Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research Article - (2015) Volume 5, Issue 1
The population of the world is aging rapidly, because of increasing life expectancy and falling birth rates This age is also more prone to have chronic diseases and hence there is a need to ensure that the health and social support to these individuals is available. Mental illness represents an important public health problem. Local-level data concerning mental illness in different populations provides the evidence-base for public health authorities to plan, implement and evaluate control programs. Aims: to estimate the prevalence of psychiatric disorders among the elderly in this region and to analyze for differences between urban and rural areas and also identify and suggest some risk factors for these disorders. Methodology: The study was done in Zulfi region of Saudi Arabia. The sample size of rural & urban study was 550&392 persons from 65 years and more, respectively. Instruments and procedures: All the participants of the study were given a general health questionnaire, a symptom check list, a questionnaire to assess the social and economic level and a Structured clinical interview for DSM –IV (SCID) Results: The psychiatric symptoms among elderly in this study according to SCL 90 were not seen in 15.56% in urban people and 40.4% in rural area. The most prevalent psychiatric disorder in urban area is dysthymia 19.37% while the most prevalent psychiatric disorder in rural area is adjustment disorder with depressed mood at 14%.
<Keywords: Psychiatric morbidity; Geriatric; Rural; Urban
The global population is aging rapidly, this is due to increasing life expectancy and falling of birth rates, especially in the developed word. The world’s older population has a net increase of 1.2 million each month. It is estimated that by the year 2025 the total elderly population will be 976 million [1]. The ageing of the world’s population means that health problems associated with the elderly are becoming relatively more important. This growing group has its specific health and social problems which need to be addressed accordingly.
Old age is not a disease, It is a phase of the life cycle characterized by its own developmental issues, many of which are concerned with loss of physical agility, mental acuity, friends and loved ones, status and power [2,3]. This age is also more prone to have chronic diseases and hence, there is a need to ensure that the health and social support to these individuals is available. Mental illness represents an important public health problem. Local-level data concerning mental illness in different populations provides the evidence-base for public health authorities to plan, implement and evaluate control programs [4]. Habib et al. in 2009 reported that 45.5% of prevalence of depressive symptoms were present among Bahraini elders attending local health centers [5].
Saudi Arabia has population growth rates which rank above the general average of 2.37%, registered across the Arab world [6]. As a result of dedicated and intensive efforts towards health care issues the mortality rate has been reduced significantly resulting in increasing percentage of elderly population. Many studies have been done previously to estimate the prevalence of mental disorders with rates varying in different populations, age groups, times, and geographic locations. Psychiatric morbidity in primary care was estimated in 1995 around 30-46% of the visiting patients [7]. In 2002, depression and anxiety disorders were noted about 18% among adults in central Saudi Arabia [8]. Al Ibrahim et al., in 2010 showed an overall prevalence of 41% in a systematic review on depression [9], El Rufaie et al. in 2009 noted a 17% prevalence of depression among residents of Dammam [10]. Al Qahtani et al., in 2008 reported a 27% prevalence of depression in Asir [11]. Abdul Wahid et al. in 2011, reported an overall prevalence of depression nearing 12%, with 6% as severe cases, in the south-eastern region [12]. In Riyadh, Becker et al in 2002 and 2004, found depression prevalence to be 20% in primary care settings [13].
As very few studies have focused on the elderly population [14,15], there is a lacuna in data of mental disorders in elderly in Zulfi region. This study was designed to estimate and compare the prevalence of psychiatric disorders among the elderly between urban and rural areas and also identify some risk factors for these disorders.
This study was conducted from October 2012 until October 2013. It was designed as a population based cross-sectional study, in which the city of Zulfi was taken as the urban population and Al-Artaweyah region near Zulfi which is a rural community, represented rural sample. Medical and Dental students of our university were trained regarding the General Health Questionnaires (GHQ) and symptom check list (SCL 90) and these students were instructed to interact with elderly individuals in their respective areas. The data was collected by systematic random sampling technique, 1000 questionnaires were distributed out of which 950 were returned, 58 forms were rejected as they were incomplete. The individuals who rejected the interview or had severe medical or mental illness such as personality disorders, mental retardation etc. which interfered with communication was excluded from the study. Finally a total of 892 elderly of 65 years and older formed the sample size. 392 respondents (262 males &130 females) formed the urban sample, while rural sample consisted of 500 respondents (278 males & 222 females).
All 892 elderly subjects with scores above cut off point –7 in GHQ and SCL 90 were interviewed with structured clinical interview for DSM –IV to diagnose the disorders. The data was entered and analyzed using SPSS 22.0. Mean + S.D was reported for quantitative variables. Frequencies and percentages were reported for qualitative variables. Two independent sample t test was applied to compare group mean differences. ANCOVA was applied to compare group means and interaction effects. A p-value of <0.05 was considered as statistically significant.
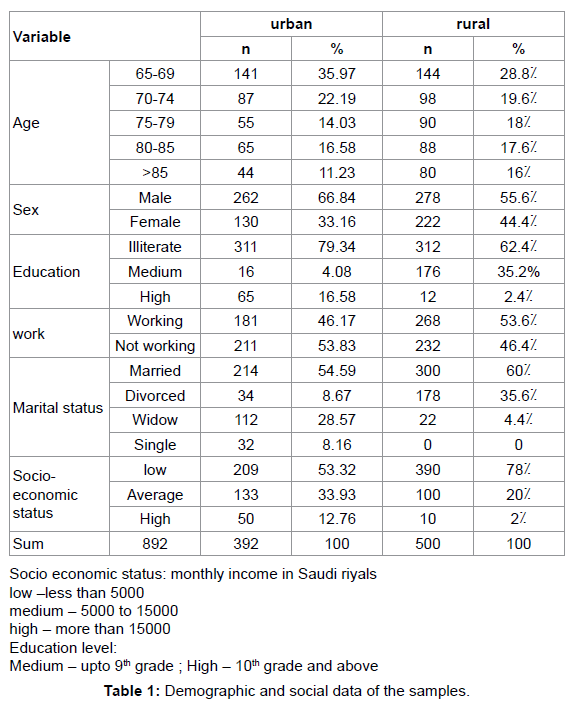
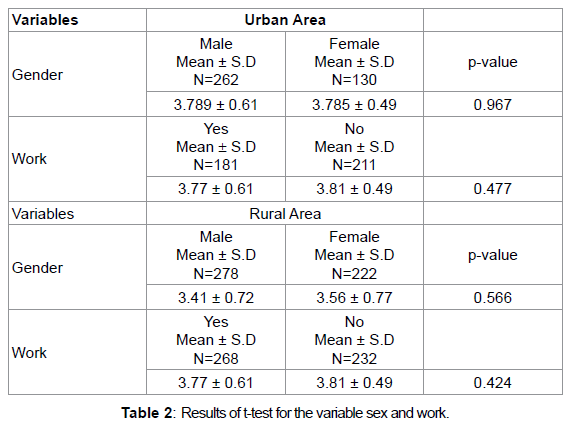
The demographic data of all 892 subjects reveals that most of the parameters for the urban and rural population are the same however the rural population has a remarkably high percentage of divorcees (35.6%) and the high percentage of low socio economic group (79.2%) (Table 1). However the results of covariance and t test analysis revealed that there are no statistically significant differences between the prevalence of mental disorders among the two groups regarding to the variables such as age, education level, marital status, monthly income, age and gender (Table 2).
The GHQ scores were positive for a high percentage of population (79.2%) in rural population as compared to urban (64.54%).
72.07% of the total sample was positive for presence psychiatric symptoms. A high percentage of population (40%) in the rural sample shows no symptoms of psychiatric disorders as compared to 15.56% of urban. Somatization symtom was the most common in rural group (28%) whereas the depressive symptom was common in urban (15.56%) (Table 3).
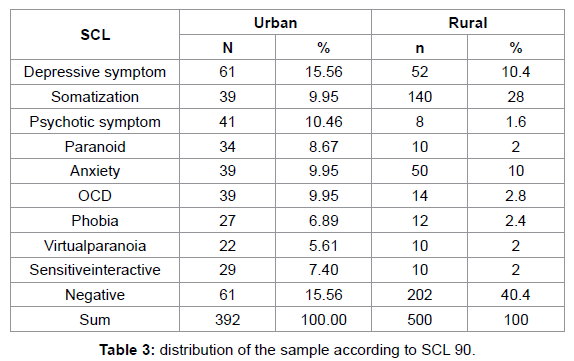
Psychotic symptoms and paranoid are more in urban population as compared to the rural sample.
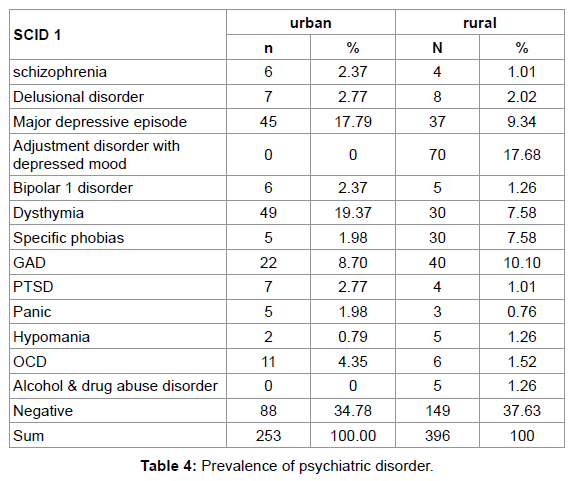
According to SCID, dysthymia was the most found disorder in the urban group (19.37%) whereas in rural sample it was adjustment disorder with depressed mood at 14%. Major depressive episode and OCD were more in the urban population at 17.79% and 4.35% than in the rural population; specific phobias were more in the rural group than in the urban group (Table 4).
This study showed that the rural population had more percentage of people who were negative for prevalence of mental disorders than the urban population. This was consistent with similar studies done earlier [16], this difference could be due to the variation in lifestyle, social and cultural settings. The demographic data obtained from the study shows that the rural population had more percentage of people of more than 85 years of age; this can be correlated to the less prevalence of mental disorders in this group and overall healthy living habits seen in rural areas. The socioeconomic status of the rural group shows 78% of the population is in low status and this is consistent with earlier studies [17] which show less prevalence of psychiatric disorders in lower socioeconomic status group. The urban group had 8.67% of people who were divorced but the rural population had a considerably high percentage of people 35.6% who were divorced. This finding is not consistent with earlier studies like M. Mohammadi et al. [16] which have reported that married individuals are less likely to have psychiatric disorders as compared to single and divorced individuals, whereas in our study the rural group which has a high percentage of divorcees also shows less prevalence of psychiatric disorders. Although the differences mentioned above were not statistically significant, there was a large variation in the distribution of psychiatric disorders between the urban and rural groups. This is an interesting finding and it needs to be studied in detail. the lack of statistical significance could be due to small size of sample or could be due to some hidden bias in the sample selection.
Depression was the most common symptom in urban population and was more than that seen in rural group, This was consistent with studies like Al Sehri et al. [18] which have shown that depression is less prevalent is rural population. Anxiety was seen in both the population groups in similar percentage of people (9.95% and 10%), this was considerably less than that seen in previous studies.
Many differences are seen between the urban and rural group in their demographic and social data with respect to the education level, marital status, socio-economic status etc., which is reflected in the difference in prevalence of various psychiatric disorders in the two groups hence these variables could be the possible risk factors in development of psychiatric disorders in elderly and need to be further evaluated as the lack of statistical significance could be because the sample of our study was small, the area targeted was a small region and also there could be a bias in selection of sample as the initial data was collected by medical and dental students and not professionals related to psychiatry. These limitations could also explain the high prevalence of psychiatric symptoms when compared to previously mentioned studies, in spite of this we have obtained a valuable data on the mental disorders in the elderly.
This data shows that the elderly population has more symptoms of psychiatric disorders hence more care should be taken of this population group.
As elderly persons are less likely to seek medical help, more home surveys and camps should be conducted to evaluate the elderly. This data could also be used by the mobile medical units of the university to deliver psychiatric care and implement preventive strategies.
To conduct a more extensive research by psychologists and social workers, with a larger sample size, use of specific scales to detect individual disorders like Hamilton scale for depression, to also correlate with co morbid conditions like diabetes, hypertension etc.
To appoint more psychiatrists in rural areas to make psychiatric care available to all elderly people.
Further investigations are needed to conduct to discuss relationship between elderly and younger population and also how socio-economic supports could the health status of the targeted population.