Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research Article - (2021)Volume 11, Issue 1
The objective of this non-randomized, within-group comparison was to evaluate the addition of mindfulness as a new technique in an outpatient group therapy program with participants diagnosed with a psychotic spectrum disorder, alongside of cognitive behavioral therapy. Additional objectives were to replicate concepts from earlier works, to evaluate scores on depression and anxiety scales related to distressing psychosis, and to determine if participants’ responses were a mindfulness-based response or an experiential-avoidance response. Participants completed the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder 7-item scale, at admission and discharge. The first experiment compared matched scores of those who received mindfulness training plus standard psychiatric treatment (treatment as usual: TAU) against those who received TAU. The second experiment compared age using matched scores from participants who received mindfulness training plus TAU. Participants attended group therapy for a five-week minimum, and were taught the mindfulness practices of breath, acceptance, observation, remaining non-judgmental, and letting go. The first experiment showed a significant pretest to posttest decrease in anxiety and depression scores in those who received mindfulness training and TAU. A Tukey-Kramer test indicated a statistically significant finding for the GAD-7. Secondary data indicated improvement in skills and the importance of the mindfulness training. The TAU only group showed a significant reduction in depression but not anxiety. In the second experiment, both the older and younger groups showed a significant pretest to posttest decrease in anxiety and depression. The findings have implications for mindfulness training as an effective method for decreasing anxiety and depression in psychosis.
Mindfulness; Psychosis; Anxiety; Depression; Outpatient; Group therapy; Schizophrenia
The history of mindfulness as an intervention
Kabat-Zinn [1,2] described mindfulness as a way of focusing attention purposefully in the present moment, non-judgmentally; he developed mindfulness-based stress reduction (MBSR) to use as a psychiatric intervention. Kabat-Zinn [2] also developed a technique alongside cognitive behavior therapy (CBT) and emphasized that distress and suffering result from the mind and not from sensations. Segal, Williams, and Teasdale [3] drawing from Kabat- Zinn concepts, wrote about Mindfulness-Based Cognitive Therapy (MBCT) as an independent intervention. A meta-analysis of the two interventions, reported by Baer [4] showed clinical benefits for those who were experiencing pain, stress, anxiety, depression, and disordered eating behaviors; mindfulness treatment therefore became an accepted intervention.
Historically, the recommended treatment for psychotic disorders from the National Institute of Mental Health (NIMH) has been the use of anti-psychotic medications, individual therapy, cognitive behavioral therapy, and psychoeducation [5-8]. Personcentered care and recovery-oriented treatment were added in 2014 [9]. Although individual CBT and Cognitive Behavior Therapy for Psychosis (CBTp) is recommended by NIMH and the National Institute for Care Excellence [10] for patients with a diagnosis of psychosis, Chadwick, et al. [11] noted that access to group CBTp remains poor, and that it lacks sufficiently robust evidence of its effectiveness. Chadwick, et al. [11], argues that CBTp is aimed at trying to control psychotic symptoms; whereas Person Based Cognitive Therapy (PBCT) is aimed at alleviating distress. Chadwick, et al. [11] noted that PBCT has lasting effects on improvements in mood, reductions in depression levels, and behavioral change, and that CBTp has not typically found a reduction in depression levels [12].
Past research urged caution when using mindfulness with psychosis [13]. However, randomized studies using Acceptance and Commitment Therapy (ACT), which includes mindfulness training, reported a reduction in relapses for inpatients experiencing psychosis, as well as a decrease in hospital readmissions [14,15].
Early developments
With no recommended group therapy for psychosis, or use of mindfulness from either NIMH or NICE, Chadwick, Newman- Taylor, and Abba [16] developed a 10 minute mindfulness group-based technique to alleviate the distress associated with psychosis. Their research resolved this gap, since it demonstrated that a shorter duration exposure to mindfulness was effective in reducing stress, anxiety, and depression [17].
Investigations of how people relate to their psychotic experience found that most of the distress was from their reaction to the psychosis [18,19]. Chadwick and his colleagues introduced the idea that patients were more than their psychosis and that the patient’s core self is good [16,20]. Abba, Chadwick, and Stevenson [21] noted that those who experienced auditory hallucinations were unable to direct and focus their attention. Chadwick et al. [16] and Ratcliffe & Wilkinson [22] both wrote of how depression accompanies anxiety with psychosis, and notably verbal hallucinations.
Experiential avoidance versus mindfulness response
Part of the recovery process is being able to identify how distressing psychosis events and related avoidance behaviors can lead to a relapse [23] Hayes and Wilson [24] referred to the process as “experiential avoidance,” which occurs when the person avoids a distressing situation, and takes steps to change their form, frequency, and context. The process results in more avoidant behaviors to manage the experience. Ruminating about the avoided situation affects judgment in a negative manner [25,26]. The person becomes more frustrated with this behavior, which limits choices [27]. Increased anxiety shapes anticipation and perception of psychosis events [22]. In response to a psychosis event, a person can get stuck in a habitual pattern that maintains their distress and increases the possibility of relapse [28]. Thus, the reaction to the psychosis event is rumination about how they misperceive the event and turn to confrontation.
The core goal is to create a mindful response to the psychosis event. This response enables a person to develop an awareness of the event and begin the process of disengaging from it. The person does not resist the psychosis event, but becomes aware of it, and learns to observe, accept, and let it go. The process of disengaging from psychosis and developing an open attitude towards it is vital when applying mindfulness [29].
The Mindfulness Process
Chadwick adapted techniques from MBSR and MBCT approaches, adding the first minute which involves the body scan. All mindfulness practices are guided, with reminders every few minutes to re-focus on the mindfulness process and not become lost in reactions to psychosis. Homework is encouraged, but not required. Therapeutic process, relationships, and group therapy concepts from Yalom and Leszcz [30] are included in the structure.
Results and benefits from the mindfulness intervention
Benefits of mindfulness training showed significant improvement in the areas of symptom severity, illness insight, functioning, and in the number of hospital admissions [31]. The PBCT process focuses on reducing negative symptoms of affect, reducing positive symptoms of psychosis, and on improved functioning and quality of life [32]. Langer, Cangus, Salcedo, and Fuentos [33] found an improvement in the ability to respond to stressful internal psychotic symptoms and external events. The PBCT approach has been demonstrated to be a powerful technique that reduces the distress associated with psychosis [34] and specifically with the distress associated with auditory hallucinations [22].
Chadwick [11] noted that the mindfulness training results demonstrated a post-intervention reduction in the participants’ feeling controlled by their voices. Regarding delusions, Ellett [35,36] found improvements in levels of distress, preoccupation, anxiety, and depression, and improvements which were maintained at a one-month follow-up, suggesting that mindfulness training can impact cognition and affect associated with paranoid beliefs. Khoury, Lecomte, Gaudiano, and Paquin [37] found that mindfulness interventions were moderately effective in treating psychosis when used as an adjunct to pharmacotherapy. In sum, mindfulness has been beneficial for those suffering from psychosis, as noted by Newman-Taylor and Abba [28], and with adaptations, mindfulness can be safely used with this population.
The aim of the present study was to evaluate the addition of mindfulness, as a new technique to be in a group therapy setting with participants who have a psychotic spectrum disorder diagnosis. Additional focuses are to evaluate scores on depression and anxiety scales, to replicate concepts from Chadwick’s 2005 [16] and 2009 [20] studies, and to determine if participants’ responses were from a mindfulness-based response or from an experiential-avoidance response. The hypothesis was that depression and anxiety scores would drop as participants applied learned skills. Since CBTp alone did not appear to decrease depression, Chadwick [11] believed that mindfulness practices would help alleviate the symptoms of distressing psychosis; in particular, it would alleviate symptoms of anxiety and depression, and demonstrate that Groupbased CBT with mindfulness is a vital intervention that needs to be incorporated as a treatment recommendation.
Mindfulness training as part of group therapy
Participants referred to the outpatient program, were interviewed by a licensed mental health professional and received a diagnosis that included psychosis from the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (American Psychiatric Association, 2013) [38]. The necessary level of care was determined to be outpatient group therapy.
Participants were screened for substance abuse using the CAGEAID and scores had to fall within two or less affirmed questions. Consultation with a licensed addiction and drug counselor was obtained for questionable participants, and all agreed to remain sober and comply with doctor recommendations. A mental status exam was conducted to determine their ability to retain information and apply it. For inclusion, the Columbia Suicide Severity Rating Scale (C-SSRS) scores needed to be between 1 and 3, which indicates a level of care appropriate for outpatient programs.
Upon admission to the outpatient program, participants signed hospital treatment consent and a consent for research. No recruitment was done for this research. Participants’ scores on the PHQ-9 and GAD-7 were taken at admission and discharge. Scores were matched for two sets of data to compare participants who received treatment plus mindfulness and those who received only treatment for the first experiment. The second experiment compared scores that examined different age groups.
The author is a doctoral level licensed clinical psychologist with over 20 years of outpatient experience, has training in CBT, mindfulness, has knowledge of severe and persistent mental illnesses, and conducted the group therapy for all participants. Mindfulness training was measured on a daily and weekly basis over five to 12 weeks. This length of time corresponds to the full duration of the day treatment program. Sessions were 50 minutes long with 10 minutes of mindfulness practice. Only scores from participants who completed a minimum of five weeks were included, which is consistent with the Chadwick [20]study.
Person-Based Cognitive Therapy for Distressing Psychosis by Chadwick [23] was used for treatment conception, but there was not a manual. Five concepts were emphasized. The first concept is how the therapist radically collaborates with the client to meet them where they are. The second concept includes personal growth. It shows how development occurs through a dynamic social and collaborative process within the group explained by Vygotsky’s [39] zone of proximal development, which enhances insight. The third concept demonstrates how the mindfulness intervention builds personal development, awareness, teaches a non-judgmental stance, and acknowledges that others have distress [40]. When distress is experienced, the participants choose to adopt a mindfulness response rather than the experiential avoidance response.
The fourth concept uses the Vygotsky model. It integrates CBT and adapts Ellis’ [41] rational-emotive therapy ABC model and enables participants to recognize that their self-evaluative thoughts are generated by beliefs, which are not facts. Within the group therapy process, participants apply skills, analyze their own experiences with others, and develop a new self-acceptance. The fifth concept involves developing metacognitive insight and integrates learned skills with expressing personal perceptions of change, which teaches how to disengage from distress and accept oneself as a person who can learn and grow [23].
All groups took place in an outpatient Adult Day Treatment program, which met three times each week and included CBT, psycho-educational hours conducted by licensed professionals, and collaborative work with psychiatry. A mental status exam was completed on each participant daily. This was conducted by the author and documented within a hospital progress note; this helped determine their progress and level of stability. Those who completed at least five weeks of training were considered for the experiment.
As part of the mindfulness training, participants completed a oneminute body scan, were taught to observe and to notice where they held tension in their bodies, as recommended in MBSR, MBCT, and PBCT. Then, participants listened to a guided exercise for up to 10 minutes which had a prompt approximately every 30 seconds. This was helpful for those who experience psychosis to remain grounded and present. If they lost their focus, participants were encouraged to refocus on their breathing. Discussions about the use of mindfulness, how participants practiced it at home, and how mindfulness related to CBT skills helped them develop the mindfulness response to distress.
In the group therapy sessions, there were discussions about CBT skills and how they related to mindfulness. This is demonstrated in Figure 1, which was adapted from Chadwick [16]. Learning mindfulness by repetition encouraged participants to observe, accept, acknowledge distressing thoughts, feelings, and symptoms of psychosis, and then disengage, and eventually “let go.” This enabled participants to establish a different relationship with their negative symptoms, depression, anxiety, and psychosis. Concepts of self-compassion were emphasized, including mindfulness, being non-judgmental, staying present, and common humanity, or how others experience suffering.
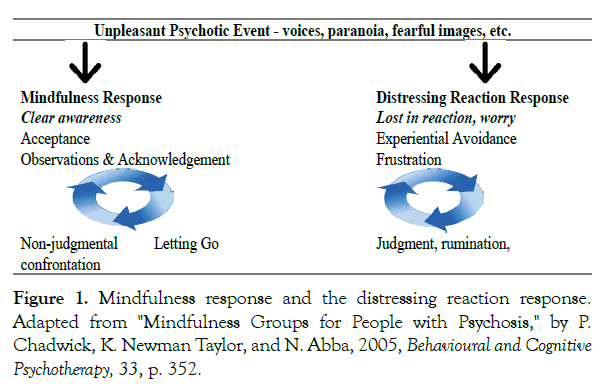
Figure 1: Mindfulness response and the distressing reaction response. Adapted from "Mindfulness Groups for People with Psychosis," by P. Chadwick, K. Newman Taylor, and N. Abba, 2005, Behavioural and Cognitive Psychotherapy, 33, p. 352.
Participants
Approval from the Internal Review Board was obtained from the hospital corporation, Fairview Health Service, University of Minnesota Internal Review Board: STUDY00005035. Informed consent was obtained both verbally and with written materials.
Experiments 1 and 2
A total of 64 participants were involved in Experiment 1. Eligible participants had a DSM5 diagnosis which included: 295.2 Schizophrenia, Catatonia type, 295.3 Schizophrenia, Paranoid Type, 295.4 Schizophreniform Disorder, 295.70 Schizoaffective Disorder, Depressed Type or Bipolar Type, 295.9 Schizophrenia, Unspecified, 296.34 Major Depressive Disorder, With Psychotic Features, 296.54 Bipolar Disorder, With Psychotic Features, 297.1 Delusional Disorder, 298.8 Brief Psychotic Disorder, 298.9 Unspecified Schizophrenia and Other Psychotic Disorders, 301.22 Schizotypal Personality Disorder.
The information in Tables 1 and 2 describe Experiment 1, which compares scores and demographics of two groups: 1A received TAU, and 1B received TAU + mindfulness training. Attrition groups are those who did not complete the program. The TAU included CBT, psychoeducation, psychotherapy, and psychiatric care from the community or the NAVIGATE and First Episode Psychosis program (FEP) at the U-MN.
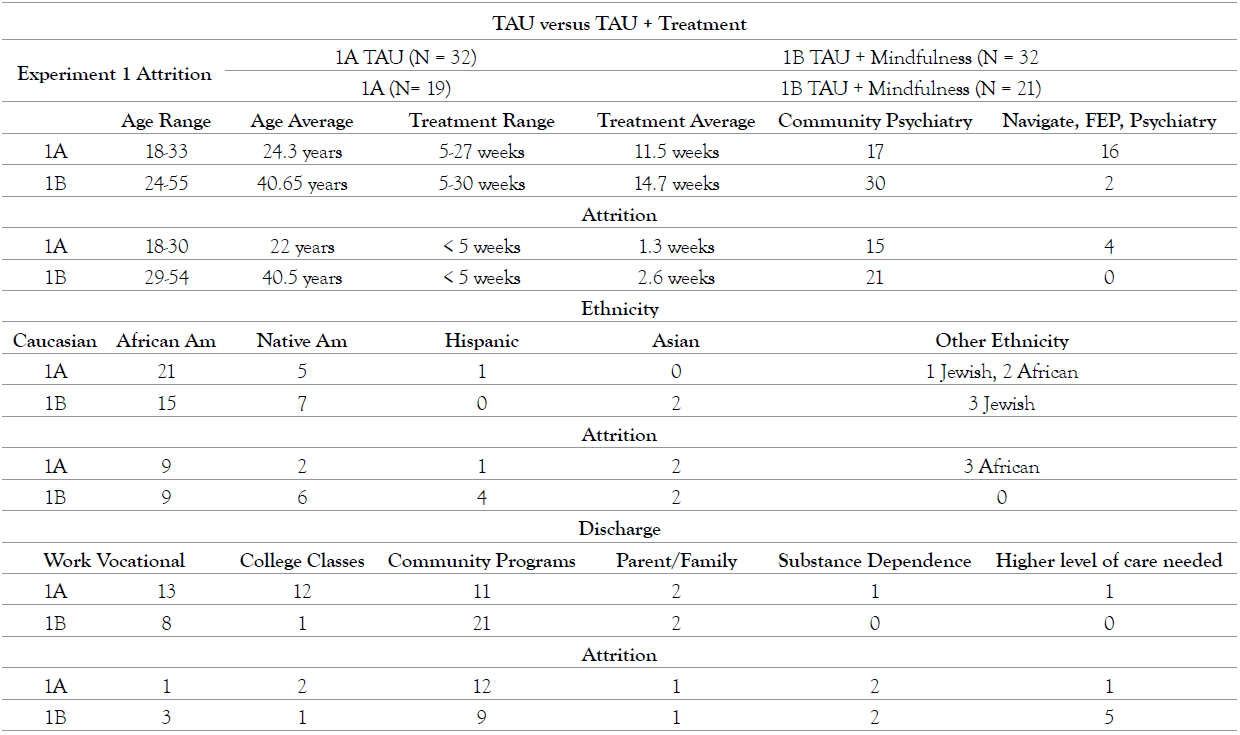
Table 1. TAU + Treatment.
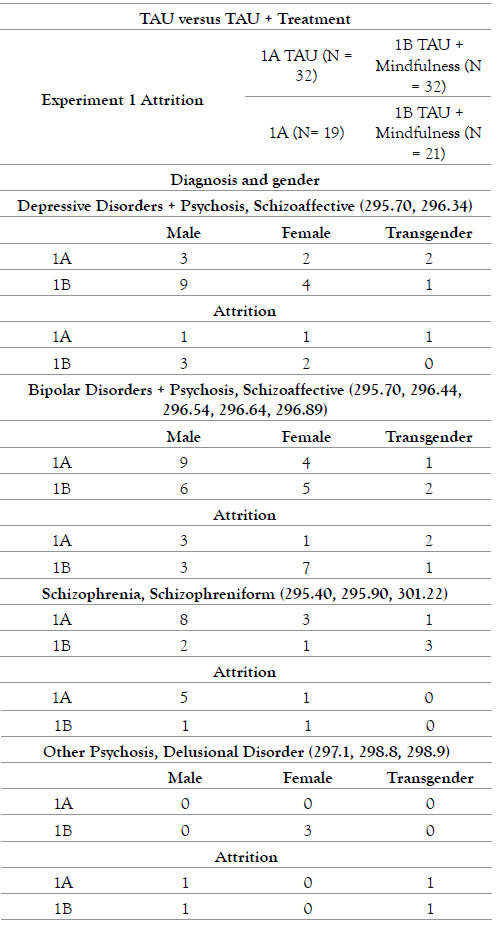
Table 2. TAU + Treatment.
The information in Table 3 describes Experiment 2, which compares scores and demographics of two groups of matched scores, 2A younger, and 2B older, as well as the attrition groups, who did not complete the program. Both groups received CBT, mindfulness training, psychoeducation, psychotherapy, and psychiatric care from the community or the NAVIGATE and First Episode Psychosis program (FEP) at the U-MN.
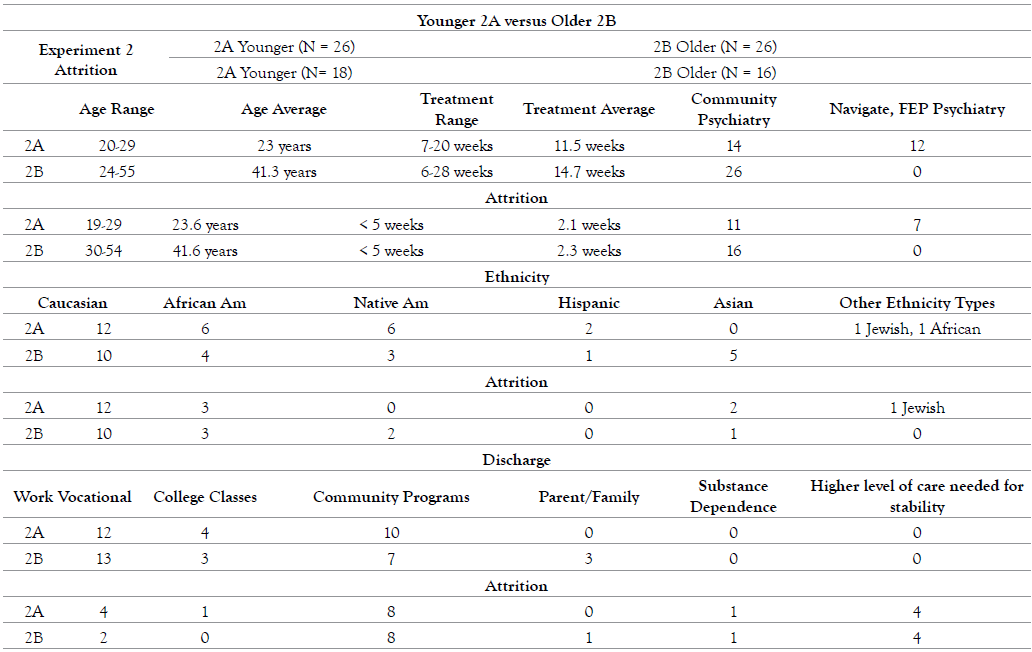
Table 3A. Younger 2A versus Older 2B.
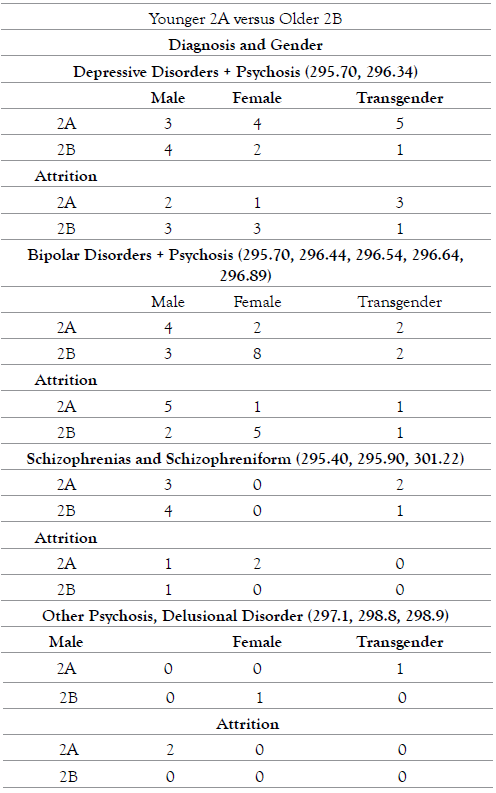
Table 3B. Younger 2A versus Older 2B.
Experiments 1 and 2
The Generalized Anxiety Disorder 7-item scale [42] is a 7-item questionnaire that evaluates levels of anxiety at home, work, and with other people. Participants respond to items on a 4-point scale where 0 = “not at all” and 3 = “nearly every day.” Item responses are summed to create a total score of anxiety. When used as a screening tool, further evaluation for an anxiety disorder is recommended when the score is 10 or greater. The measure has been shown to be a valid and reliable measure of anxiety [43].
The Patient Health Questionnaire-9 (PHQ-9) by Kroenke, Spitzer, & Williams [44] is a 9-item screening for major depressive disorder based on DSM-IV criteria. It is rated on a 4-point scale where 0 = “not at all” and 3 = “nearly every day” for the past two weeks. Item responses are summed to create a total score of depression symptoms. The measure has been shown to be a valid and reliable measure of depression [45].
The Columbia Suicide Severity Rating Scale (C-SSRS), developed by Posner et al. [46], is a suicidal ideation and behavior rating scale which helps determine passive and active suicidal ideation with intent, behaviors, and specific plan. The scale identifies specific behaviors indicative of suicide attempts. Questions are phrased in an interview format to determine the outcome. It has been shown to be valid and reliable [47].
The CAGE-AID [48] is a 5-question tool that assesses severity of drug and alcohol abuse, and if further assessment needs to be done. If two or more questions are affirmative, a complete drug assessment is advised. The measure has been shown to be a valid and reliable measure for substance abuse [49,50].
Experiment 1
A non-standardized, within group comparison was used, since there was open enrollment into the program. The use of a T-test for unequal variances compared pre and posttest scores to determine the effect of the mindfulness intervention on anxiety and depression. A single-factor ANOVA was used to determine differences between the groups (Table 4).
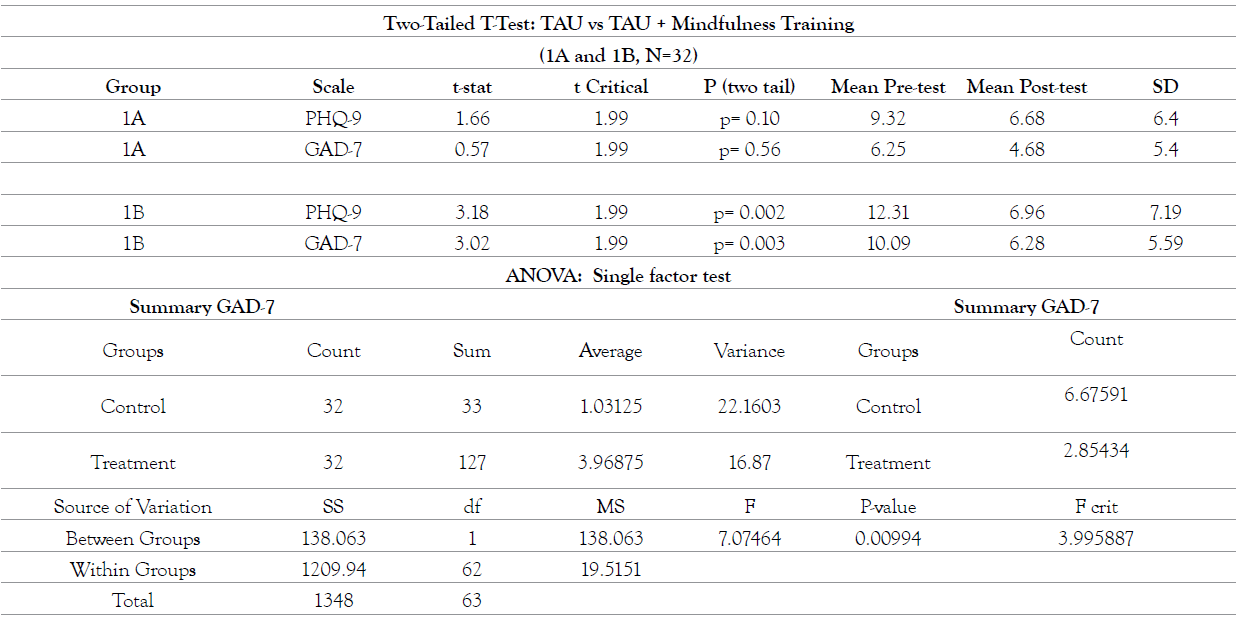
Table 4. Two-tailed T-Test: TAU vs TAU + Mindfulness training.
To determine the differences between and within groups, a single factor ANOVA was conducted. Results indicated that PHQ-9 was not significant with p=0.119, however, the GAD-7 did show statistically significant results with F(1, 62) = 7.0746, p=0.021. The GAD-7 results indicate the impact of the mindfulness treatment upon anxiety levels. Post hoc comparison using the Tukey-Kramer Test indicated a statistically significant effect at p<.05 level for the treatment group, demonstrating the relevance of the mindfulness training in lowering anxiety levels of those diagnosed with psychosis.
Experiment 2
A paired t-test comparing the pre- and posttest means was used to determine the effect of the mindfulness intervention on anxiety and depression. All participants completed the PHQ-9 and the GAD-7 upon admission to the program and at discharge from the program (Table 5).
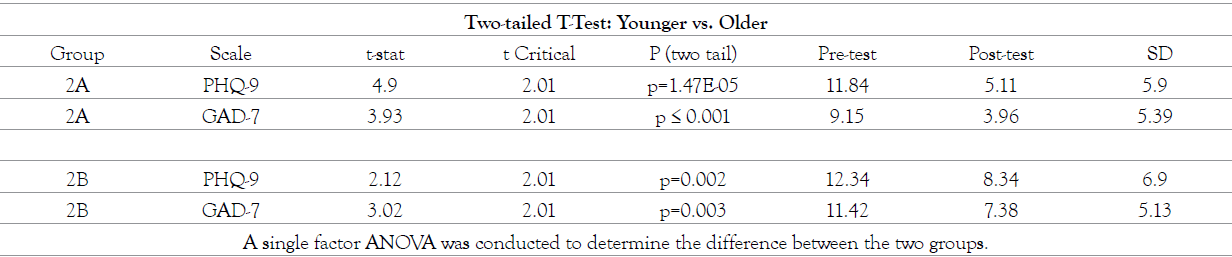
Table 5. Two-tailed T-test: Younger vs. Older.
The PHQ-9 reported F(1, 50) = 2.773, p=0.102, which indicated there were no significant differences between the two groups. The GAD-7 results were: F(1,50) = 0.569, p = 0.451, indicated no differences between older or younger participants.
Experiment 1
When examining the T-tests from the experiment 1, a significant difference from pre to post-test scores was discovered. Scores from participants in group 1A, which received TAU, or CBT, psychoeducation, psychotherapy, and standard psychiatric care did not show significant results, however group 1B, which received TAU plus mindfulness training showed statistically significant results. The 1B finding demonstrates the importance of the added mindfulness training to lower anxiety scores. When comparing within-group and between-group differences, the single factor ANOVA indicated a significant reduction in scores on the GAD-7 anxiety scale, but not the PHQ-9 depression scale. Interestingly, this emphasizes the importance that the training has on mood and how it can impact psychosis symptoms. Many participants with paranoia expressed problems with underlying anxiety which increased symptoms, such as hallucinations, delusions, and paranoia. Mindfulness training lowers anxiety level and allows participants to develop a mindfulness response to the psychosis event. The development enables the participant to become aware of the psychosis event and learn to disengage from it. Thus, the mindfulness training has importance for the development of a mindful response as opposed to the experiential response to distress.
Experiment 2
The second experiment examined the effectiveness of mindfulness training for matched scores from participants that were arranged into a younger and an older group. The T-Test shows significant results for both PHQ-9 and GAD-7 for this comparison, which demonstrates how both benefitted from the therapy that included mindfulness training plus TAU. The single factor ANOVA result was not significant, indicating that both groups benefitted equally.
Participants’ response to mindfulness training
At discharge participants were asked to rank statements about mindfulness training from the most to least important. These items asked about staying present; making observations of thoughts, feelings, images, actions, and psychosis symptoms; letting go; being non-judgmental; understanding triggers; and being able to do reality checks. The participants indicated that “staying present” and “noticing, observing, and accepting the thoughts, feelings, images, and psychosis symptoms” were the most important. This was followed by being non-judgmental, understanding triggers, being able to do reality checks, and letting go. These responses are represented in the previously mentioned model by Chadwick et al. [16], illustrating the mindfulness response as compared to the distressing reaction response.
Participants were also asked to rank the benefits of group therapy using Yalom’s 8 therapeutic factors and they ranked them from most to least important. Participants chose the following factors: Altruism 24%; Catharsis 16%; Instillation of Hope and Self- Understanding, both at 12%; Group Cohesion, and Learning both at 8%; Guidance at 4%.
At discharge from the program, participants reported that they learned from peers to let go of negative thoughts and feelings and see that the psychosis symptom was from the illness and not real. Participants reported making different choices, trusting themselves, and learned how drugs influenced mood and made their paranoia and voices worse. Participants experiencing paranoia and delusional thoughts stated the training took time to learn, but once learned they noticed less anxiety, lower paranoia levels, and could understood the illness in a different way. Participants stated they could complete daily routines, and ignore psychosis symptoms, with continued mindfulness practice at home. They reported being able to disengage from the psychosis and had no adverse effects from the mindfulness training.
Participants that experienced voices reported benefits by being able to disengage from it, understand how their perception was affected by anxiety and depression levels, and could choose their reaction to the event in a mindful way or in an experiential avoidance way. After five weeks of practicing mindfulness training, they stated that they were less disturbed by the symptoms and were able to refocus, so that they could choose their method of response. Participants learned how their response to psychosis events affected their relationships with family, friends, and the community, and felt more empowered by this understanding.
General discussion
The aim of the present study was to evaluate the effectiveness of providing a new technique of mindfulness training in a group therapy format with psychiatric outpatients diagnosed with a psychotic disorder. The rationale for mindfulness training and the specific practice of focused attention to one’s breath and its rhythm was discussed in relation to the participant’s experience of psychotic events. It was expected that mindfulness practices would help lower anxiety and depression levels. The PHQ-9 and GAD-7 were used to determine pretest and posttest depression and anxiety levels. Scores were derived from participants who received mindfulness training plus treatment as usual, and from those who received treatment as usual. The results showed that those who received mindfulness training had lowered levels of depression and anxiety at posttest. The participants that did not receive mindfulness training had a lower level of depression at posttest, but no change in their level of anxiety.
The results of the training are encouraging because there has been limited research on the use of mindfulness with participants diagnosed with a psychotic disorder due to concerns about meditation having the potential to trigger psychosis. However, in the present study, feedback from the participants about the group was positive, and they did not find the process to be harmful. As more is written about using mindfulness practices with patients diagnosed with a psychotic disorder, the idea has become more acceptable; however, access to the treatment remains limited. The therapist who led the group had over 20 years of clinical experience using mindfulness techniques and CBT, and the groups were conducted in an open, accepting, and collaborative manner. This enabled a partnership or alliance to develop with the therapist and among the group participants. Therefore, generalization of this practice to other therapists, approaches, types of meditation, and participants cannot be assumed.
The pretest-posttest design was used to measure the benefits of mindfulness practice in addition to psychiatric care. However, the specific benefits measured were limited to anxiety and depressive symptoms. Future research should include other specific symptombased instruments to measure different dimensions of the psychotic experience, as well as examine the transfer of mindfulness training and practices from the group to the participant’s daily life. In addition, measures such as the Mindful Attention Awareness Scale [51], the revised 12-item Cognitive and Affective Mindfulness Scale [52], and the Five Facet Mindfulness Questionnaire [53] can be used to assess improvements or changes in mindfulness and how mindfulness relates to psychosocial functioning in this population.
The results suggest that the mindfulness training had a statistically significant effect on the level of anxiety and depression of the participants, and that lowering anxiety was beneficial for those who had auditory hallucinations and paranoia, whose selfreports indicated less distress. Participants who completed the mindfulness training reported feeling more confident to return to the community since their anxiety and depression levels had decreased. Certainly, a decrease in anxiety would be considered improvement in psychological functioning, but it is only one aspect of one’s overall functioning, and the intervention was delivered as part of an overall treatment program that included a group process. Participants were able to describe openly their psychosis experiences during the group therapy, and they would ask for advice from other participants about how to manage their psychosis symptoms of voices, images, sensations, and paranoia. The effects of the mindfulness training, discussions, and practice may have contributed to a change in non-psychotic symptoms as well. In this regard, more rigorous empirical investigations are recommended to gain evidence of the effects of mindfulness training on different aspects of the psychosocial functioning of patients with a psychotic disorder.
Implications for practice
Results of the experiments with participants diagnosed with a psychotic disorder show promising results for mindfulness training in a group format and have implications as a beneficial method for decreasing anxiety and depression. Clinicians who work in outpatient psychiatric programs should consider integrating mindfulness training as part of the treatment provided to those diagnosed with a psychotic disorder. If there is no group therapy offered, outpatient programs should consider providing adapted versions of MBSR [1] and MBCT, consistent with the treatment provided in the current study [16].
Clinicians need to have experience conducting therapy groups with this population and learn the mindfulness techniques to provide the training. Once that knowledge is in place, the intervention consists of at least five weeks of sessions twice weekly that include up to 10 minutes of mindfulness training in each session. The aim of the mindfulness intervention is designed to alleviate the patient’s distress associated with psychotic symptoms, not control the symptoms, by learning to separate oneself from the symptoms. In addition to leading the group members in mindfulness exercises, the group therapist has discussions about the practice and benefits of mindfulness, learning to observe, be non-judgmental, acknowledge, and accept distressing psychosis, and how “letting go” helps establish a different relationship with their psychosis. As patients learn to observe their psychosis symptoms and remain non-judgmental, they develop insight which can help them understand and react to their psychosis in a different manner, resulting in a reduction or alleviation of the distress associated with experiencing psychotic symptoms.
The author wishes to acknowledge Daniel Wayne Olson, PhD, and the NIH Clinical and Translational Science Award at the University of Minnesota: UL1TR002494
Clinicaltrials.gov number: NCT04711460
Citation: Lund JD (2021) Mindfulness, Group therapy and Psychosis: Training Decreases Anxiety and Depression in Outpatients with a Psychotic Disorder in a Non-Randomized Within Group Comparison. J Psychol Psychother. 11:388. doi: 10.35248/2161-0487.20.11.388
Received: 29-Dec-2020 Accepted: 07-Feb-2021 Published: 14-Jan-2021 , DOI: 10.35248/2161-0487.21.11.388
Copyright: © 2021 Lund JD. This is an open access article distributed under the term of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.