Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2021)
Bowen's disease is the in-situ form of squamous cell carcinoma rarely reported in the dark skin type, especially in sub- Saharan Africa. A 51-year-old patient presented with a 7 cm infiltrated plaque in the perianal area, with condylomas on the top of the plaque, evolving for 2 years. Histopathology confirmed the diagnosis of Perianal Bowen's disease. Surgical excision with a 5 mm margin allowed healing without recurrence, after a follow-up of 2 years. This is first reported case of perianal Bowen's disease in Senegal. Our observation is particular not only because of the rarity but also due to the existence of condylomas on the top of Bowen's disease and the absence of recurrence after 2 years follow despite the size and location.
Bowen's disease; Condyloma; Perianal; Dark skin
Bowen's disease is a situ form of cutaneous squamous cell carcinoma [1]. It is most often found in photo-exposed areas [2,3]. The prognosis is linked to the progression risk to invasive squamous cell carcinoma, which is about to 3% to 5% [4]. The perianal location is rare and involve papillomavirus infections as a risk factor [5,6]. It is rarely reported in a dark skin phototype [7]. We report the first observation of perianal Bowen's disease developed on the top of condyloma in a dark phototype in Senegal.
A 51-year-old woman, without remarkable past medical history, and any notion of avowed risky sexual behavior, consulted for anal swelling that started for 2 years. The general condition was good and there was no fever. Dermatological examination revealed an infiltrated verrucose patch, with hyperpigmentation and leukoplakia in some areas, localized in perianal region, measuring 7 cm in largest diameter and more extensive on the right (Figure 1). The plaque was topped with slightly exophytic lesions, in a shape of "cockscombs", reminiscent of condylomas. On questioning, the condylomas had preceded the gradual installation of the closet by a year. There was no lymphadenopathy, and the digital rectal examination was unremarkable.
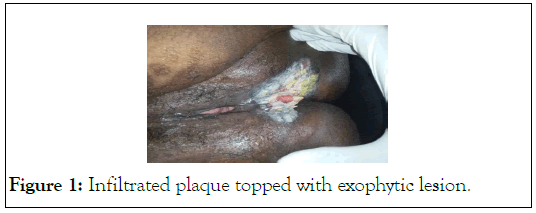
Figure 1: Infiltrated plaque topped with exophytic lesion.
In front of the cupboard, the diagnostic hypotheses evoked were sclero-atrophic lichen, Paget's disease, basal cell carcinoma, melanoma, and Bowen's disease. Histopathology made it possible to make the diagnosis of Bowen's disease by objectifying a strongly acanthotic epithelium, basophilic keratinocytes with numerous mitoses and nucleo-cytoplasmic atypia and dyskeratosis (Figure 2). The dermis was the site of a dense lympho-plasma cell infiltrate. Thoraco-abdominal-pelvic computed tomography was normal. The HIV and syphilitic serologies were negative, as well as AgHbs. A large surgical excision, with 5 mm margins, was performed after a multidisciplinary consultation meeting. The outcome was good, and no recurrence was noted after a 2-year follow-up (Figure 3).
Figure 2: Multinucleated epidermal cells and dyskeratotic cells are found throughout the epidermis (x100).
Figure 3: Complete remission after surgical excision after a follow-up of 2 years.
We report a case of perianal Bowen's disease occurring in a patient with a dark skin phototype infected with condyloma. The clinical manifestations of Bowen's disease are variable [8], and a clinical presentation with an infiltrated plaque with partial hyperpigmentation and leukoplakia, is seen only 2% of cases [9-11]. This clinical picture is compatible with several diagnostic hypotheses, but the chronological evolution of the lesions and the histopathologic finding suggest the diagnosis of Bowen's disease on top of a papilloma virus infection.
Bowen's disease is rarely reported in people with a dark skin phototype [2]. In the United States, Mora et al. [12], reported 19 cases over a period of 20 years in a black American population. In the same country, in another series of 155 patients with Bowen's disease, Graham et al. [13] had found only 4 cases of dark skin patient. Similarly, in a series of 130 patients with Bowen's disease in a study by Callen et al. [14], there were no patients with a dark skin phototype. In sub-Saharan Africa, isolated cases are reported by Malian and Nigerian authors [7,11].
The rarity of Bowen's disease in dark phototypes could be explained by the natural photoprotection offered by the presence of abundant eumelanin in epidermis. In fact, ultraviolet rays constitute a risk factor for the onset of Bowen's disease, explaining the most common location in photo-exposed areas in persons with fair skin [3,4,15]. On the other hand, in dark skin phototype with Bowen disease the involvement of nonsun exposed area, indicate the implication of other risk factors such as papillomaviruses. These would explain the perianal location in our patient. The non-fortuitous association with HPV infection supports this hypothesis. Peixoto et al. [16], have shown patients with anal condyloma were at greater risk of developing carcinoma in situ. In a series of 82 patients with anal warts and 152 performed biopsies, carcinoma in situ was found in 66% of cases [16] and the most common HPV’s genotype were oncogenic genotypes 16 (49%) and 18 (27%). However, 76% of their patients were infected with HIV, unlike our patient. The oncogenesis mechanism of HPVs infection comprises the functional inactivation of the tumor suppressor proteins p53 and pRb by viral oncogenic proteins E6/E7 [17,18].
Bowen's disease progresses slowly to invasive squamous cell carcinoma. This progression is about 3% to 5% of cases over a period of 5 to 10 years, with a survival rate of 80% after 5 years [4].
As treatment there is a multiple therapeutic options such as surgical excision, radiotherapy, cryotherapy, local application of imiquimod or 5 fluorouracil, dynamic phototherapy, and photocoagulation through argon laser [4]. Wide surgical excision with a security margin of 5 mm to 15 mm is the treatment of choice, especially for the perianal location [19], as in our patient. The width of the excision is extremely important as Bowen's disease cells can extend beyond the macroscopic limit of the lesions [8]. Some authors recommend a margin of 10 mm for a better reduction of the recurrence risk [8]. In a series of 26 patients with perianal Bowen disease, Brown et al. [20] after a mean follow-up of 9 months found a recurrence rate of 23%. In our patient, after two years of follow-up the evolution was still favorable. However, in majority of cases, recurrence of perianal Bowen's disease occurs in the anal canal [8], justifying regular anoscopic follow-up.
Perianal Bowen's disease is rare in the dark phototype. Moreover, its clinical presentation can be very unusual. However, surgical removal, which is more accessible in lowincome countries, can be successful. However, surgical excision, which is more accessible in countries with limited resources, can give good results.
The authors declare no conflict of interest.
Citation: Diop K, Diop A, Kante MD, Ndiaye MT, Ndour N, Sarr M, et al. (2021) Perianal Bowen's Disease and Condyloma in Immunocompetent Dark Skin Phototype Senegal. J Clin Exp Dermatol Res. S13:585.
Received: 25-Oct-2021 Accepted: 08-Nov-2021 Published: 15-Nov-2021
Copyright: © 2021 Diop K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.