinence. J Women's Health Care. 12(9):680.
Received: 21-Aug-2023, Manuscript No. 26283; Editor assigned: 25-Aug-2023, Pre QC No. 26283; Reviewed: 30-Sep-2023, QC No. 26283; Revised: 08-Sep-2023, Manuscript No. 26283; Published: 16-Sep-2023 , DOI: 10.35248/2167-0420.23.12.680
Copyright: © 2023 Guerette N et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Sources of funding : This IRB-approved study (ClinicalTrials.gov Identifier: NCT03969368) was sponsored by BTL Industries