Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 1
Despite Meckel´s Diverticulum (MD) being the most common congenital anomaly of the gastrointestinal tract, symptomatic presentation in neonates is rare. In new-borns, bowel obstruction and perforation have been described as the most frequent clinical manifestation of MD. We describe a case of neonatal Meckel´s Diverticulum presenting as lower gastrointestinal bleeding and a review of the literature. We have found only one other case of rectal bleeding caused by a MD in a neonate reported so far. The diagnosis of intussusception in the neonatal period requires a high index of suspicion and does not have any specific radiological findings or signs, in contrast to older children. Misdiagnosis leads to delay in treatment, which leads to intestinal perforation and necrosis.
Meckel’s Diverticulum (MD); Gastro intestinal bleeding; Neonate; Enteral Nutrition (EN)
Meckel’s Diverticulum (MD) is a congenital gastrointestinal anomaly that results from the persistence of the omphalomesenteric duct at its attachment site to the distal ileum on the anti-mesenteric border. MD is the most common gastrointestinal congenital malformation in children, with a reported incidence of 2%–3%. MD patients are usually asymptomatic, with symptoms only appearing in complicated cases. Reported complications of MD, which occur in only 4.2%–9% of patients, include intestinal obstruction, diverticulitis, volvulus, intussusception and hemorrhagic ulcers. We report a very rare case of lower gastrointestinal bleeding of Meckel's diverticulum. Preoperative diagnosis of gastrointestinal bleeding is a challenge because of its rarity and the absence of specific radiological findings and clinical presentation.
A 35-week preterm was admitted to the general neonatal ward due to prematurity and low birth weight (1900 g). He was delivered by an emergency caesarean-section for bradycardia, with an Appearance, Pulse, Grimace, Activity and Respiration (APGAR) score of 5-9-10, requiring positive pressure ventilation for 2 minutes. The initial physical examination was normal and meconium was passed within the first 16 hours after birth.
At 48 hours, he emitted a stool with a significant amount of fresh blood. Blood analysis was normal, with a hemoglobin of 21 g/dL and a Receptor Component Protein (RCP) of 8.6 mg/L. Abdominal examination was normal, however, he continued with emitting bloody stools. The following day, RCP raised to 40 mg/L and platelet count decreased to 77,000.
Taking into consideration the hyponatremia, thrombopenia, abdominal distention and bloody stools in a late preterm infant, the first suspected diagnosis in this case was NEC. The radiography showed no signs of perforation, so a conservative management was taken. He was prescribed Nothing by Mouth (NPO) and empiric antimicrobial therapy with intravenous vancomycin and piperacillin-tazobactam. An urgent abdominal x-ray showed “small bowel faeces sign” in the ascending colon, with no signs of perforation. The pediatric surgeons ruled out the need of an urgent intervention at this moment.
The patient had a positive response; he completed a week of NPO with Total Parental Nutrition (TPN) and intravenous antibiotics. Each day, the stools were less frequent, with less blood and darker in colour. An abdominal ultrasound showed no apparent alterations. Laboratory tests were repeated; platelet count normalized and RCP descended to 21 mg/L. Enteral Nutrition (EN) was reinitiated with hydrolysed formula and the patient was discharged with a weight of 2320 g.
At 23 days of age, the patient was taken to emergency services for a 24-hour history of irritability, constipation and projectile vomiting after the last two feeds. An urgent abdominal x-ray showed a fixed intestinal loop and an absence of distal gas (Figure 1). He was readmitted with a suspected diagnosis of bowel obstruction.
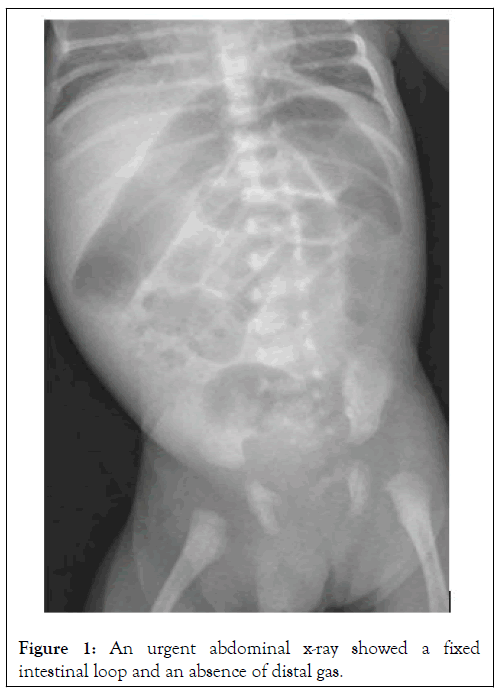
Figure 1: An urgent abdominal x-ray showed a fixed intestinal loop and an absence of distal gas.
On admission, the abdomen was swollen, tense, a dark erythematous colouration and painful with palpation. He was examined by the pediatric surgeons, ruling out the need of urgent surgery. He was again prescribed NPO and antibiotics with vancomycin and meropenem. Over the next few hours, the evolution was unfavourable. The patient present uncontrollable pain that required paracetamol, metamizole and a perfusion of fentanyl. He emitted two stools with strings of blood and on examination, the abdomen was even more distended. Laboratory tests showed a mild hyponatremia (132 mEq/L) and an elevation of RCP to 56 mg/L, with a normal hemogram. After an urgent abdominal ultrasound detected free abdominal fluid, it was decided the patient was to undergo explorative laparotomy. A Meckel´s Diverticulum (MD) was identified and removed (Figure 2). The histological report later confirmed the diagnosis.
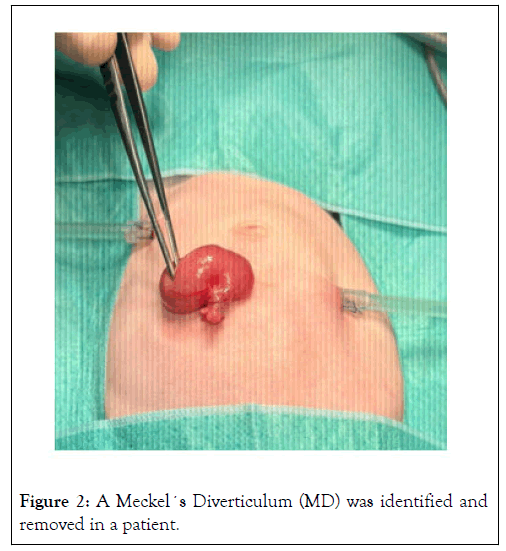
Figure 2: A Meckel´s Diverticulum (MD) was identified and removed in a patient.
The postoperative evolution was favourable. He continued NPO with TPN for 6 more days. EN was reinitiated and well tolerated. The patient was discharged 11 days postop with no complications.
Despite Meckel´s Diverticulum (MD) being the most common congenital anomaly of the gastrointestinal tract, symptomatic presentation in neonates is rare [1,2]. Complications in this age group occur in less than 4 % of cases [3]. In new-borns, bowel obstruction and perforation have been described as the most frequent clinical manifestation of MD [4]. We have found only one other case of rectal bleeding caused by a MD in a neonate reported so far [2].
MD follow the “rule-of-twos”, it affects 2% of the general population, 2 % are symptomatic, is located within two feet (<60 cm) of the ileocecal valve, measures two inches (5 cm) in length, presents two types of heterotopic mucosa (the most common being gastric and pancreatic), is twice as common in males than females and a large proportion of cases are diagnosed before the age of two. It is a remanent of the omphalomesenteric duct, a connection from the yolk sac to the gut in the embryo that provides nutrition until the placenta forms. It usually separates and regresses between the fifth to the seventh week of gestation, an incomplete obliteration of the duct results in a diverticulum in the small intestine [1].
MD are frequently underdiagnosed as many cases are clinically silent and diagnosed as an incidental finding in surgery or on autopsy [5]. The most common clinical presentations are painless rectal bleeding, intestinal obstruction (from volvulus or intussusception) or inflammation (diverticulitis) that causes abdominal pain and vomiting, simulating acute appendicitis [6]. The usual age of presentation is from 2 to 5 years of age. MD should be strongly suspected when a child has massive rectal bleeding [7]. This bleeding is a result of ulcers in the intestine caused by the acid secreted from the ectopic gastric mucosa of the diverticulum [8]. In neonates, lower gastrointestinal bleeding, can be caused by a variety of situations. Differential diagnosis must include ingestion of maternal blood, Hirschsprung’s disease, infant haemorrhagic illness, anal fissure, volvulus, cow´s milk protein allergy and Necrotizing Enterocolitis (NEC) [7,9].
Neonatal symptomatic MD are rare, when reviewing the literature, most cases present as pneumoperitoneum by perforation or intestinal obstruction. Perforation and obstruction are the result of inflammation [10]. However, a preoperative diagnosis is very difficult due to the rarity and the simulation of other, more common abdominal complications.
MD cannot be identified in radiography nor ultrasound images. The “gold standard” imaging test is a technetium-99m ( 99mTc) pertechnetate scintigraphy, with a 90% accuracy in children [6]. However, this test is contraindicated if there is active bleeding and is only indicated if there is a strong clinical suspicion.
Surgery is the treatment of choice. Depending on location and size, an open diverticulectomy or segmental bowel resection with terminal-terminal anastomosis is performed. Many cases, such as this one, are incidental findings and are found with explorative laparotomy.
In summary, despite being very rare, MD must be considered in the differential diagnosis of neonatal lower gastrointestinal bleeding and an early surgical approach is essential to prevent future complications.
We report an internal bleeding caused by Meckel's diverticulum in a prematurely born neonate, with likely origin in the prenatal period as evidenced by the presentation, surgical findings and pathology. Intussusception in neonates can present very similar to NEC and the differential diagnosis should be made early to prevent increased morbidity from delayed management.
Although surgery represents the appropriate treatment of gastrointestinal bleeding with complicated MD, there is no consensus on the optimal treatment of uncomplicated MD: routine resection of MD is not advised and it should be based on identified risk factors because of possible complications following its resection.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Martin LB, Diaz FJG, Vallecillo MG, Perez PR (2024) Neonatal Meckel´s Diverticulum Presenting as Lower Gastrointestinal Bleeding. Clin Pediatr. 09:260.
Received: 02-Jan-2024, Manuscript No. CPOA-24-29630; Editor assigned: 05-Jan-2024, Pre QC No. CPOA-24-29630 (PQ); Reviewed: 19-Jan-2024, QC No. CPOA-24-29630; Revised: 26-Jan-2024, Manuscript No. CPOA-24-29630 (R); Published: 02-Feb-2024 , DOI: 10.35248/2572-0775.24.09.260
Copyright: © 2024 Marti LB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.