
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2020)Volume 11, Issue 10
COVID-19; Antibodies; Chest X-ray
The Covid-19 presents with variable timeline and clinical presentation involving different organs. The management of COVID-19 (acute phase) is based in our hospital with variable symptoms/organ dysfunction. The time interval between their recovery from first admission and presentation with newer symptoms varies.
Case 1
A 44 years old post renal transplant patient admitted with symptoms of diarrhea and tested positive for COVID-19 RT-PCR. She was having oxygen saturation of 98% in room air with stable cardiovascular and renal function. She was admitted in our hospital isolation unit for observation and got discharged to home 4th day when her symptoms subsided. She was in home isolation and tested COVID-19 (RT-PCR) negative 14 days after her first symptom.
She presented on day 16 (after first RT-PCR) with AKI and her oxygen saturation was 92% in room air. Cardiovascular observations were normal. Her chest X-ray showed bilateral patchy shadows (consolidation). She slowly developed shortness of breath and she was assisted with NIV (BiPAP). Arepeat Chest X-ray showed worsened patchy shadows and subcutaneous emphysema spread, but with no Pneumothorax. As she developed ARDS, she was intubated and ventilated. Bilateral ICD was done (Figure 1).
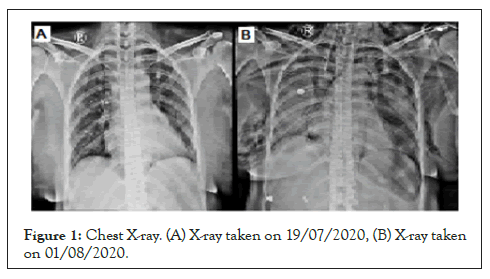
Figure 1: Chest X-ray. (A) X-ray taken on 19/07/2020, (B) X-ray taken on 01/08/2020.
Case 2
A 78 years old patient admitted with history of SOB for 7days and admitted to our CCU and found to have Mitral Valve regurgitation. He was dyspneic and treated with BiPAP. He was tested RT-PCR negative 7 days after his first day of SOB and intubated. He was started on inotropes and posted for MVR on day 10.
Surgery went uneventful and on second day of post-operative surgery he was extubated. After few days, he became progressively dyspneic with lot of secretions. He was intubated again, COVID RT-PCR was repeated (day 20 from first symptom) and found negative. Blood cultures were done to rule out other infections and found negative.
As patient improved, slow weaning with tracheostomy was planned.
Patient can’t be weaned from 7 cm H2O of PEEP.
ON day 25 we took another RT-PCR as he had high fever and it again came negative. CXR revealed bilateral patch shadows. On strong clinical suspicion (day 30), he was tested for IgG and IgM antibodies for COVID-19. For our surprise IgG for COVID-19 was positive.
Patients diagnosed positive for COVID-19 either symptomatic or asymptomatic during admission were discharged after testing negative for COVID-19 (RT-PCR) or recovery of clinical symptoms. Some of these patients presented variably with ARDS/LRTI, myocardial infarct, myocarditis [1], acute kidney injury, CVA days after discharge. According to one study patients with CT value higher than 34 (during first RT-PCR) are found to be at lesser risk. The definition of post-acute COVID also called by long COVID, post COVID sequel, post COVID syndrome varies in different countries. Considering false negative results are common and many mild clinical presentations go unreported, the definition of Post COVID is not definite. Generally, when the symptoms persist or complications start after a period of 2-3 weeks from day 1 of COVID-19 it falls under the category of long COVID. COVID-19 persistence after 12 weeks comes under category of ‘Chronic COVID” [2].
In UK COVID symptom study [3], it is found that 65% of people suffering from COVID-19 recovered to normal health in 2-3 weeks. The post COVID varies from mild clinical presentation to life threatening complications. The post COVID involves various organ systems including lungs, heart, brain, gut, skin, kidneys and eye.
The pathogenesis of such prolonged or delayed illness may be weak or absent immune response, relapse, re-infection, inflammatory or immune responses. Thrombo embolic pathogenesis is proposed to explain vascular events.
The mild symptoms includes cough, low grade fever, fatigue and may progress to severe symptoms as well. Various cases have been reported with following presentations:
CVS: Myocardial infarction, myocarditis, pericarditis, new CCF, arrhythmias [4].
RS: ARDS, severe pneumonic consolidation, pulmonary embolism, lung fibrosis.
CNS: Ischemic stroke, seizures, encephalitis, cranial neuropathies, neuro-cognitive defects
Endocrine: Diabetes
Renal: Acute kidney injury.
GIT: Gastrointestinal disorder.
Skin: Rashes, macula, vesicles.
The British cardio thoracic society has developed guidelines for follow-up assessment of recovered cases and rehabilitation programs. Daily home monitoring of pulse oximetry readings, breathing technique exercises, pulmonary rehabilitation programs are the significant recommendations.
Breathing technique is found to improve the function of diaphragm in the recovery phase, however caution advised to adapt slowly. Even pulse oximeter SpO2 readings after standard exertions (40 steps on level or 1 min sit-stand exercise) is suggested for early detection of post COVID. If SpO2 level decreases more than 3%, its positive [5]. Apart from physical status, COVID-19 also affects mental, social, cognitive status. The large volume of people recovering from illness and need for follow-up assessment had lead to formation of post COVID functional status scale. The scale is simple to use by the patients themselves and categorize the risk in the aftermath of acute COVID. A post VTE functional status scale is also being used for the same purpose, as thrombo embolism is one of the proposed pathogenesis of COVID-19.
PCFSS can be described in a more simplified form as [6]:
Class 0-No limitations in daily life/symptoms
Class 1-No limitations in daily activities, but persistent symptoms
Class 2-Occasional limitation in activities due to persistent symptoms
Class3-Not able to perform daily activities but can take care of self.
Class4-Not able to take care of self, needs assistance.
To conclude, COVID-19 spares no organ systems, no age group and the medicine is yet to form definite guidelines. Hence, the authors emphasizes the need for long term follow up of recovered COVID-19 cases and rehabilitation support in the following post COVID areas as recommended by NHS:
Lung: Pulmonary parenchymal and vascular disease, chronic cough.
Dysphagia: Risk factors are Patients requiring NIV assistance, CXR abnormalities.
Cardiac: Acute myocardial injury, arrhythmias, heart failure, peripheral arterial disease.
Neurological: Muscle weakness following ICU admissions, neuropathy.
Endocrinology: Diabetes.
General well-being and Nutrition support: Malnutrition, pressure ulcers, fatigue, poor oral dental health.
Psychiatric issues: Depression, post-traumatic stress disorder.
Renal issues: Acute renal injury.
Citation: Kumar S, Kumar R, Kumar S, Rohit KA, Vijayakumar S, Mathews M, et al. (2020) Post COVID-19 Complications and Need to Follow Up. J Anesth Clin Res. 11: 970.
Received: 15-Sep-2020 Accepted: 01-Oct-2020 Published: 08-Oct-2020 , DOI: 10.35248/2155-6148.20.11.970
Copyright: © 2020 Kumar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.