Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2023)Volume 8, Issue 1
Background: The patient room whiteboard serves as an effective communication tool between the patient and the healthcare team. Effective communication is crucial for both patient safety and quality of care.
Aim: To improve patient provider communication with the use of the patient room whiteboard.
Objectives: To facilitate patient and family knowledge for the plan of care and provider identification, and to increase the staff compliance with the utilization of the patient room whiteboard.
Design and setting: This is a Quality Improvement (QI) project using the Model For Improvement (MFI). The implementation of change was facilitated by the Plan-Do-Study-Act (PDSA) methodology. The study has been conducted in 2015 in pediatric in-patient unit in a general hospital in Al Wakra, Qatar. Patient and staff indepth interviews and surveys were conducted.
Results: Provider identification of physicians and nurses increased from 45% to 100% and 60% to 100% respectively during 2015 and 2020. The percentage of patients’ awareness of their admission goal and estimated date of discharge increased from 58% in 2015 to 100% in 2020 and 68% in 2015 to 100% in 2020 respectively. Patients’ perception of the whiteboard was helpful throughout their admission and improved from 72% in 2015 to 100% in 2020. Nurse’s compliance increased from 40% in 2015 to 100% in 2020.
Conclusion: The patient room whiteboard promotes effective patient provider communication and improves patient awareness of their healthcare providers, estimated discharge date, and plan of care.
Whiteboard; Communication tool; Improving patient’s knowledge; Goals of hospital admission; Nurse compliance
Effective communication is crucial for both patient safety and quality of care. According to the Joint Commission International (JCI), communication breakdown is the most frequently cited root cause for sentinel events [1]. A key element of the commission’s 2009 national patient safety goals for hospitals is improving the effectiveness of communication among health care providers and engaging patients in the plan of care. Effective communication that is timely, accurate, complete, unambiguous, and understood by the recipient reduces error and results in improved patient safety [2]. In a 2005 report from Australia’s national health and hospitals reform commission, every year doctor to patient communication problems contribute to more than half a million dollars in preventable patient complications in emergency rooms alone. To reduce such problems, it’s crucial that contact between patients and caregivers is improved whenever possible [3]. Other study concludes that improved health care team communication and teamwork have been shown to enhance the job satisfaction of nursing staff, which has been linked to improved patient outcomes [4,5]. Whiteboards at a patient’s bedside can serve as a quick reference for the interdisciplinary team and a great platform to relay the information from the healthcare team to the caregiver. Patients and their families also can write questions for their providers on the whiteboard, which triggers a nonverbal dialogue between patients and healthcare providers. Moreover, the white board can promote patient safety, increase patient satisfaction, and serve as a mechanism to engage patients in their care, encourage patient autonomy and adherence to care regimen which in turn improves patient outcomes, increase the satisfaction between nurse and physician communication and help in reducing missed nursing care [6]. One of the main tools that many hospitals use to facilitate interdisciplinary communication as well as the communication between the healthcare team and the patients is the whiteboard. White boards have spaces to fill in patient identification, patient status, and name of attending physician, name of current shift’s nurse, dietary needs; daily goal, reception area welcome notes, and other information. In the in-patient unit, patients’ plans of care and their primary healthcare provider change often. This drastic change gives a feeling of uncertainty to patients and relatives regarding their healthcare team. Moreover, often they are not well-informed about the plan of care and discharge plans [7]. Hence, the use of patient whiteboards serves as a visual explanation and reminder. Although whiteboards have been used for a long time in the in-patient unit as a communication tool, there is limited literature that reported their effectiveness in increasing patient provider communication. Therefore, the purpose of our study was to determine the effectiveness of the whiteboard as a tool to facilitate patient-provider communication. The primary objective was to increase the patients’ knowledge of their care providers, the plan of care and estimated discharge, and their overall satisfaction with the care provided. The secondary objective was to increase the staff’s compliance with the use of the whiteboard.
Study design
This is a Quality Improvement (QI) project using the Model for Improvement (MFI). The MFI framework is designed to support organizations in answering fundamental questions before agreeing on drivers for change. The implementation of change was facilitated by the Plan-Do-Study-Act (PDSA) cycles methodology [8]. Quality Improvement (QI) is a systematic, datadriven framework that is popular amongst healthcare organizations that aims to introduce change and foster improvement through the close monitoring of selected metrics. One of the major components of this framework is that it engages relevant subject matter experts from the field, therefore ensuring a multidisciplinary contribution in achieving significant performance improvements. QI can be described as an iterative or multi-stepped process by which process modifications are progressively introduced with anticipated improvement [9].
The pilot of the whiteboard project was done in the pediatric in-patient unit of Al Wakra hospital, Qatar. The whiteboard was attached to the patient’s room wall, perpendicular to the bed, for easy access and to allow the healthcare team to communicate with the patient and family by answering questions and considering suggestions. The whiteboard is adequately sized, readable, uncomplicated, and visually attractive, with attached erasable markers. The content of the whiteboard was in english, which included the room number, current day and date, the names of the care team involved, daily goals, a space for questions, patient’s weight, food or drug allergies, the expected date of discharge and comments or suggestions from the patient and family attached. Once the patient was admitted, the assigned nurse gave an orientation about the bedside whiteboard and its use. Even though the information was written in english; the nurses ensure that the language preferred by the patient is used for the explanation. The whiteboard was updated at the change of shift, during ward rounds, and as needed. Nurses ensure that patient privacy is protected by not including sensitive information or sharing patient details when updating the whiteboard. During shift rounds, the charge nurse checked the patient room whiteboard for completeness of data for auditing. The primary nurse was informed to identify and address issues or concerns about any missing data on the whiteboard (Figure 1).
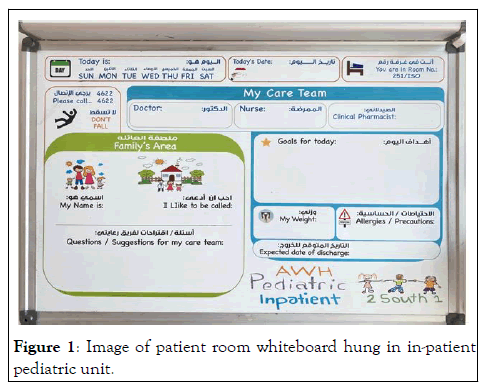
Figure 1: Image of patient room whiteboard hung in in-patient pediatric unit.
Setting and sampling
The quality improvement project was conducted in the inpatient pediatric unit of Al Wakra hospital over a 3 months pilot period. Al Wakra Hospital (AWH) is a general hospital and one of the 11 facilities that make up Hamad medical corporation in Qatar and provides comprehensive healthcare to people of all ages.
Challenges and PDSA methodology
There were four challenges to implementing the project, which the QI and healthcare team solved through the PDSA methodology. First, the whiteboard was in english and was not suitable for Arabic patients. The whiteboards were redesigned to include the translation to the Arabic language to increase usability and acceptance. Figure 2 shows the redesigned whiteboard template. Second, the whiteboard design was not usable due to the background image, and the markers always became misplaced. The design of the whiteboard was revised to remove the background image. The whiteboard markers and dust holders were fastened on top of the board, out of children’s reach. The availability of the features was checked every shift; the marker supply was readily available in the nurse station to quickly replace those with fading ink. Third, the board’s material did not allow good cleaning, causing untidiness, and overwriting, making the instructions unclear. The whiteboard material was changed for easy removal of marker stains. Fourth, the whiteboards were either not updated regularly, or the information updated was not complete. The charge nurses were instructed to fill incomplete areas during the regular rounds and remind the staff to update them regularly. Specific duties were assigned among the interdisciplinary team to complete different sections of the whiteboard. Patient and staff in-depth interviews and surveys were conducted to collect the data related to staff compliance, board completion, staff, patient, and family satisfaction. After the initial implementation period in 2015, the Whiteboard project was extended to all units in the core network. Data were collected monthly and ranged from 30-60 audits. Random checking was performed by department heads in 8 units year 2016 to 2017, and post-implementation data were collected for the year (2015 to 2020) for patient and family satisfaction.
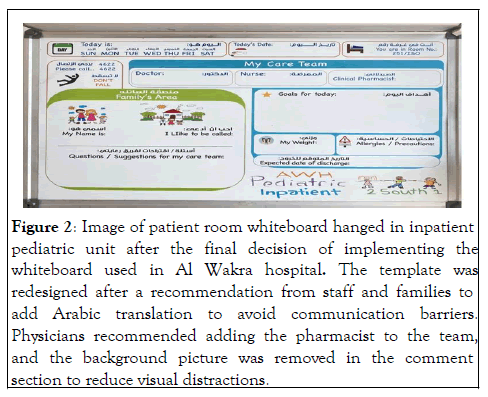
Figure 2: Image of patient room whiteboard hanged in inpatient pediatric unit after the final decision of implementing the whiteboard used in Al Wakra hospital. The template was redesigned after a recommendation from staff and families to add Arabic translation to avoid communication barriers. Physicians recommended adding the pharmacist to the team, and the background picture was removed in the comment section to reduce visual distractions.
A total of 120 patients and staff 35 completed the questionnaires and interviews. The patients and their families expressed satisfaction with using whiteboards as a communication tool, as evident from the data from the survey and interviews. The percentage of patients/families aware of their primary physician increased from 45% in 2015 to 100% in 2020 (Figure 3), and awareness of their primary nurse rose from 60% in 2015 to 100% in 2020 (Figure 4). More percentage (100%) of patients/families in 2020 knew their admission goals as compared to the ones (58%) in 2015 (Figure 5). About 100% of the patients/families (2020) were aware of their estimated discharge date, which was only 68% in 2015 (Figure 6). More families found the whiteboard helpful throughout their admission (increased from 72% in 2015 to 100% in 2020) (Figure 7). The staff compliance was increased from 40% in 2015 to 100% in 2020, indicating positive response and acceptance (Figure 8).
Figure 3: Percentage of patients/families who knew their physician’s name.
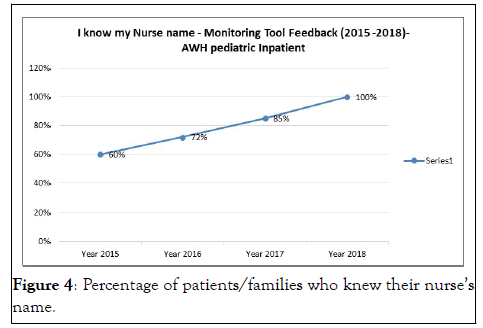
Figure 4: Percentage of patients/families who knew their nurse’s name.
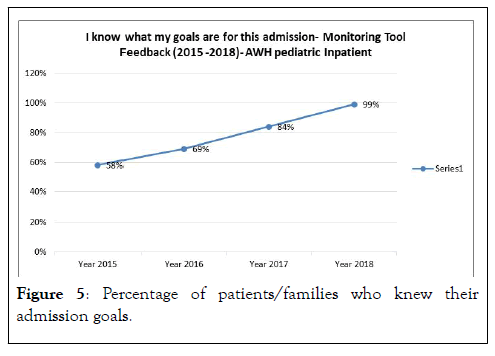
Figure 5: Percentage of patients/families who knew their admission goals.
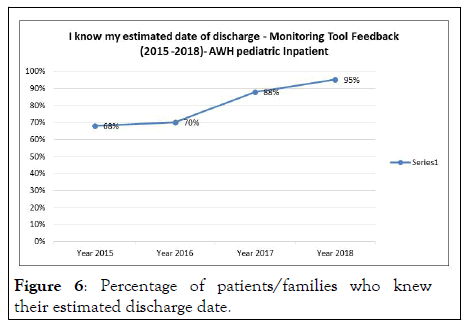
Figure 6: Percentage of patients/families who knew their estimated discharge date.
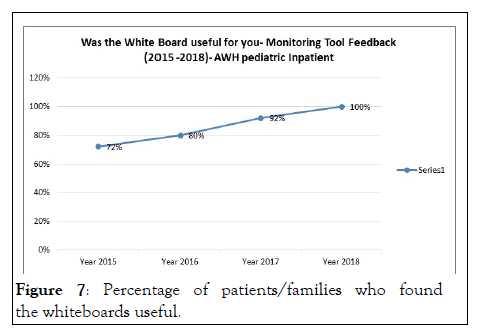
Figure 7: Percentage of patients/families who found the whiteboards useful.
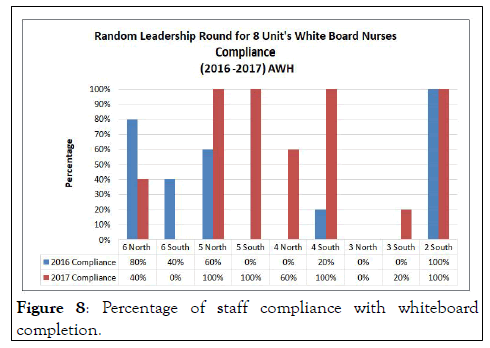
Figure 8: Percentage of staff compliance with whiteboard completion.
Our study revealed that the patient room whiteboard is a simple yet effective communication tool between the healthcare provider and patient. With the use of in-patient whiteboards, many patients and their families knew their healthcare providers, which was consistent with the results obtained in previous studies [10,11]. Improved provider identification, enhanced communication between the healthcare team and patient, and enhanced knowledge of their course of disease management led to improved patient satisfaction; these results aligned with studies done by Tan, et al. A similar analysis performed involving the use of whiteboards in labor room showed to improve patients' knowledge of their delivery physician's name and patient satisfaction with care on labor and delivery [12]. However, there is a need to orient patients and their families to whiteboards and their proper use [13]. We revised the whiteboard template based on the challenges faced to improve its usability. The revised whiteboards were considered much more user-friendly and were able to help capture critical information for patient care. Nowacki, et al. reported similar results with revised whiteboards in their in-patient pediatric facility.
Strength and limitation
The strength of our study was the large subject size and the consistency of data collection. The implications of the results emanating from this large sample can be applied to most clinical settings, given that patient provider communication is the cornerstone of all patient-centered care strategies. The limitation of the study was the fewer data points of patient-provider communication, and the data quality could have been increased with the inclusion of other data points or measured parameters.
The patient room whiteboard is a valuable communication tool for patients/families and the healthcare staff by promoting effective communication, maintaining goal directed care for the patient, and contributing to a significant increase in the patient/family’s overall hospital stay satisfaction. It became a norm for nurses and physicians to engage the family in their care. Encouragement of a patient room whiteboard is recommended for continuous quality patient care and facilitating effective communication between the patient and the healthcare team.
Ethical consideration
The patient room whiteboard project was reviewed and approved by the Al Wakra hospital committee for quality improvement. It was an improvement project and not a research study on human subjects. Therefore, ethical approval was not required. However, patient consent was secured using a detailed assent form.
Citation: Mustafa G, Abraham S, Salameh K, Zakaria A, Maghreby K, Atrash M, et al. (2023) Patient Room Whiteboard as an Effective Communication Tool: A Quality Improvement Project, Al Wakra Hospital-Qatar. Clin Pediatr. 8:226.
Received: 07-Jun-2022, Manuscript No. CPOA-22-17873; Editor assigned: 08-Jun-2022, Pre QC No. CPOA-22-17873(PQ); Reviewed: 22-Jun-2022, QC No. CPOA-22-17873; Revised: 15-Sep-2022, Manuscript No. CPOA-22-17873(R); Published: 31-Jan-2023 , DOI: 10.35248/2572-0775.22.8.226
Copyright: © 2023 Mustafa G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.