International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2023)Volume 11, Issue 5
Pelvic obliquity is a common, but overlooked condition and it causes functional scoliosis and leg length discrepancy which in turn predispose to musculoskeletal symptoms and a formation of trigger points causing myofascial pain. In the previous papers, we have described the three main manifestations of pelvic obliquity, their diagnosis, and methods of adjustment using patients’ muscular strength. In search of still more practicable methods, the author wishes here to study the effectiveness of a new simple technique of self-correction.
Methods: This preliminary study consists of 22 patients in a physiatric practice presenting various musculoskeletal pain symptoms. All three types of pelvic obliquities were present within the group and some had localized vertebral dysfunctions. The iliac crest levels and inferior scapular angles were measured using a Palpation Meter (PALM®) before and after the exercise. They all have undergone self-correcting maneuvers, as described in our previous article. By these patients, all the original dysfunction had recurred during the visit. The spinal rotations as described here were used as an alternative method during the same visit. The patients were taught to perform a movement consisting of alternating maximal spinal rotations. After the procedure, the pelvic position and possible vertebral position were assessed anew using the guidelines presented in our previous article. After the procedure, the pelvis and vertebrae involved were assessed anew.
Findings: Spinal rotations brought about pelvic alignment in 17 out of 19 cases (89%). and vertebral symmetry in all except one case, 15 out of 16 (93%). The difference between pelvic asymmetry and alignment is abrupt, and we have not been able to observe any intermediate stages. The fact that the study was implemented by one physician leaves it open to bias. The results have a tentative character calling for further research.
Conclusion: Studies covering reversible pelvic obliquity are still lacking though the condition appears to be common among patients suffering from musculoskeletal pain. Studies concerning the possible self-correcting methods are close to non-existent.
Sacroiliac joint; Functional scoliosis; Leg length discrepancy; Muscle energy technique; Pelvis; Pelvic tilt; Malalignment; Myofascial trigger points
Reversible asymmetry of the pelvis together with functional scoliosis and Leg Length Discrepancy constitutes a syndrome that has so far remained overlooked, both in literature as well as in clinical diagnostic and treatment practices [1]. Schamberger describes how pelvic obliquity predisposes to various musculoskeletal symptoms and limits physical abilities. Schamberger suggests that malalignment of the pelvis and/or spine is presented in 80% to 90% of the total adult population and might be responsible for back pain in 50% to 60% of the cases. Several studies have investigated sacroiliac joint dysfunction, functional scoliosis, and leg length discrepancy as separate entities. However, the possible interdependency of these three conditions has been mostly ignored [2]. Describe how pelvic asymmetry parameters were related to the occurrence of Non-Specific Chronic Low Back pain (NCLBP). The association between pelvic asymmetry and NCLBP was assessed by the global postural system. There are three distinctly different pelvic asymmetries:
• In upslip the iliac bone of the affected side has slipped or moved caudally causing apparent shortening of the ipsilateral leg and an S-scoliosis with elevation and more anteriorly positioning of the ipsilateral shoulder
• In anterior rotation of the iliac bone, the ipsilateral leg appears longer, and the iliac crest is elevated. It causes a C-scoliosis with an elevation and a more anteriorly positioning of the contralateral shoulder. These two conditions do not coincide.
• In torsion of the sacrum the iliac bones and legs are even. Sacrum has slightly rotated along a diagonal axis causing C-scoliosis and a more anterior position of the elevated shoulder. Sacral torsion often coincides with the two above-mentioned conditions (Figures 1-3).
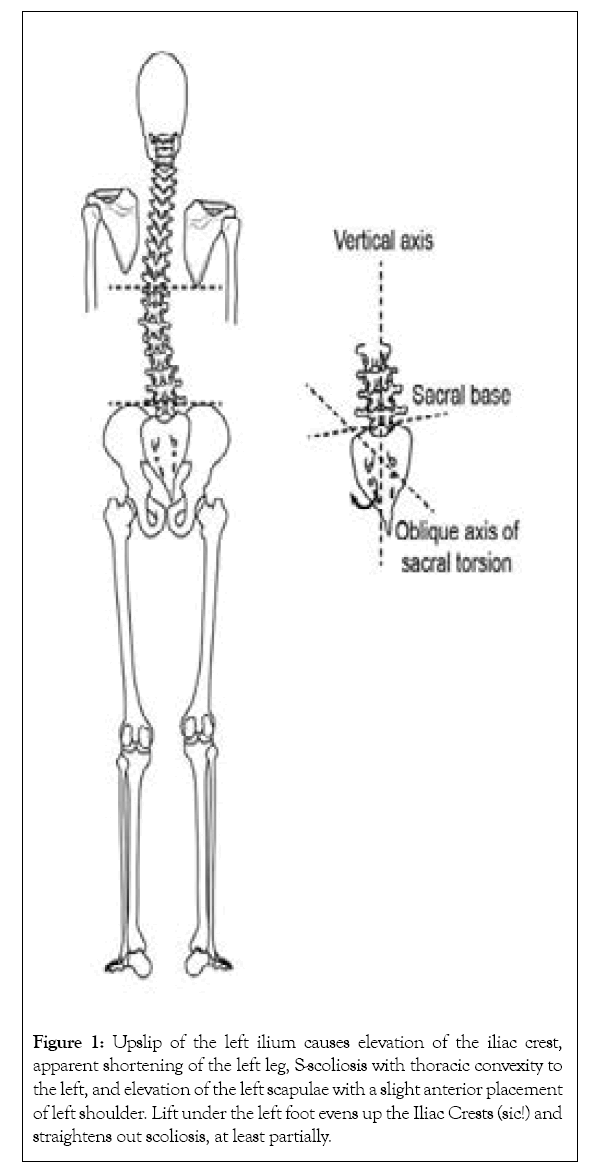
Figure 1: Upslip of the left ilium causes elevation of the iliac crest, apparent shortening of the left leg, S-scoliosis with thoracic convexity to the left, and elevation of the left scapulae with a slight anterior placement of left shoulder. Lift under the left foot evens up the Iliac Crests (sic!) and straightens out scoliosis, at least partially.
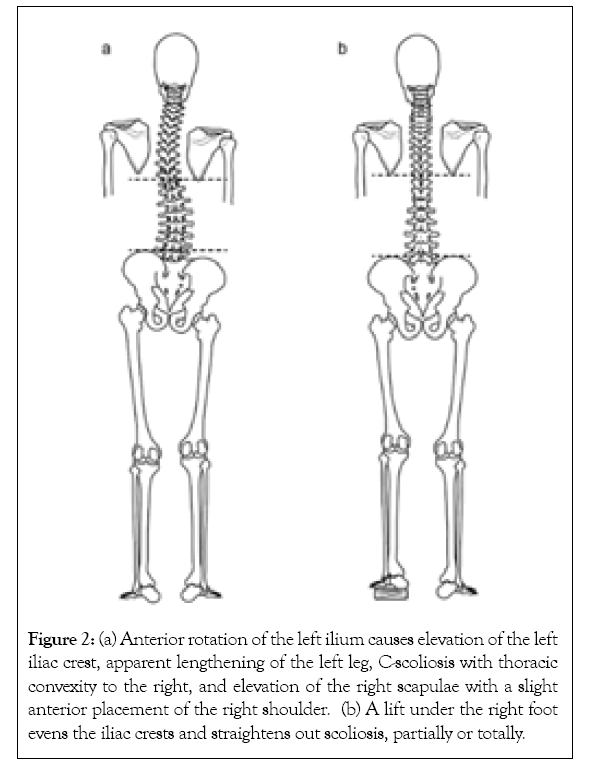
Figure 2: (a) Anterior rotation of the left ilium causes elevation of the left iliac crest, apparent lengthening of the left leg, C-scoliosis with thoracic convexity to the right, and elevation of the right scapulae with a slight anterior placement of the right shoulder. (b) A lift under the right foot evens the iliac crests and straightens out scoliosis, partially or totally.
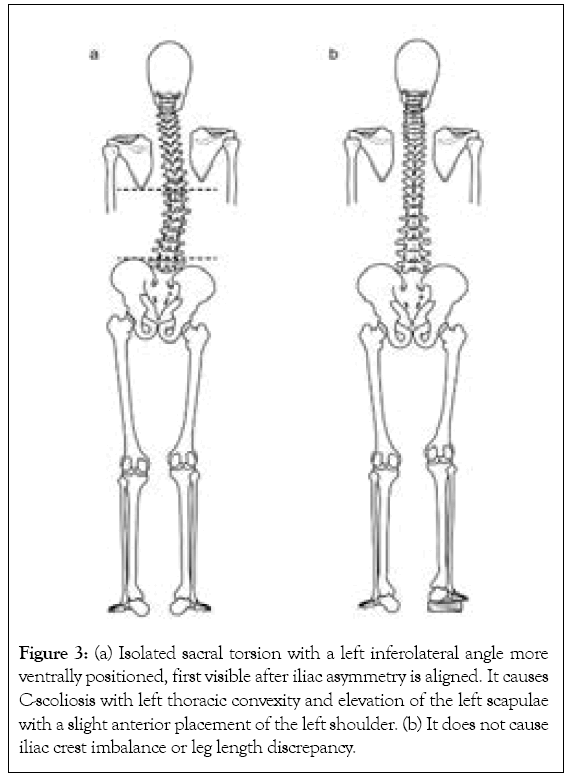
Figure 3: (a) Isolated sacral torsion with a left inferolateral angle more ventrally positioned, first visible after iliac asymmetry is aligned. It causes C-scoliosis with left thoracic convexity and elevation of the left scapulae with a slight anterior placement of the left shoulder. (b) It does not cause iliac crest imbalance or leg length discrepancy.
It is possible to bring the pelvis back to alignment using the patient’s muscular effort. A summary of the diagnostic criteria and the treatment using the self-correcting muscle energy technique is described in our previous article [3]. In search of still more practicable methods, than the ones described previously, the author wishes here to study the effectiveness of a new simple technique of self-correction. The practitioner was originally made aware of this exercise through a patient. This preliminary observational study aimed to examine whether full alternating rotations of the spine can bring about pelvic and vertebral symmetry. The outcome of this initial survey comes across as positive.
In this observational retrospective study, we analysed 22 patients having reversible pelvic asymmetry and some of them additionally localized vertebral dysfunction. They visited a private doctor’s office (a specialist in physiatrist) between February and December 2019 due to diverse complaints of pain or discomfort. There were 18 women, aged 21-60 years, and 4 men aged 34-51 years. The patient’s medical records were retrieved for analysis. The diagnostic and treatment procedures described in the introduction have been incorporated into the routine physiatric practice of the author over the past several years. This group consists of patients by whom pelvic obliquity has been diagnosed. The assessment of three possible pelvic malalignments was added to a usual physiatric examination. The iliac crest levels and inferior scapular angles were measured before and after the self-correcting maneuvers using a Palpation Meter (PALM®, Performance Attainment Associates, and Roseville, MN, USA) [4]. The Meter combines a caliper and an inclinometer that produce an estimate using a sine function slide ruler. This instrument is a valid, reliable, and precise tool to measure scapular position and pelvic crest height difference [5-7]. Additionally, the spinal column was palpated in all participants. Vertebral dysfunction is here defined as a single vertebra being locked to a rotated position so that its spinous process can be felt right or left from the central line and correspondingly the spinous process of aligned vertebrae has returned to the neutral position. This group had undergone the self-correcting maneuvers, as described in our previous article [3]. However, the original dysfunction immediately recurred after standing up or having done squats-a standard procedure for testing pelvic stability. The spinal rotations as described here were used as an alternative method during the same visit (Video 1) (Figure 4).
Video 1: The spinal rotations as described here were used as an alternative method during the same visit.
Figure 4: The patient was instructed to do maximal rotations of the spine. Feet are placed steadily abreast and the upper body makes in turn maximal rotations to left and right. It is important that also the head is turning maximally and at the endpoint, the eyes are also looking sideways as possible. The movement is repeated 10 times on both sides. Regularly the rotational movement is more restricted to one side because of the initial asymmetry, but during the exercise, the rotations become of equal range as the symmetry returns.
After the procedure, the pelvic position and possible vertebral position were assessed anew using the guidelines presented in our previous article [3]. Additionally, the patients were asked to perform 3 squats to test the stability of the pelvis. After the procedure, the pelvis and vertebrae involved were assessed anew. The patients examined were not exposed to additional examinations or interventions other than those belonging to the routines of the practice. Consequently, approval from an ethical board was not required.
Among this group of 22 patients, within the group of 22, in total 15 had vertebral dysfunctions. Spinal rotations brought about pelvic alignment in 17 out of 19 cases (89%) and vertebral symmetry in all except in one case 14 out of 15 (93%). By all the alignment endured 3 squats. This movement, despite its simplicity, is possibly an applicable option for self-correction in treating pelvic and spinal asymmetry and is certainly in need of further clinical studies (Table 1).
| Pelvic obliquity | Co-existing sacral torsion | Co-existing vertebral dysfunction |
|---|---|---|
| Left upslip, 7 | 5 | 4 (Th1, Th1, Th4, Th6) |
| Right upslip, 1 | 1 | - |
| Left anterior rotation in ilium 5 | 3 | 4 (C3, Th5 and L2, Th12, L2, L3) |
| Right anterior rotation 1 | 1 | |
| Isolated sacral torsion 5 | - | 4 (Th3, Th4, Th4 and Th12, Th5) |
| Remaining vertebral dysfunction after the pelvic obliquity had been treated by the previous standard method. | - | Th4, Th4, L4 |
Table 1: The Pelvic obliquity.
The scientific literature is practically void of research concerning pelvic obliquity that causes functional scoliosis and leg length discrepancies. Additionally, pelvic obliquity is mostly reversible, but this fact is often omitted. In manual medicine, leg length discrepancy (LLDs) are still considered anatomical and treated with leg lifts. Accordingly, slight scoliosis is often considered to be idiopathic although it can rather be functional and hence treatable. In the treatment of reversible pelvic obliquity, the most challenging problem seems to be its recurrent nature. Therefore, it is essential to teach patients to recognize it and subsequently treat it with self-correcting measures, making repeated visits to therapists for realignment unnecessary. A characteristic feature of these three pelvic asymmetries is a unilaterally elevated and anteriorly located shoulder. This can be used by the patient in self-assessment to distinguish the difference in front of a mirror before and after the exercise in question without having to further differentiate between the three subgroups. The fact that the study was implemented by one physician leaves it open to bias. The results have a tentative character calling for further research. The author describes the consistent coexistence of Atlantooccipital (AO) or Atlantoaxial (AA) dysfunction with pelvic asymmetry and their correction using the conjugate gaze method [7]. This suggests a close interdependency between dysfunctions of the pelvis and upper cervical spine. In the clinical work of the author, it has been repeatedly possible to bring the pelvis to alignment by mobilizing the upper cervical spine with the help of the above method. The explanation is that this exercise seems to act as mobilizing AO and AA functions (Video 2) (Figure 5). The results of this study can only be taken as tentative because this was a retrospective study among patients treated by a single physician who also performed all the assessments. Further research is needed for confirmation.
Video 2 : The spinal rotations as described here were used as an alternative method during the same visit.
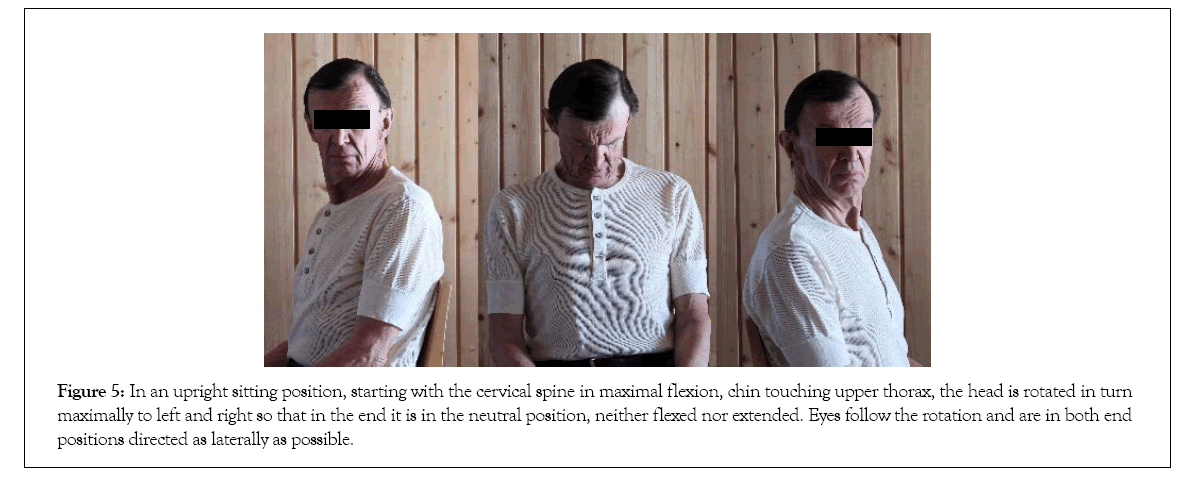
Figure 5:In an upright sitting position, starting with the cervical spine in maximal flexion, chin touching upper thorax, the head is rotated in turn maximally to left and right so that in the end it is in the neutral position, neither flexed nor extended. Eyes follow the rotation and are in both end positions directed as laterally as possible.
In this connection the author being subject to recurrent pelvic obliquity wishes to share a personal announcement. It has become apparent that a self-correcting mobilization of the upper spine with full rotations, will also in most cases bring about pelvic alignment.
None to declare
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Timgren J (2023) Possible Treatment of Pelvic Asymmetry and Vertebral Dysfunction by Spinal Rotations. Int J Phys Med Rehabil. 11:674
Received: 14-Apr-2023, Manuscript No. JPMR-23-23508; Editor assigned: 18-Apr-2023, Pre QC No. JPMR-23-23508 (PQ); Reviewed: 03-Apr-2023, QC No. JPMR-23-23508; Revised: 10-May-2023, Manuscript No. JPMR-23-23508 (R); Published: 18-May-2023 , DOI: 10.35248/2329-9096.23.11.674
Copyright: © 2023 Timgren J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.