Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2020)Volume 9, Issue 3
Background: Postpartum family planning helps women to achieve the recommended birth interval before next pregnancy. In Ethiopia contraception use in postpartum period is only 8% while unmet need is 81% resulted in short birth interval, abortion, unplanned birth and miscarriage.
Objectives: To assess magnitude of postpartum family planning utilization and its associated factors among postpartum women who gave birth within one year prior to the study.
Methods: Community based cross-sectional study was conducted in Lode Hetosa district from July 20, 2018 to August 20, 2018. A random sample of 1162 postpartum women who gave birth within 12 months prior to study was recruited for the study. Structured and pretested questionnaire were utilized to collect the data. After entered to Epi info version 7, a cleaned data was analysed using SPSS version 21. Multivariate logistic regressions were fit to determine association between postpartum family planning utilization and independent variables.
Results: Magnitude of postpartum family planning utilization in the study area was 15%. The most frequently used family planning method within 6 weeks after delivery was implants (35%). The odds of using contraception were 2.9(95%CI: 1.41, 5.97) times higher among women whose partners completed secondary education when compared to those with no formal education. Odds of utilizing contraception were 8.27 (95%CI: 4.14, 16.52)times more likely among mothers who got FP counselling during ANC visit when compared with who didn’t get counselling during this time. Likewise, who didn’t get counselling at PNC services were 0.41(95%CI: 0.2, 0.86) times less likely used PPFP relative to who were counselled.
Conclusions: Postpartum family planning utilization was low in the district. Partner’s educational status, knowledge of mother, family planning counselling during ANC and PNC and sexual resumption were factors significantly associated with postpartum family planning utilization.
Postpartum Family Planning, Women, Associated Factors, Lode Hetosa District, Arsi zone, Ethiopia
ANC: Antenatal Care; AOR: Adjusted Odds Ratio; CI: Confidence Interval; FMOH: Federal Ministry of Health; FP: Family Planning; HEW: Health Extension Workers; HTSP: Healthy Timing and Spacing Pregnancy; IUD: Intra Uterine Device; LAM: Lactation Amenorrhea Method; MNCH: Maternal, Newborn and Child Health; OR: Odds Ratio; PHCU: Primary Health Care Unit; PNC: Postnatal Care; PPFP: Postpartum Family Planning; PP: Postpartum Period; PPIUD: Postpartum Intrauterine Device; SE: Standard Error; SPSS: Statistical Package for Social Sciences; WHO: World Health Organization
Postpartum Family Planning (PPFP) is a service delivery strategy that expands access to family planning through its integration with the existing continuum of MNCH services [1]. It’s most important role is to help a woman achieve the desired interval before the next pregnancy in order to optimize her health and that of her young children [2]. WHO recommended that after a live birth, the interval before attempting the next pregnancy is at least 24 months. This is because birth-to-pregnancy intervals of around 18 months or shorter are associated with elevated risk of infant, neonatal and perinatal mortality, low birth weight, small size for gestational age, and pre-term delivery [3]. However, worldwide even though more than 9 out of 10 women want to avoid pregnancy for 2 years after having had a baby, 1 in 7 of them is not using contraception [4].
It is very true that women can get pregnant before the return of menses if they resume sexual intercourse early [5]. In general, women resume pregnancy risk from 4-6 weeks postpartum. Hence, effective contraception method must be available to assist women in reaching recommended inter pregnancy intervals [2,6].
The timing of PPFP was defined programmatically in different ways such as post placental (10 minute after placental delivery), immediate postpartum (within 48 hours after delivery), early postpartum (48 hours up to 6 weeks after delivery) and extended postpartum representing (six weeks to one year) [7].
According to recent (2016) guideline of Communicable Disease Control Medical Eligibility Criteria (CDCMEC) for less than 30 days postpartum period; Implant, Depo Provera, and Progestin Only Pill are category 2 options. But for greater than 30 days postpartum there is no restriction for the use of these contraceptive methods [8].
There are about 75 million unintended pregnancies every year in the world which place women at greater risk of maternal death and disability [9]. In Africa 49.1 million women became pregnant annually of which 39% are unintended resulted in abortion (48%), unplanned births (38%) and miscarriage (13%). Majority (82%) of all unintended pregnancies occurred among women using traditional or no contraception [10]. In Ethiopia 101 unplanned pregnancies happened per 1000 women which constituted 42% of all pregnancies. Unsurprisingly, the vast majority of unintended pregnancies (95%) occur among the women who do not practice contraception at all [11, 12]. Especially, in the first year postpartum at least 70% of pregnancies are unwanted [13].
In 2015 globally 12% of married or in-union women are estimated to have had an unmet need for PPFP. Sub-Saharan Africa is the region where the level doubles (24%) and greater magnitude of unmet need (26.3%) seen in Ethiopia [14, 15]. Married women in general population those in first year postpartum are less likely using family planning and can be considered as unreached critical populations [16]. If all unmet need for contraception were met, 104,000 maternal deaths would be prevented each year mainly in sub-Saharan Africa [15]. Postpartum family planning is one of the highest impact interventions to address the unmet need [17]. To effectively address this unmet need, it is important to uniquely focus on issue of integrating the service to MNCH services [18, 19].
Federal Ministry of Health of Ethiopia (FMOH) set a target to meet need of immediate postpartum contraception use, 100% by 2020 through applying strategy set for this issue: increasing access, creating demand, improving utilization of quality family planning services and scale up immediate postpartum service to all districts [20]. Despite this strategy, studies conducted on PPFP utilization so far showed very low utilization level of PPFP in the country. Study conducted in six low and middle income countries showed total unmet need for PPFP service in Ethiopia is 81% [21]. Other study conducted using data from 2016 EDHS in Ethiopia also showed PPFP utilization at 1 month, 3 months, 6 months, 9 months and 12 months postpartum are 8%, 16%, 21%, 24% and 26% respectively [22].
The reasons for unplanned pregnancy within a year of after birth may be diverse. Even though ovulation can occur as early as 25 days from last birth, around a quarter of women (23%) will have started having sex before 6 weeks, which is before a postnatal check is scheduled where contraception is generally discussed [13, 23].
To our best knowledge, there is very limited data on PPFP utilization in the country, particularly in Lode Hetosa district. Therefore it is quite important to assess magnitude of PPFP utilization and associated factors among women who gave birth in the last 12 months prior to the study in Lode Hetosa District, south east Ethiopia. The finding from this study will be helpful for women in the general population, policy makers, partners working on maternal, new-born and child health, health workers and other stakeholders to address the problem of low utilization of PPFP (Figure 1).
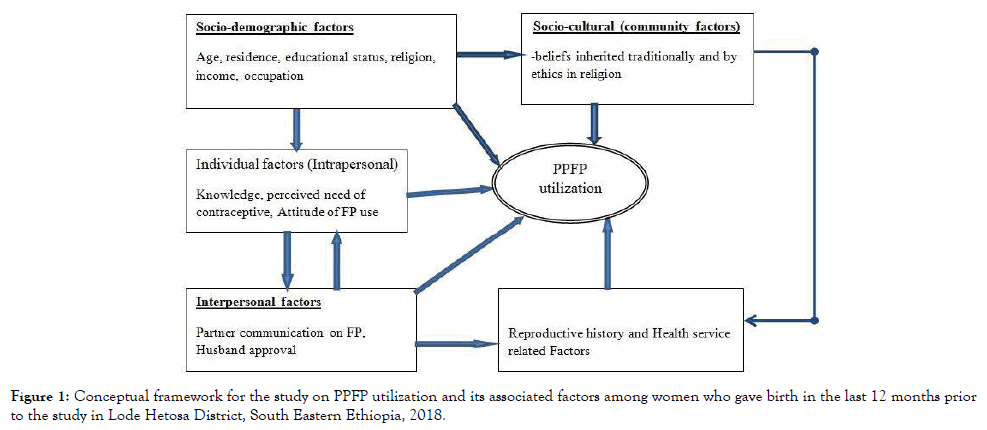
Figure 1. Conceptual framework for the study on PPFP utilization and its associated factors among women who gave birth in the last 12 months prior to the study in Lode Hetosa District, South Eastern Ethiopia, 2018.
Study area and period
The study was conducted from July 20, 2018 to August 20, 2018 in Lode Hetosa district, South East Ethiopia. The district has 23 kebeles (the lowest administrative structure in the country) of which 19 are rural kebeles and the rest are urban-based. The capital town of the district, Huruta, is located at 164 km from Addis Ababa (towards the East). According to information obtained from the district’s Health Office, a total of 146,634 people are living in the district in 2018. Number of child bearing women, under one year infants and total live births are estimated to be 28,447(19.4%), 4717(3.2%),5088(3.45%)respectively. There are four functional governmental health centers, 19 health posts, 12 private clinics and 5 drug stores in the district. All governmental health facilities and private clinics are providing family planning service.
Study design
Community based cross sectional study design was used.
Source population
All postpartum women who gave birth within 12 months prior to the study period in Lode Hetosa district were the source population for the study.
Study population
All postpartum women in selected kebeles who gave birth within 12 months prior to the study period in Lode Hetosa district were included in to the study.
Sample size determination
Sample size was estimated using single population proportion formula (n = ((Zα/2)2 P (1-p))/d2). Proportions of PPFP utilization of 10.2% from previous similar study done in Ethiopia were used [24]. Other similar studies reviewed were also reviewed but the above mentioned proportion could give maximum sample size. A margin error of 2.2%, 95% CI (z=1.96), 10% non-response rate and 1.5 design effect was also used to determine the estimated sample size. Hence, the calculated sample size was 1199.
For qualitative part two focus group discussions (FGD) were carried out. Each had 12 individuals; 4 midwife providing the service, 4 primary health care directors (each from the four health centres in the district) and 4 experts from district health office. The second included FGD had 12 women development army (WDA).
Sampling procedure
For quantitative part, 23 kebeles in the district were stratified in to Rural and urban assuming that there could be a difference among them with regards to PPFP utilization. According to information received from Lode Hetosa Woreda Health Office there were about 2647 postpartum women who had given birth within one year (July, 2017 to June 2018). Therefore, the average number of postpartum women per kebele was expected to be about 115. Hence, we randomly selected 10 kebeles (2 from urban 8 from rural) (Figure 2). For qualitative approach participants were selected purposely.
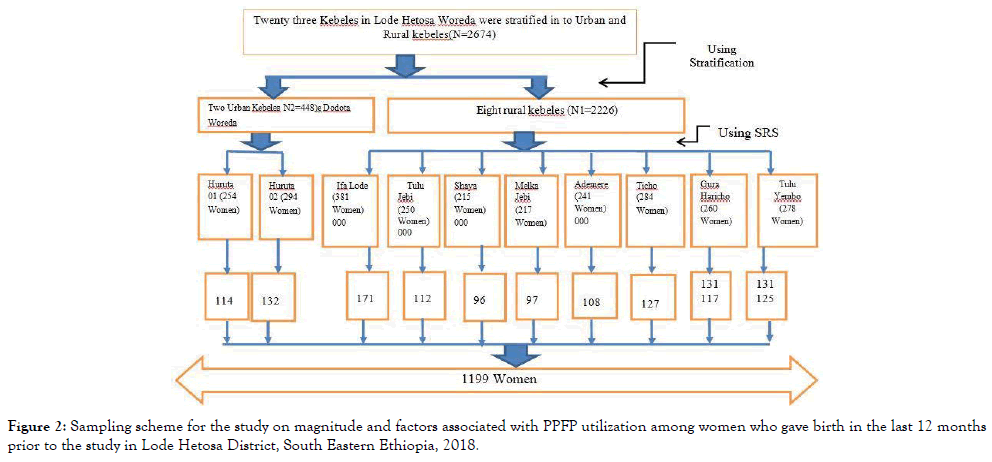
Figure 2. Sampling scheme for the study on magnitude and factors associated with PPFP utilization among women who gave birth in the last 12 months prior to the study in Lode Hetosa District, South Eastern Ethiopia, 2018.
Data collection
Quantitative data was collected using structured and pretested questionnaire via face to face interview at participant’s home. Tools were first prepared in English and translated to Afan Oromo version (local language) then translated back to English to ensure accuracy. All the ten data collectors recruited were experienced health professionals fluent in the local language. They received 3 days training on the study purpose, questionnaire, and ethical issues. Mock interviews were used to test inter-rater reliability. Two field supervisor were assigned supervise quality of data collection by observing interviews and checking completed questionnaire. Data collectors were asked to make corrections when errors were found.
In order to identify eligible women, data collectors first attempted to get a list of postpartum women from health posts in the selected kebeles. But it was totally impossible to get up to date list. Hence HEWs and kebele chairpersons helped identify local guides who would know which households had postpartum women. Interviewed women were also asked if they knew of other postpartum women.
For qualitative approach check list was used to guide the FGD and facilitated by two health professionals who were already recruited to supervise quantitative data collection under close monitoring by principal investigator. The discussions were under gone for 60 to 90 minutes.
Study variables
Dependent variable: Postpartum family planning utilization.
Independent variable: The independent variables were sociodemographic variables (age, residence, occupation, income, religion, marital status, woman’s educational level, partner’s educational level and ethnicity), number of live children, knowledge on PPFP, attitude toward PPFP, perceived need of contraception, husband approval of family planning, partner discussion on family planning, prior use of contraception, having ANC & PNC care, place of delivery, menses return , resumption of sexual activity, counselling on family planning during ANC, delivery & PNC, fertility desire, previous health outcome experience from family planning and others.
Data processing and analysis
The data was coded and entered in to Epi info version 7 and exported to SPSS version 21 for analysis. Descriptive statistics was performed to characterize the study population by independent variables using frequency and proportions. Bivariate logistic regression was fitted to select candidate variables for further analysis and those whose P-value less than or equal to 0.25 were remained in the multivariate logistic regression analysis. Odds Ratios was calculated for each variable and the independence of any association was controlled by entering all variables into the model using backward stepwise method (backward conditional). The magnitude of the association between PPFP utilization and independent variables was measured using adjusted odds ratios (AOR) and 95% confidence interval (CI) and P- values below 0.05 was considered statistically significant.
Operational definitions
Postpartum family planning utilization: In this study utilization of modern family planning methods within six weeks after delivery was considered as PPF utilization. For these purpose women who gave birth 12 months before the survey were interviewed.
Knowledge of PPFP methods: For this particular study, knowledge was assessed by six item questions adapted from study conducted in Somali region with little modification [25]. Total score was 10. The second and fifth item had 3 score each while others had only 1 score each. For questions which consisted 3 scores number of correct answers would be number of scores given with exception of only 3 scores for who responded even greater than 3 right answers. Those who scored 5 and above were taken as have good knowledge to PPFP and who answer 4 and below were taken as poor knowledge.
Attitude for FP: Items used to measure attitude of postpartum women regarding PPFP was adapted from previous study with few modifications [25]. Ten items were used to measure the opinion of respondents using likert scale of five categories. Assumptions for scoring items were given by scoring rule. For items with negative connotations that triggering a disagreement response if there was favourable influence; scores of 5=for strongly agree,4=for agree,3=for uncertain,2=for disagree and 1=for strongly disagree was given. But for items with positive connotations that triggering agreement response if there was favourable influences; scores of 1=for strongly agree,2=for agree,3=for uncertain,4=for disagree and 5=for strongly disagree was given. Therefore it followed from the assumption that the lower the score the greater favourable attitude was, and vice versa. Then total scores were categorized in to cut-off values of 10-29, 30 and 31-50 for favourable, neutral and unfavourable attitude respectively.
Socio-cultural influence
This part was measured by 3 items with positive connotations that triggering positive response if there was favourable socio-cultural influence. If answer was positive (yes) for all items it was classified as favourable influence while as unfavourable socio-cultural influence if negative (no) would be responded for one or more items.
Socio-demographic characteristics of the participated women
The totals of 1160 postpartum women were interviewed making response rate of 96.7%. Mean age of respondents was 29 years with minimum and maximum of 17 years and 45 years respectively. More than one third, 399(34.4%), of study participants were in age group of 25-29 years. With regards to marital status, most of them 999(86.1%) were married and living with their husband. About half, 562(48.4%), of the participants were Orthodox followed by Muslim 366 (31.6%). Dominant ethnic group were Oromo 791 (68.2%). More than half, 667 (57.5%), of the participants had no formal education (Table 1).
| Variables | Frequency | Percent |
|---|---|---|
| Age of respondents (n=1160) | ||
| 15-19 years | 56 | 4.8 |
| 20-24 years | 198 | 17.1 |
| 25-29 years | 399 | 34.4 |
| 30-34 years | 266 | 22.9 |
| 35-39 years | 169 | 14.6 |
| 40-49 years | 72 | 6.2 |
| Marital status (n=1160) | ||
| Married | 999 | 86.1 |
| Single | 73 | 6.3 |
| Divorced | 40 | 3.4 |
| Widowed | 32 | 2.8 |
| Separated | 16 | 1.4 |
| Religion (n=1160) | ||
| Muslim | 366 | 31.6 |
| Orthodox | 562 | 48.4 |
| Protestant | 200 | 17.2 |
| Catholic | 16 | 1.4 |
| Others | 16 | 1.4 |
| Mother educational status (n=1160) | ||
| Tertiary education | 40 | 3.4 |
| Secondary education | 136 | 11.7 |
| Primary education | 317 | 27.3 |
| No formal education | 667 | 57.5 |
| Occupation (n=1160) | ||
| Farmer | 600 | 51.7 |
| Merchant | 344 | 29.7 |
| Salaried worker (public) | 72 | 6.2 |
| Student | 56 | 4.8 |
| Unemployed | 40 | 3.4 |
| Salaried worker (private) | 24 | 2.1 |
| Others | 24 | 2.1 |
| Ethnicity (n=1160) | ||
| Oromo | 791 | 68.2 |
| Ahmara | 273 | 23.5 |
| Guragie | 80 | 6.9 |
| Tigrae | 16 | 1.4 |
| Residence (n=1160) | ||
| Rural | 918 | 79.1 |
| Urban | 242 | 20.9 |
| Family income (n=1160) | ||
| 350-1000ETB | 385 | 33.2 |
| 1001-1599ETB | 288 | 24.8 |
| 1600-2999 | 255 | 22 |
| 3000ETB and Above | 232 | 20 |
| Partner educational status (n=1160) | ||
| Tertiary education | 190 | 16.4 |
| Secondary education | 345 | 29.7 |
| Primary education | 367 | 31.6 |
| No formal education | 258 | 22.2 |
Table 1: Socio-demographic characteristics of postpartum women who gave birth within 12 months prior to the survey in Lode Hetosa district, south east Ethiopia 2018.
Knowledge of women about postpartum family planning
About half, 607(52.3%) of women had awareness on types of family planning methods used during postpartum period. The majority ,872(75.2%) ,of them knew that using contraception is important to limit number of children but only 350(30.1%) knew about healthy timing and spacing of pregnancy. Generally 624(54%) had good knowledge while the rest had poor knowledge as summarized as per the operational definition used for this purpose (Table 2).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Women knew PPFP methods | Yes | 607 | 52.3 |
| Mentioned PPFP method by women during survey | Injectable | 304 | 26.2 |
| Pills | 280 | 24.1 | |
| implants | 144 | 12.4 | |
| IUCD | 48 | 4.1 | |
| LAM | 24 | 2 | |
| Condom | 8 | 0.7 | |
| Benefits of PPFP methods mentioned women during survey | Prevent unwanted pregnancy | 801 | 69.1 |
| Limit number of children | 872 | 75.2 | |
| Healthy timing and Space pregnancy | 349 | 30.1 | |
| Have no any advantage | 16 | 1.4 | |
| I don’t know | 80 | 6.9 | |
| Do you know side effects of contraceptive methods? | Yes | 400 | 34.5 |
| Side effects mentioned by women during the survey | Back pain | 136 | 11.7 |
| Headache | 72 | 6.2 | |
| Abdominal pain | 49 | 4.2 | |
| Heavy vaginal bleeding | 40 | 3.4 | |
| Weight gain | 32 | 2.7 | |
| Prolonged vaginal bleeding | 25 | 2.1 | |
| Weakness | 23 | 0.19 | |
| Discoloration of face | 7 | 0.6 | |
| After stopping contraceptive use can fertility resume? | Yes | 1081 | 93.2 |
| No | 21 | 1.8 | |
| I don’t know | 58 | 5 | |
| Knowledge(Summary) | Good knowledge | 624 | 54 |
| Poor knowledge | 536 | 46 | |
Table 2: Knowledge of women about postpartum family planning postpartum in Lode Hetosa district, South east Ethiopia 2018.
Attitude of women toward postpartum contraceptive use
Among all respondents 552(47.6%) agreed that PPFP utilization is necessary for health of both mothers and their children. Women who had favourable attitude toward utilization of postpartum family planning were 951(82%) while only 80(7%) had unfavourable attitude. The rest 129(11%) had neutral attitude (Table 3).
| Variable | Strongly disagree n(%) | Disagree n(%) | Neutral n(%) | Agree n(%) | Strongly Agree n(%) |
|---|---|---|---|---|---|
| Discussing PPFP use with partner is good | 24(2.1) | 72(6.2) | 449(38.7) | 519(44.7) | 96(8.3) |
| Using postpartum contraceptive is shame | 136(11.7) | 607(52.3) | 353(30.4) | 56(4.8) | 8(0.7) |
| PPFP is good for mother and child health | 0 | 62(5.3) | 458(39.5) | 552(47.6) | 88(7.6) |
| Small family size makes family happy | 16(1.4) | 78(6.7) | 320(27.6) | 666(57.4) | 80(6.9) |
| PPFP use good for standard of living | 8(0.7) | 62(5.3) | 280(24.1) | 714(61.6) | 96(8.3) |
| Exclusive BF used to prevent pregnancy | 24(2.1) | 128(11.0) | 374(32.2) | 594(51.2) | 40(3.4) |
| Unmarried women can use contraceptive | 40(3.4) | 134(11.6) | 400(34.5) | 570(49.1) | 16(1.4) |
| Using Contraceptive can cause infertility | 104(9.0) | 536(46.2) | 392(33.8) | 128(11.0) | 0 |
| Utilization of condom is shame | 120(10.3) | 576(49.7) | 280(24.1) | 184(15.9) | 0 |
| Risk of using FP is higher than its benefit | 72(6.2) | 680(58.6) | 296(25.5) | 104(9.0) | 8(0.7) |
| Attitude | Favorable | 911 | 78.5 | ||
| Neutral | 128 | 11 | |||
| Unfavorable | 121 | 10.5 | |||
Table 3: Attitude of women toward postpartum family planning utilization in Lode Hetosa district, south east Ethiopia 2018.
Postpartum family planning utilization
About half, 576 (49.7%), of women who gave birth within 12 months prior to this survey were using family planning method during the survey. Of these only 73(12.7%) started using family planning within the first 48 hours and 101(17.5%) started immediately after 48 hours to 6 weeks after delivery. Majority of them, 402(69.8%) started using after 6 weeks. This showed only 174(15%) of women who gave birth in 12 months before this survey were using family planning method with in the 6 weeks of postpartum (Table 4).
| Time after delivery when FP use started | Frequency | Percent |
|---|---|---|
| Within 48 hours | 73 | 12.7 |
| 48hours to 6 weeks | 101 | 17.5 |
| Six weeks to 3 months | 123 | 21.4 |
| Four-six months | 130 | 22.6 |
| Seven to nine months | 120 | 20.8 |
| Ten to twelve months | 29 | 5 |
| Total | 576 | 100 |
Table 4: Timing of PPFP among women who gave birth within 12 months prior to the survey in Lode Hetosa district, south east Ethiopia 2018.
The most utilized family planning method with in the 6 weeks after delivery implant 61(35%) followed by LAM 47(27%) while condom and sterilization were not utilized in this period (Figure 3).
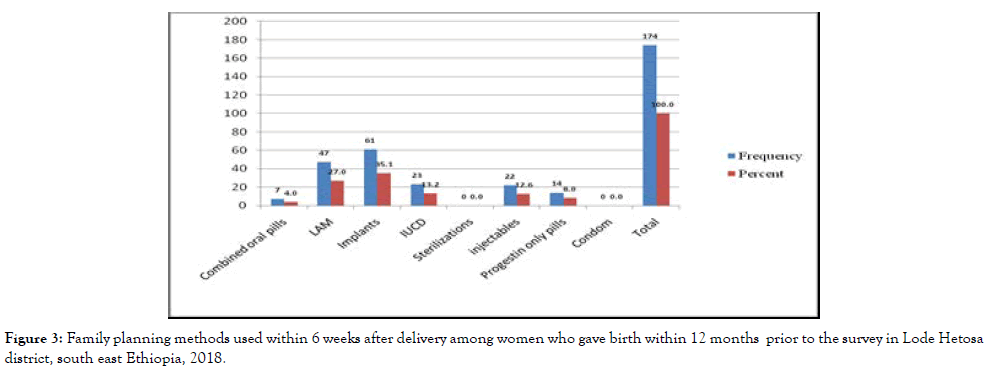
Figure 3. Family planning methods used within 6 weeks after delivery among women who gave birth within 12 months prior to the survey in Lode Hetosa district, south east Ethiopia, 2018.
This finding was supported by FGD undergone with health workers where it was stated that relatively the most preferred method by postpartum women was implant. One midwife from Huruta health center said “After receiving proper counseling especially on utilization of long acting family planning like tubal ligation (sterilization), postpartum women usually choose implants. Also with regards to IUCD there is a misconception that it can harm their uterus and make them infertile”.
Reproductive history and health service related characters of women
About 164(14%) of the women resumed sexual activity within 6 weeks after delivery while 628(67.6%) of them resumed with 6 weeks to 3 months after delivery. Menses was returned on 608(52.4%) of the interviewed women of which 30(5.2%) was before 6 weeks of delivery and 576(94.8%) was after 6 weeks of delivery. But Family planning counseling during ANC, delivery and PNC were 592(51%), 520(44.8%) and 384(33.2%) respectively (Table 5).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Maternal services received in the last 12 months(n=520) | ANC visit | 935 | 80.6 |
| PNC service | 520 | 44.8 | |
| Place of delivery in the last 12 months(n=520) | Government facility | 909 | 78.4 |
| Private facility | 69 | 5.9 | |
| Home | 182 | 15.7 | |
| Timings of PNC(n=520) | Less than 1 day | 248 | 47.8 |
| In 1-2 days | 120 | 23 | |
| 3 days and after | 152 | 29.2 | |
| Counseling received in the 12 months | during ANC | 592 | 51 |
| during delivery | 520 | 44.8 | |
| during PNC service | 384 | 33.2 | |
| Number of live children in the family | 1 | 192 | 16.6 |
| 02-Mar | 775 | 66.8 | |
| 4 and above | 192 | 16.6 | |
| Desire for more children | Yes | 753 | 64.9 |
| Prior use of contraception | Yes | 708 | 61 |
| Prior experience of side effects(n=708) | Yes | 222 | 31.3 |
| Timing of sexual resumption(n=928) | before six weeks | 164 | 17.6 |
| six weeks-3 months | 628 | 67.6 | |
| four - 6 months | 128 | 13.8 | |
| ten - 12 months | 8 | 1 | |
| Menses return | Yes | 608 | 52.4 |
| Time when menses return(n=608) | At or before 6 weeks after delivery | 32 | 5.2 |
| After 6 weeks | 576 | 94.8 | |
| Duration of amenorrhea(n=608) | four weeks - 3 months | 288 | 47.4 |
| four to 6 months | 256 | 42.1 | |
| seven to 9 months | 56 | 9.2 | |
| ten to 12 months | 8 | 1.3 | |
| Availability of family planning methods at nearest health facility | always available | 504 | 43.4 |
| sometimes shortage seen | 278 | 23.9 | |
| Always not available | 26 | 2.2 | |
| I don't know | 352 | 30.5 | |
Table 5: Reproductive history and health service related characteristics of postpartum women who gave birth within 12 months prior to the survey in Lode Hetosa district, south east Ethiopia, 2018.
Discussion on Family planning during postpartum period
Two hundred and forty eight (21.4%) of the respondents didn’t discussed about family planning utilization with their husband and 289(25%) of husbands didn’t allow their wife to use family planning methods. The majority are supporting their wife to use family planning methods through provision of transports fee, reminding dates of appointment give items or finances and use condom as one of family planning methods.
Socio-cultural characteristics of respondents
About 3 in 4 women had favourable socio cultural conditions while only 24.2% experienced unfavourable community level conditions like religion, culture and influence from neighbour in different ways.
Factors associated to postpartum family planning utilization
In multiple logistic regression analysis partner educational status, FP counselling during ANC and PNC, sexual resumption, and knowledge of women about PPFP were significantly associated with postpartum family planning utilization (Table 6).
| Variables | PPFP Utilization | COR(95%CI) | AOR(95% CI) | P-Value | ||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Mother's educational status | Tertiary | 15 | 25 | 2.21(1.03,4.73) | 1.37(0.61,3.07) | 0.135 |
| Secondary | 29 | 107 | 2.57(1.27,5.17) | 0.47(0.20,1.12) | 0.091 | |
| Primary | 60 | 257 | 5.11(2.57,10.16 | 0.48(0.18,1.25) | 0,135 | |
| No formal education | 70 | 597 | 1 | 1 | ||
| Residence | Urban | 50 | 192 | 3.84(1.16,2.42) | 0.88(0.50,1.54) | 1.663 |
| Rural | 124 | 794 | 1 | 1 | ||
| Partner's educational status | Tertiary education | 66 | 124 | 2.51(1.62,3.90) | 0.84(0.47,1.52) | 0.57 |
| Secondary education | 46 | 299 | 10.95(6.19,19.3 | 2.9(1.41,5.97)* | 0.004 | |
| Primary education | 17 | 350 | 3.46(2.24,5.32) | 1.11(0.62,1.97) | 0.72 | |
| No formal education | 45 | 213 | 1 | 1 | ||
| Knowledge | Poor knowledge | 23 | 513 | 0.14(0.08,0.22) | 0.17(0.10,0.31)* | 0.001 |
| Good knowledge | 151 | 473 | 1 | 1 | ||
| Attitude | Favorable attitude | 148 | 763 | 1.11(.65,1.88) | 0.48(0.23,1.01) | 0.054 |
| Neutral | 8 | 120 | 2.91(1.39,6.08) | 0.92(0.34,2.47) | 0.87 | |
| Unfavorable attitude | 18 | 103 | 1 | 1 | ||
| ANC attendance | Yes | 157 | 778 | 2.46(1.46,4.16) | 0.59(0.26,1.31) | 0.19 |
| No | 17 | 208 | 1 | 1 | ||
| Place of delivery | Government facility | 163 | 746 | 5.46(2.51,11.84 | 2.56(0.92,.7.17) | 0.072 |
| Private facility | 4 | 65 | 3.55(1.27,9.88) | 2.55(0.78,8.27) | 0.118 | |
| Home | 7 | 175 | 1 | 1 | ||
| PNC service | Yes | 132 | 388 | 4.84(3.34,7.01) | 1.28(0.59,2.77) | 0.53 |
| No | 42 | 598 | 1 | 1 | ||
| FP counseling at ANC | Yes | 161 | 431 | 15.94(8.93,28.4 | 8.27(4.14,16.5)* | 0.001 |
| No | 13 | 555 | 1 | 1 | ||
| FP counseling during PNC | No | 45 | 731 | 0.12(0.08,0.17) | 0.41(0.2,0.86)* | 0.02 |
| Yes | 129 | 255 | 1 | 1 | ||
| Prior use of Contraception | Yes | 143 | 565 | 3.43(2.28,5.17) | 0.82(0.46,1.47) | 0.52 |
| No | 31 | 421 | 1 | 1 | ||
| Resumption of sexual activity | Yes | 34 | 130 | 1.59(1.05,2.42) | 1.99(1.06,3.73)* | 0.031 |
| No | 140 | 856 | 1 | 1 | ||
| Couple discussion on FP | Yes | 168 | 744 | 9.10(3.98,20.82 | 3.13(0.76,12.76 | 0.112 |
| No | 6 | 242 | 1 | 1 | ||
| Husband approval of FP use | Yes | 167 | 704 | 4.96(2.77,8.87) | 1.11(0.38,3.22) | 0.84 |
| No | 7 | 282 | 1 | 1 | ||
| Socio cultural influence | Favorable | 157 | 723 | 3.35(1.99,5.65) | 1.65(0.86,3.16) | 0.13 |
| Unfavorable | 17 | 263 | 1 | 1 | ||
| Note: *statistically significant at P value <0.05 | ||||||
Table 6: Bivariate and multiple logistic regression analysis of factors associated with PPFP utilization postpartum women who gave birth within 12 months prior to the survey in Lode Hetosa district, south east Ethiopia, 2018.
Accordingly, the odds of using contraception were 2.9(95%CI: 1.41, 5.97) times higher among women whose their partners completed secondary education when compared to those with no formal education. These findings were supported with FGD conducted among health workers. Example, as stated during discussion with health workers the primary health care unit director of Ligaba health center (one of health center in the district) said “Well educated partners usually accompany their wife during ANC and delivery; when we told them about utilization of family planning in postpartum period they better agree and influence their wife to practice it relative to illiterate partners”.
In addition, the odds of utilizing contraception were 8.27(95%CI: 4.14, 16.52) times more likely among mothers who got FP counseling during ANC visit when compared their counterpart. Likewise, the odd of using family planning in women who didn’t get counseling during PNC services were 0.41(95%CI: 0.2, 0.86) times less likely used PPFP. This finding was also supported by another FGD conducted with women. It was mentioned that there were missed opportunities for family planning counseling during ANC, delivery service and PNC which in turn affect PPFP utilization. A women who gave birth 3 months before the study period said “What I know about contraception up to today is a woman can’t start family planning use before her menses return. Even though I attended ANC and gave birth at Lode Jimata health center (another health center in the distric), I didn’t get any advice on necessity of using family planning even before 6 weeks after delivery. If I were told about it I would use the service”.
Furthermore, women who resumed sexual activity were 1.99(95%CI: 1.06, 3.73) times more likely utilized contraception in postpartum period when compared with those who didn’t resume. This finding was also supported by FGD conducted with health workers. A midwife from Lode Jimata health center said “Both in Orthodox and Muslim religions sexual activity is not allowed in at least for 40 days after delivery. Even if we told postpartum mothers to use PPFP, they usually refuse stating that they might utilize only at time of sexual resumption”.
In addition FGD conducted with health workers also indicated that some women who attended ANC at health facility might not receive counselling on PPFP due to work load, shortage of trained man power and low attention. For instance, a midwife from Huruta health center (another health center in Lode Hetosa district) said “I received in-service training on PPFP. Unless I become over loaded as a result of high client flow, I usually try to provide counselling on this service. But clinical nurses were not trained. Therefore, when trained workers are not present for various reasons, untrained one who should be assigned instead are not giving proper counselling on PPFP. This contributed to low PPFP utilization”.
Continuum of points of contact within the health care system can provide opportunity to increase level of PPFP utilization through integration of it to maternal, newborn and child health [17]. But this finding revealed that magnitude of PPFP utilization in the first 6 weeks of postpartum was only 15% which is almost similar with findings of studies previously conducted in rural Bareilly district of India(13.8%), Kebrebyan of Somali region(12.3% ) and in Dabat of Ahmara region(10.3%) [25,26,27]. But it was lower than level had been seen from studies conducted in Axum town (48%), Gonder town (48.4%), and Gozamen district of east Gojjam (21% ) [24,28,29]. The possible explanation for the differences might be due to difference in study area and target populations. Our study was conducted mainly in rural kebeles where lack of information, low educational status, socio-cultural problems and lack of transportation facilities might be a reason for less utilization of PPFP compared to studies mentioned above as they were conducted in the town.
Our study also showed partner’s education was significantly associated with postpartum family planning utilization. This was in line with community based study conducted in rural district, Dabat which revealed women whose husband had secondary and above educational status were 2.98 times higher in utilization of the service [27]. This might be due to the fact that as a partner gets a better education, he can obtain better knowledge on importance of men involvement in family planning and can help his wife to utilize contraception.
In our study, knowledge of women about PPFP was also another factors significantly associated to its utilization. This finding was consistent with similar district level community based study done in Gozamen district of East Gojjam Zone that reported strong association between women’s knowledge about PPFP ant its utilization [28]. This could be due to a woman who had good knowledge about healthy timing and spacing of pregnancy can better use PPFP when compared with their counterparts.
The current study also confirmed statistically significant difference in utilization of PPFP among women who received counselling on PPFP at ANC and PNC compared to those who didn’t receive counselling. This finding is consistent with the studies conducted in Axum town, northern Ethiopia which showed women who received counselling on PPFP during ANC and PNC visits were about 6 times more likely used PPFP than their counterparts [29]. Likewise, a facility based study in Malawi indicated counselling on fertility issues significantly associated with PPFP utilization [30]. The possible explanation for this finding is that as women get advice on PPFP utilization at all MNCH points of contact within the health system, her awareness about the importance of the service will be improved, her motivation will be enhanced and then she will practice using the methods [17].
Furthermore, this study detected women who resumed sexual activity were 1.99 times more likely utilized contraception in postpartum period compared to those who didn’t resume. This finding was consistent with studies conducted in Axum and Debrebirhan [29,31]. This might be due to fear of pregnancy risk that led them to utilize PPFP after having sex. But the finding is inconsistent with study conducted in Ghana which reported the reverse finding [32]. The inconsistency could be due to cultural, awareness and religious difference. The findings of this study can imply that, health care workers have to provide counselling services to pregnant women so that they can uptake family planning method immediately after delivery.
Strength of the study
In this study great effort was made to use larger sample size to increase precision. In addition, both quantitative and qualitative were triangulated which can definitely improve quality of the study.
Study limitations
Quantitative data were collected only from women’s view, perspective of men was not considered except in qualitative part. Some asked information relayed on the past memory of the study participants which could have recall biases. The inherent limitation of cross-sectional study was also another limitation of this study.
Magnitude of postpartum family planning utilization in Lode Hetosa district was low. Thus most of women in postpartum period were at risk to pregnancy in short birth interval. Factors significantly associated to postpartum family planning utilization were partner’s educational status, knowledge of postpartum women concerning postpartum family planning, counselling about PPFP during antenatal visit and postnatal service and resumption of sexual activity.
All concerned stakeholders should give better attention to postpartum family planning service in the district. We recommend Arsi zonal health department and Lode Hetosa district health office to routinely provide sensitization workshop for health workers in the district focusing on PPFP counselling especially at community level to reach postpartum women in the general population. Regular monitoring and supportive supervisions on proper counselling for postpartum women in all health facilities should also get attention. Moreover, we also strongly recommend health centers in Lode Hetosa district to integrate counselling and PPFP services with all MNCH services like during ANC, delivery service, PNC and EPI. We suggest, health care workers should strongly, continuously and routinely provide counselling services to pregnant women so that they can uptake family planning method immediately after delivery.
Ethical clearance was obtained from Institutional Review Board (IRB) of Arsi University College of Health Sciences. Before data collection, women were informed about the purpose of the study, the right to refuse participation and discontinue the interview. The interviewers discussed the issue of confidentiality and obtained verbal consent from all selected women before interview started.
Data sets supporting the presented finding are incorporated in to the manuscript. For the detail corresponding author of this study can be contacted to access data stored in software through the under put email address; Gebi Husein Jima (gebihussein@gmail. com).
The authors declare that there is no conflict of interests.
We are very grateful to Arsi University College of Health Science for sponsoring the study. We also acknowledge Lode Hetosa district health office and Health centers (Huruta, Lode Jimata, Ligaba and Aleko health centers) for their support during data collection. We gain appreciate all study participants for sharing data.
The whole research fund was covered by Arsi University and authors. However the university had no role in the design of the study, collection, analysis, interpretation of data and in writing the manuscript.
Wagari Bekeshie Garbaba contributed in inception, proposal writing, designing methods, recruitment and training of supervisors & data collectors, analysis & write-up of the paper. Gebi Husein Jima contributed in inception, designing of the methods used, led the study, supervised and involved in the analysis stage of the project, final approval of the research and preparation of the manuscript. Abebe Ferede also contributed in methodology and analysis. Both authors read and approved the final manuscript.
Citation: Jima GH, Garbaba WB (2020) Postpartum Family Planning Utilization and Associated Factors Among Women Who Gave Birth in the Last 12 Months Prior to the Study in Lode Hetosa District, South East Ethiopia. J Women's Health Care 9:488. doi:10.35248/21670420.20.9.488.
Received: 10-Nov-2019 Accepted: 21-Apr-2020 Published: 28-Apr-2020 , DOI: 10.35248/2167-0420.20.9.488
Copyright: © 2020 Jima GH, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.