
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 5
Background: Combination of Local anaesthetics for epidural anaesthesia will improve block characteristics and reduce toxicity. Previous studies have shown lidocaine to shorten onset time while bupivacaine prolongs duration of anaesthesia.
Objective: The aim of this study was to comparatively evaluate the block characteristics of epidural injection of different lidocaine-bupivacaine mixtures for lower limb surgeries.
Methods: Sixty-three patients receive either 15 ml of 0.5% Isobaric-bupivacaine and 5 ml of 2% Lidocaine (group A), or 15 ml of 0.5% Isobaric-bupivacaine, 2.5 ml of 2% Lidocaine and 2.5 ml normal saline (group B) or 15 ml of 0.5% Isobaric-bupivacaine and 5 ml of normal saline (group C). The primary outcome was the onset time of sensory block. The secondary outcomes were the onset of motor blockade, degree of sensory block level and motor blockade, duration of sensory block and motor block and the incidence of side effects. Data collected were analysed using Statistical Package for Scientific Solutions (SPSS) version 20 and presented as tables, graphs and charts. A p-value of <0.05 was considered as statistically significant.
Results: The onset time of sensory and motor block were significantly faster in Group A (6.33 ± 1.35 min and 16.48 ± 1.66 min), compared with Group B (8.05 ± 1.77 min and 19.52 ± 1.89 min) and Group C (10.55 ± 1.91 min and 25.52 ± 1.72 min), p<0.001 and p<0.001 respectively. The maximum height of sensory block achieved was T3 in Group A, T3 in Group B and T4 in Group C, p<0.001. The duration of sensory block was statistically longer in Group A (279.81 ± 9.37 min) compared with Groups B (267.95 ± 5.92 min) and C (265.45 ± 4.91 min), p<0.001. The duration of motor block was 140.67 ± 2.24 min in Group A, 139.81 ± 2.38 min in Group B and 139.58 ± 1.54 min in Group C, p=0.21.
Conclusion: This study shows that when different volumes of the same concentration of lidocaine is added to specific amount of isobaric bupivacaine epidural injection, it provided faster onset and prolonged duration of sensory block, with stable haemodynamic, and no complications compared to when bupivacaine alone is used.
Epidural; Block characteristics; Lidocaine-bupivacaine mixture; Lower limb
Lower Limb (LL) surgery is painful, however, pain free lower limb surgeries like arthroscopy, bone fusion, open and close reduction of fractures and fixation, surgical removal of bones, nails and implants, amputations, tendon repair, skin grafting and flap cover, can be facilitated using various anaesthetic techniques [1,2]. Regional Anaesthesia (RA) techniques like peripheral nerve blocks, local infiltration and Neuraxial blocks are preferred currently [1,3]. The benefits of epidural anaesthesia with catheter in situ include improved intraoperative anaesthesia, prolonged postoperative analgesia, and improved physiologic stress responses to surgery, decrease surgical complications, improved outcomes and satisfaction in surgical patients [4]. Epidural can be used in combination with either general or spinal anaesthesia or as sole epidural technique [5].
Epidural anaesthesia involves a reversible loss of sensation and motor function adequate for surgery following injection of Local Anaesthetics (LA) into the epidural space [5]. Commonly used or studied LAs include Lidocaine, bupivacaine, ropivacaine and levobupivacaine [6-9].
Lidocaine has faster onset but shorter duration of action and safe profile even in high doses [6]. When compared with bupivacaine, Lidocaine provided significantly faster onset of epidural analgesia [10]. Lidocaine has a maximum allowable safe dose of 3 mg/kg without adrenaline and 7 mg/kg with adrenaline [11]. However, the maximum doses of local anaesthetics are affected by the site of injection, tissue distribution, metabolism and excretion [11]. The addition of adrenaline to local anaesthetics decreases the systemic absorption of the agent approximately by one-third [12]. Bupivacaine has a maximum allowable safe dose of 2 mg/kg (about 140 mg for an average 70 kg man) with or without adrenaline. Thus, indicating that adrenaline has little or no effect on safe dose of bupivacaine [11,12].
Researchers have demonstrated that epidural bupivacaine analgesic effect can be prolonged by the use of adjuvants like magnesium sulphate, clonidine, dexmedetomidine, neostigmine, midazolam, dexamethasone, and fentanyl [13-17]. They have also shown that the combination of bupivacaine with adjuvants can lead to dose reduction, improvement in quality of analgesia, as well as decrease in bupivacaine related toxicity [13,15,17]. Zand et al. showed in their study, that combination of bupivacaine with lidocaine can improve the epidural block characteristic, quality of analgesia and minimize undesirable effects. Epidural anaesthesia with lidocaine-bupivacaine mixtures have been widely studied and used in clinical practice, but studies have not extensively evaluated the block characteristics of different lidocaine-bupivacaine mixtures [7,10,18,19]. Thus, the present study comparatively evaluated the block characteristics of epidural injection of different lidocaine- bupivacaine mixtures for lower limb surgeries.
This prospective double-blind randomized study was conducted in the orthopaedic and plastic surgery theatres, Post-Anaesthetic Care Unit (PACU) and wards of Federal Medical Centre (FMC), Owerri, and Imo State.
Ethical approval was obtained from the Health Research and Ethics Committee of the institution and also approved by the West African College of surgeons. The study was explained to all patients scheduled for lower limb surgical procedures and a written informed consent obtained from each of the patients who were willing to participate in the study. We recruited patients of American Society of Anesthesiologists (ASA) physical status I-II, 18 years to 65 years, of either sex, posted for elective Lower Limb surgeries under sole epidural anaesthesia. Patients of ASA class III or higher, who refused to participate, or with history of allergy to the study drugs, gross spinal abnormality, local infection, known medical history of hypertension, diabetes mellitus, peptic ulcer disease, cardiac, pulmonary, hepatic, renal or bleeding disorders were excluded. Also excluded were patients with head injury, cognitive impairment, peripheral neuropathy, or other neurological involvement/diseases. This study was conducted between July 2019 and June 2020.
Sample size was calculated using a significance level of 5% and power of study 80% and some other assumptions. About 19 patients were required in each group to demonstrate changes in onset of action of significance. However, allowing for 10% attrition to make allowance for loss of follow-up/protocol violation, a total of 63 patients were recruited for the study.
Patients were randomized into three groups (A, B and C) containing 21 patients each by a pick from an envelope by a research assistant; to receive 20 ml mixture of either 15 ml of 0.5% Isobaric-bupivacaine and 5 ml of 2% Lidocaine (group A), 15 ml of 0.5% Isobaric-bupivacaine, 2.5 ml of 2% Lidocaine and 2.5 ml normal saline (group B) or 15 ml of 0.5% Isobaric-bupivacaine and 5 ml of normal saline (group C).
Preoperative evaluation was done at least a day before the surgery, to establish rapport with the patient, clinically ascertain fitness to undergo anaesthesia/surgery, establish pre-anaesthetic and postoperative plans, and obtain informed written consent. All the patients received oral diazepam 5 mg at night. In the theatre, pre-anaesthetic check was carried out on the anaesthetic machine, airway maintenance devices and suction machine, and two carts prepared for pain care and emergency resuscitation.
In the surgical theatre, patients were received and identified and baseline peripheral oxygen saturation (SpO2), systolic, diastolic and mean arterial blood pressures (SBP, DBP and MAP) respectively, Heart Rates (HR) and rhythm and body temperature were measured and recorded. Intravenous access was secured in the non-dominant upper limb with appropriate-sized cannula. Intravenous ondansetron 4 mg was given as prophylaxis for nausea and vomiting. Preloading was done with 10 ml/kg of 0.9% saline solution, before activating epidural anaesthesia, and maintained with 4-8 ml/kg/hour as needed during surgery.
The epidural set was mounted on a sterile tray and catheter primed via its filter using 2% lidocaine in a sterile 5 ml hypodermic needle. The patient was then placed in a sitting position with both feet on a stool, flexed knees slightly higher than the flexed hips, arms round about a pillow, head down and back arched outwards. The back was aseptically cleaned using alcohol-chlorhexidine solution and draped. The interspace between the third and fourth lumbar vertebrae (L3/L4) was located using the iliac crests as landmark (Tuffier's line/intercristal line). A skin wheal was raised and the supraspinous ligaments infiltrated using 2 ml of 2% lidocaine (diluted to 4 ml) in a sterile 22 Gauge hypodermic needle after negative aspiration for blood. Thereafter, an 18-Gauge Touhy epidural needle (Epidural Minipack System 1, Portex, Smiths Medical International limited) was introduced via L3/L4 interspace after skin puncture using a Sise needle. It was advanced to about the 2 cm mark and the stylet removed. An air-filled syringe was then attached and advanced gradually together with the needle till the epidural space was located and confirmed using the loss of resistance to air technique. The depth of the Touhy needle from the epidural space was noted and then a 20-G primed catheter threaded via the needle, leaving about 3-5 cm in the epidural space, needle removed and sterile dressing with adhesive tape applied to secure catheter on the patient's back.
Clear fluid appearing in the catheter during insertion or aspiration may be due to injected of saline, local anaesthetics or cerebrospinal fluid. However, False negative aspiration of blood and CSF can occur during epidural anaesthesia thus, the need for a test dose using 3 ml of 1.5% lidocaine with epinephrine 1:200,000 injected through the catheter to confirm correct catheter placement. Aspiration of blood necessitated repeating the procedure, however in case of aspiration of CSF, epidural block was abandoned and patient excluded from the study, in order to avoid the risk of extensive spinal anaesthesia. Increase in heart rates and/or extensive motor block after 5 minutes of test dose injection indicated vascular or subarachnoid catheter placement/ advancement and thus was adjusted. Negative response to epidural test dose injection, epidural anaesthesia was achieved by injecting 20 ml of study mixtures. Group A received 15 ml of 0.5% Isobaric- bupivacaine and 5 ml of 2% Lidocaine, Group B received 15 ml of 0.5% Isobaric-bupivacaine, 2.5 ml of 2% Lidocaine and 2.5 ml normal saline and Group C received 15 ml of 0.5% Isobaric- bupivacaine and 5 ml of normal saline. Patients were placed on a modified Trendelenburg with lateral (surgical site) tilt position [5,7,19,20]. The study drugs were prepared by the research assistant and the basis of the grouping made known at the end of the study to avoid bias.
Having achieved the desired level of sensory (T10) and motor (modified Bromage score 2) blocks, the patients were returned to supine/appropriate surgical position till the end of the surgery. The HR, electrocardiography, SpO2, and body temperature were monitored continuously and recorded. The SBP, DBP, and MAP were recorded every 3 minutes for 30 minutes, then every 5 minutes until the end of surgery. Sensory block was assessed every 5 minutes using cold swab to test for sensory loss to cold and; Motor block every 5 minutes using Modified Bromage score (0=Full flexion of knees and feet (no block); 1=Just able to flex knees, full flexion of feet; 2=Unable to flex knees, but some flexion of feet possible; 3=Unable to move legs/feet). The sensory and motor block characteristics were recorded to ascertain the onset of analgesia and motor blockade, loss of sensation at the level of the umbilicus (T10) maximum sensory level using cold swab test and modified Bromage score 2 motor blockades.
All assessments were made by the researchers who were blinded to the study drugs used. The intraoperative SBP, DBP, and MAP were monitored every 5 minutes, SpO2, heart rate and rhythm, peripheral temperature, and surgical blood loss were monitored continuously. Hourly urine output was also monitored.
For the purpose of this study, bradycardia was taken as decrease in heart rate of >25% from the baseline or PR <0 beat per minute, hypotension as a decrease of >20% SBP from the baseline or decrease of >25% MAP from the baseline, while desaturation was taken as a value of SpO2 <95%.
Adverse effects like Hypothermia was prevented and managed by giving warm fluids and keeping the theatre temperature at 25˚C. The block characteristics were observed and recorded intraoperatively. The sensory and motor blocks were assessed every 5 minutes to determine the highest level of sensory block and degree of motor block, thereafter, assessed every 15 minutes to determine the time for two segment regression and total volume epidural injection given. Sedation was assessed and recorded every 15 minutes using a six-point Ramsay Sedation Score if awake; 1-Anxious, agitated, restless; 2-Cooperative, oriented, tranquil; 3-responsive to commands only; or asleep but 4-Brisk response to light glabellar tap or loud auditory stimulus; 5-Sluggish response to light glabellar tap or loud auditory stimulus; 6-No response to light glabellar tap or loud auditory stimulus.
At the end of the surgery, patients were transferred to the PACU for 4 hours monitoring and data collection. The SBP, DBP, MAP, SpO2, heart and respiratory rates, temperature, motor-block, pain and sedation were monitored and recorded at 0 (on arrival in PACU), 15 and 30 minutes, 1,2,3 and 4th hour following recovery. Motor-block of the lower limbs was assessed using the modified Bromage score. Before discharge from PACU, patients achieved a modified Bromage score of ≤ 1. Patients’ follow up continued in the ward post-operatively. Epidural catheters were removed aseptically at the 24th hour post insertion. Patients were assessed at 6th and 24th hour post-operatively in the ward for their degree of satisfaction with the technique using Likert scale 1-Very satisfied, 2-Somewhat satisfied, 3-Neither satisfied nor dissatisfied, 4-Somewhat dissatisfied, 5-Very dissatisfied.
The data collected were analysed using SPSS version 20 and presented as tables, graphs and charts. Categorical data were presented as frequencies and percentages. Categorical data were analysed using chi-square test. Parametric data were reported as mean ± standard deviation. Continuous data were analysed using analysis of variance (ANOVA). Non-parametric data were presented as frequencies and percentages and analysed using Kruskal-Wallis test. Kruskal-Wallis test was also used to evaluate the sensory block level, maximum motor block score and intergroup differences in the quantity of ephedrine used. A p-value of<0.05 will be considered as statistically significant.
Sixty-three patients were recruited and they completed the study, twenty-one patients each in groups A, B and C.
Demographic characteristics
The mean age was comparable among Group A (40.00 ± 9.01 years), Group B (39.86 ± 8.52 years) and Group C (40.00 ± 7.49 years), p=0.10. The mean height was higher in Group A (160.00 ± 4.39 cm), compared to Group C (159.00 ± 3.81 cm) and Group B (158.00 ± 3.81 cm) and the difference was not significant (p=0.28). The mean weight was significantly lower in Group A (70.00 ± 6.20 Kg) compared to Group B (71.33 ± 6.61 Kg) and Group C (80.00 ± 4.04 Kg), p<0.001. The mean BMI was significantly lower in Groups A (27.40 2.80 Kg/m2), compared to Group B (28.58 ± 2.48 Kg/m2) and Group C (31.66 ± 1.65 Kg/m2), p<0.001. The gender distribution between male and female was statistically comparable (p=1.00), and Group A having 10/11 (47.6/52.4), Group B 11/10 (52.4/47.6), and Group C 11/10 (52.4/47.6) (Table 1).
| Variable | Group A (n=21) | Group B (n=21) | Group C (n=21) | p-value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Age (year) | 40.00 ± 9.01 | 39.86 ± 8.52 | 40.00 ± 7.49 | 0.1 |
| Height (cm) | 160.00 ± 4.39 | 158.00 ± 3.81 | 159.00 ± 3.81 | 0.28 |
| Weight (kg) | 70.00 ± 6.20 | 71.33 ± 6.61 | 80.00 ± 4.04 | <0.001* |
| BMI (kg/m2) | 27.40 ± 2.80 | 28.58 ± 2.48 | 31.66 ± 1.65 | <0.001* |
| Gender | 10/11 (47.6/52.4) | 11/10 (52.4/47.6) | 11/10 (52.4/47.6) | 1 |
| (male/female)% |
Note: * indicates significant difference between groups p<0.05.
Table 1: Comparative demographic characteristics of the study groups.
Surgical and anaesthetic block characteristics
The ASA I/II in Group A was 12/9, Group B was 1/20 and Group C was 1/20, and the distribution was statistically significant p<0.001. The difference in mean duration of surgery in Group A (163.57 ± 11.69 min), Group B (165.86 ± 9.34 min) and Group C (164.58 ± 10.19 min) was comparable, p=0.77. The mean onset time of sensory block was significantly shorter in Group A (6.33 ± 1.35 min), compared with Group B (8.05 ± 1.77 min) and Group C (10.55 ± 1.91 min), p<0.001. The mean onset of motor block (modified Bromage 1) was significantly reduced in Group A (16.48 ± 1.66 min), compared with Group B (19.52 ± 1.89 min) and Group C (25.52 ± 1.72 min), p<0.001. The mean peak onset of motor block (modified Bromage 3) was also significantly shorter in Group A (16.68 ± 1.66 min), compared with Group B (19.76 ± 2.23 min) and Group C (25.55 ± 1.76 min), p<0.001. The maximum height of sensory block achieved in Groups A and B was T3 while Group C has T4 (p<0.0001). The mean duration of sensory block was significantly prolonged in Group A (279.81 ± 9.37 min), more than in Group B (267.95 ± 5.92 min) and Group C (265.45 ± 4.91 min), p<0.0001. Also, the duration of motor block was longer in Group A (140.67 ± 2.24 min), compared with Group B (139.81 ± 2.38 min) and Group C (139.58 ± 1.54 min), however, the difference was not statistically significant (p=0.21) (Table 2).
| Variable | Group A (n=21) Mean ± SD/median | Group B (n=21) Mean ± SD/median | Group C (n=21) Mean ± SD/median | p-value |
|---|---|---|---|---|
| Onset of sensory block (min) | 6.33 ± 1.35 | 8.05 ± 1.77 | 10.55 ± 1.91 | <0.001* |
| Onset of modified Bromage 1 (min) | 16.48 ± 1.66 | 19.52 ± 1.89 | 25.52 ± 1.72 | <0.001* |
| Peak onset of modified Bromage 2/3 (min) | 16.68 ± 1.66 | 19.76 ± 2.23 | 25.55 ± 1.76 | <0.001* |
| Maximum height of sensory block | T3 (T3 – T5) | T3 (T3 – T6) | T4 (T4 – T7) | <0.001* |
| Duration of sensory block (min) | 279.81 ± 9.37 | 267.95 ± 5.92 | 265.45 ± 4.91 | <0.001* |
| Duration of Motor Block (min) | 140.67 ± 2.24 | 139.81 ± 2.38 | 139.58 ± 1.54 | 0.21 |
| ASA I/II | 12-Sep | Jan-20 | Jan-20 | <0.001* |
| Duration of surgery (min) | 163.57 ± 11.69 | 165.86 ± 9.34 | 164.58 ± 10.19 | 0.77 |
Note:* indicates significant difference between Groups p<0.05.
Table 2: Patient’s scoring on the Kawasaki Disease scoring system.
Figure 1 shows the distribution of types of surgery done among groups A, B and C. Open reduction and internal fixation surgery for orthpaedic fractures constituted 12.7% in Group A, 12.7% in Group B and 11.2% in Group C. While ankle reconstruction and flap incidence were similar in Group A (7.9% and 7.9%), Group B (7.9% and 7.9%) and Group C (7.9% and 7.9%) respectively. However, the figure shows that amputation incidence was more in Group C (6.4%) compared to Group A (4.8%) and Group B (4.8%) (Figure 1).
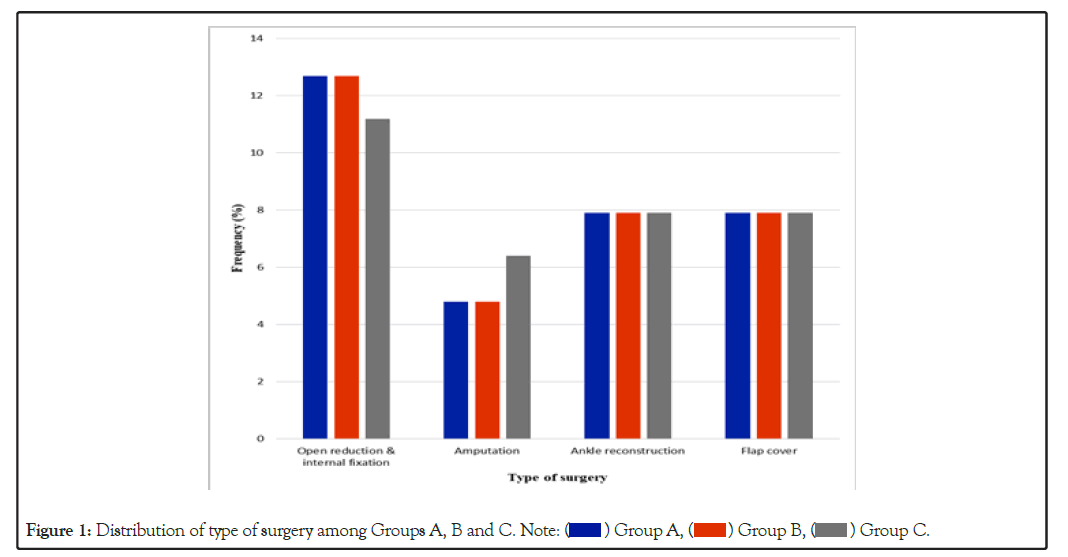
Figure 1: Distribution of type of surgery among Groups A, B and C.
Haemodynamic characteristics
Figure 2 shows the graphical representation of the intraoperative mean heart rate among the groups. There were more steep fluctuations in the intraoperative mean heart rate among the groups, but more on Group B compared to Group A and Group B (Figure 2).
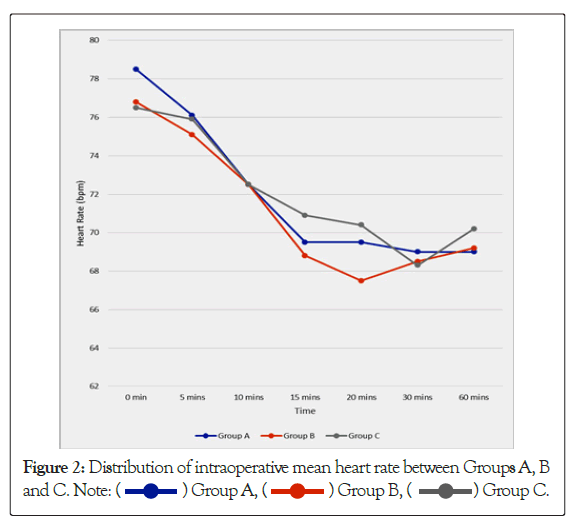
Figure 2: Distribution of intraoperative mean heart rate between Groups A, B and C.
Figure 2 shows the graphical trend in the intraoperative mean arterial pressure among the groups. The trend was observed to fluctuate more in Group A compared to Group B and Group C (Figure 3).
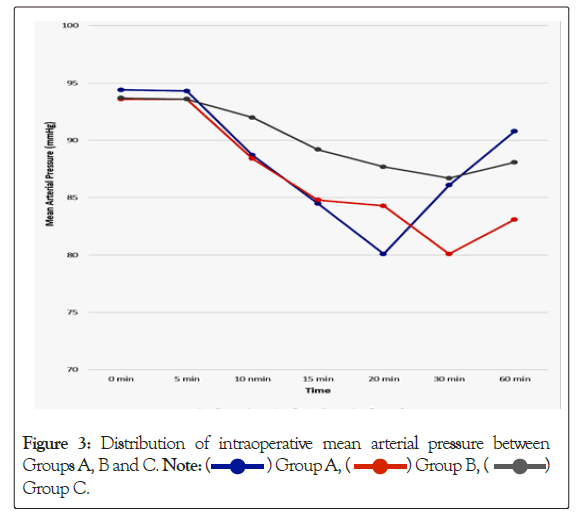
Figure 3: Distribution of intraoperative mean arterial pressure between Groups A, B and C. Group C.
Group C.
The findings of this study demonstrated that the administration of the mixture of 5 ml 2% lidocaine with 15 ml 0.5% bupivacaine provided effective epidural anaesthesia and analgesia for lower limb surgeries. The sensory block characteristics showed that the time taken to reach T10 dermatome was significantly rapid (6.33 ± 1.35 min). The maximum sensory block level (T3) was also significantly higher in the different groups of patients that received epidural injections of lidocaine-bupivacaine mixtures compared with the bupivacaine group.
This is consistent with Ozmen et al. finding, that lidocaine addition to bupivacaine significantly lowered the sensory block onset time compared to bupivacaine alone. Although Zand et al. and Powell et al. had similar faster onset of sensory block, their onset time for sensory block contrast that of the present study [21]. Zand et al. used the mixture of 9 ml of 0.5% bupivacaine and 9 ml of 2% lidocaine and noted longer onset time of sensory block of 21 ± 3.37 min. Powell et al. used 5 mL of 0.25% bupivacaine plus 5 mL of 1% lidocaine and reported almost similar onset time of sensory block of 8.5 ± 4.6 min. Thus, adapting to Verghese et al. observation that the efficacy of epidural block is related to the concentration of local anaesthetic and its volume [22]. The total volumes of local anaesthetic mixture used in all the 3 groups were comparable. However, the effect of concentration on block characteristics could be related to the variation in the onset time of sensory block between the different mixtures of lidocaine-bupivacaine used in the present study.
The high dermatomal spread with lidocaine-bupivacaine combination observed in this study is consistent with that of other researchers [7,10]. Higuchi et al. reported that the spread of local anaesthetic solutions in the epidural space and their principal sites of action are complicated, thus can affect the block characteristics [22,23]. The volume of local anaesthetic injected into the epidural space affects the level of sensory block. However, the same volume was used in this study. The relationship of spread of epidural local anaesthetic, weight and body–mass index has been documented [24]. Curatolo et al. reported that the spread of epidural local anaesthetic increases significantly with increasing weight, body– mass index, and decreasing body height. But this differed in the present study, that noted the peak sensory block level of T3 in patients with lower BMI (27.40 ± 2.80 kg/m2), Weight (70.00 ± 6.20 kg) and higher height (160.00 ± 4.39 cm) that received epidural injection of lidocaine-bupivacaine. This therefore corroborates with the report of Simon et al. and Bromage that the spread of epidural anaesthesia is highly variable [25,26]. Some of the variability is intrinsic to patients and not dependent on variations in technique or the drugs administered. We did not evaluate the sensory block regression.
The inconsistency with our study could be explained by the variability in the action of local anaesthetic injected into the epidural space. It has been noted that the epidural space contents are discontinuous circumferentially. The anterior epidural space is isolated from the rest of the epidural space and is nearly filled with veins accept caudal to the L4–L5 intervertebral disk, where a fat-filled anterior epidural space develops, while the lateral epidural compartments contain fat and nerves, which is lobulated by septae. But, the posterior fat-filled epidural compartment is enclosed, and it’s not continuous with the lateral compartment. When epidural local anaesthetic solution injection is done via the medial approach, it is assumed to be likely injected into or near the posterior epidural fat, and not into the lateral or anterior space. The duration of sensory and motor blocks in a patient after epidural anaesthesia is a factor of the degree of the sensory and motor blocks. Large volume of local anaesthetic causes prolonged sensory and intense motor blocks [23]. The combination of lidocaine-bupivacaine was evaluated in this study, to determine if there is an additive effect in the duration of sensory and motor blocks. Adding lidocaine to bupivacaine allows the combination of fast block onset of lidocaine to long block duration of bupivacaine. Hence, the present study showed a significant prolongation of sensory block in the lidocaine- bupivacaine combination.
Local anaesthetics are weak bases, and they are present in plasma in 2 different forms: freely circulating (toxic form) or bound to plasma proteins. The plasma proteins involved are albumin and more preferentially alpha acid glycoprotein which is rapidly saturated. Cuvillon et al. affirms that this saturation mechanism is amplified with mixture [27]. Also, Clarkson et al. [28] reported that epidural injection of lidocaine-bupivacaine produces more free lidocaine in plasma, resulting in a more rapid fixation kinetics than bupivacaine, thus, lidocaine would fix more to sodium channels for low concentrations and low stimulations, this effect is not seen with bupivacaine even with increasing concentrations. Clarkson and colleagues noted that adding lidocaine to bupivacaine would minimize bupivacaine dose, which is more cardiotoxic than lidocaine, as a result of its blocking effect on the heart sodium channels; the mixture of lidocaine-bupivacaine would be much safer than bupivacaine alone. This also corroborates with Jong et al. finding on neurological effect of bupivacaine [29]. They observed that, lidocaine-bupivacaine mixtures are less neurotoxic compared to bupivacaine alone. The cardiovascular effects of epidural anaesthesia are proportional to the height of block and they result from denervation of the sympathetic outflow tracts. This produces dilatation of resistance and capacitance vessels and results in changes in the haemodynamic profile of the patients [30,31]. We demonstrated that the haemodynamic disturbances associated with administration of local anaesthetic agents into the epidural space were significantly reduced. However, the addition of high concentration of lidocaine to bupivacaine had more fluctuations compared with lower concentration of lidocaine mixed with bupivacaine and bupivacaine alone. In another study conducted by Seow et al., they reported that epidural injection of lidocaine- bupivacaine significantly reduced the mean arterial pressure in their study, but did not significantly alter the heart rates [32].
Bradycardia is a common cardiovascular system complication of epidural anaesthesia. For the purpose of this study, bradycardia was taken as decrease in heart rate of >25% from the baseline or PR<50 bpm. Lesser et al. in their study reported that bradycardia may occur at any time during neuraxial anesthesia regardless of the duration of anesthesia and that low baseline heart rate increases the risk [33]. Bradycardia following epidural injection of local anaesthetic results from the blockade of sympathetic cardiac accelerator fibers and decreased venous return to the heart [31,34]. It can be treated with atropine [35]. However, this complication was not observed in this study. There was a reduction in heart rate but did not reach the value set as bradycardia. This could be attributed to the proper patient’s selection, preparation and use of ondansetron premedication which has been shown to inhibit Bezold Jarish reflex [34]. Also, all the patients were properly monitored throughout the study period.
There is a relationship between epidural anaesthesia and blood pressure changes. Epidural injection of lidocaine-bupivacaine or bupivacaine can result in cephalad spread of the drug. This produces neuronal transmission blockade that results in decrease in sympathetic tone of blood vessels. The decreased vasomotor tone leads to the dilatation of the arterioles and pooling of blood in the capacitance vessels, thus, resulting in hypotension [31,36]. Hypotension is a decrease of >20% SBP from the baseline or decrease of >25% MAP from the baseline. Campagna et al. reported that the main cause of hypotension following epidural anaesthesia is the decrease in the sympathetic outflow causing arterial vasodilatation [34], a decrease in venous return and consequently resulting in the activation of the Bezold Jarish reflex. Bezold Jarish reflex elicits a triad of bradycardia, vasodilatation and further hypotension by activation of 5-HT3 receptors within the intracardiac vagal nerve endings. Hypotension due to epidural injection of local anaesthetic can be treated with intravenous ephedrine. It can also be managed with intravenous fluids. Holte et al. observed that both ephedrine and intravenous fluid have comparable hemodynamic effects when applied 90 min after establishing an epidural blockade [36]. Remarkable blood loss during surgery can also cause haemodynamic instability. In our study, significant blood loss was avoided by careful selection of patients, positioning surgical site above the level of the heart, haemodilution (Preloading), use of tourniquet and drugs like tranexamic acid. Blood loss was also managed with fluid therapy.
Epidural anaesthesia can be complicated by shivering. Ponte et al. reported an incidence of 27.5% in their study [37]. Shivering during and after surgery can cause some discomfort, and at times exacerbates postoperative pain. It can also interfere with patient’s monitoring. Shivering has been shown to increase oxygen consumption as much as 500% and accompanies increase in minute ventilation, as well as results in increase in catecholamine release, cardiac output, heart rate blood pressure and intraocular pressure [38]. Ozaki et al. reported that post-anesthetic shivering is spontaneous, involuntary, rhythmic, oscillating, tremor-like muscle hyperactivity that increases metabolic heat production up to 600% [39]. However, the mechanism of shivering under epidural anaesthesia is not clear. Hynson et al. noted that shivering may be a normal thermoregulatory mechanism in response to core hypothermia due to redistribution of heat from core to periphery [40]. However, non-thermoregulatory shivering also occurs in normothermia patients. The study agents administered to all the patients were within the safe maximal dose.
This study shows that when different volumes of the same concentration of lidocaine is added to 15 ml of 0.5% of isobaric bupivacaine epidural injection, it provided faster onset and prolonged duration of sensory block, with stable haemodynamic, and no complications compared to when bupivacaine alone is used. We recommend that epidural injection of lidocaine-bupivacaine mixture should be used for lower limb orthopaedic surgeries, as it provides faster onset and prolonged duration of sensory block and tropical and global studies in block characteristics of different volumes of the same concentration of lidocaine added to specific amount of isobaric bupivacaine for epidural injection should be done to improve knowledge in the practice of neuraxial block.
[Cross ref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [Pubmed]
[Cross ref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Cross ref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Cross ref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
Citation: Kalu UM, Nnaji CT, Imarengiaye C (2022) Randomized Comparative Evaluation of the Block Characteristics of Epidural Injection of Different Lidocaine-Bupivacaine Mixtures for Lower Limb Surgeries. J Anesth Clin Res. 13:1060.
Received: 03-May-2022, Manuscript No. JACR-22-17274; Editor assigned: 05-May-2022, Pre QC No. JACR-22-17274(PQ); Reviewed: 20-May-2022, QC No. JACR-22-17274; Revised: 27-May-2022, Manuscript No. JACR-22-17274(R); Accepted: 06-Jun-2022 Published: 06-Jun-2022 , DOI: 10.35248/2155-6148.22.13.1060
Copyright: © 2022 Kalu UM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.