Journal of Biomedical Engineering and Medical Devices
Open Access
ISSN: 2475-7586
ISSN: 2475-7586
Research - (2020)Volume 5, Issue 1
Local extra cellular water accumulation in a tissue is the essential feature of edema. It is a manifestation of lymphatic stasis as caused by infection, trauma or congenital lymphatic dysplasia. Usually the condition can be graded visually but difficulty persists in quantifying the edema with a non-invasive tool. Near-infrared (NIR) spectral imaging has been shown to be an elegant method to study the edema pathology. It relies on the scattering and absorption of light by the water and its constituents. The instrument presented uses a probe which can be handheld. It contains an infrared light source and a silicon-based detector device. A transmission and a reflection mode are studied. The measurements can be compared to a standard reference or to a previous result. This study confirms that near infrared imaging can be used as a practical, simple, non-invasive tool in the study of edema. This method allows one to follow the evolution or treatment of a clinical condition with edema.
Follow-up edema; Handheld NIR-instrument; Opto-Electrical Transfer Function (OTF)
Near-Infrared Spectroscopy (NIR) can be used to measure the water content of tissues also in edema. Chronic edema affects the morbidity or function of patients with conditions such as chronic wounds or post-nodectomy surgery for tumor. Beginning edema is not seen on the naked eye but it can be mapped before appearance of clinical swelling. There is still a lack of non-invasive technology to practically quantify edema at the bedside. NIR with an extensive technology has been used to measure hydration of normal skin [1] and at burn injury [2]. Beyond medicine, such systems have been used in agriculture, in food industry and in cosmetology for assessment of the moisture content of skin [3]. In this article, the authors present a simple, hand-held gadget quantifying the water content.
The electronic measuring device contains a probe that gently rests on the subject’s skin or even better, is glued there with double sided transparent tape. The unit consists of an infrared (IR) light source optically separated but adjacent to a phototransistor, both with the maximal sensitivity at 970 nm (Figures 1A and 1B). An IR-led emits light, what is reflected on the skin and is detected by a phototransistor. The small probe (1.5 cm diameter) contains the IR-led and the optically separated phototransistor. The main box controls the light power for the depth of penetration and another switch selects the sensitivity of the signal. A standard voltmeter indicates Vexit, leading to OTF, the translucency factor. The instrument is a self-made version and the average cost would be beneath $100. The light source is conceived as follows (Figure 2). Technically Vi has 4 settings (1 – 4) to be selected for the power of the IR LED (L970-33).
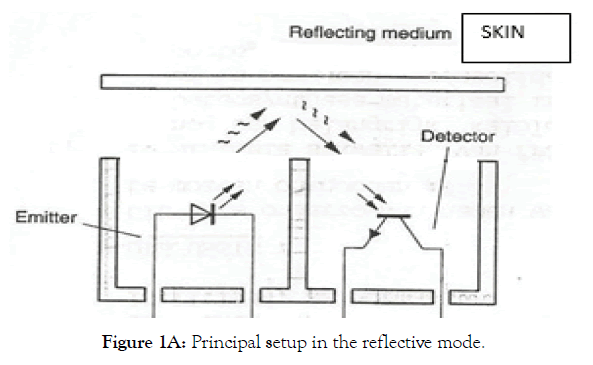
Figure 1A: Principal setup in the reflective mode.
Figure 1B: Photography of the instrumentation.
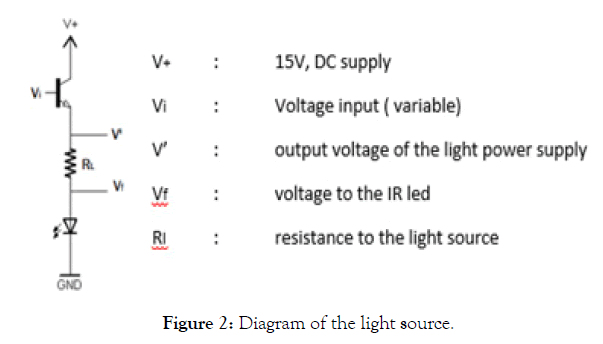
Figure 2: Diagram of the light source.
(RL = 330Ω, V+ = 15V)
The electrical power (P) of the light source is:
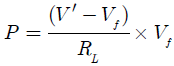
This intensity (P) determines the depth of penetration, which can be been measured and is related to the different layers of the skin (Table 1). The light in the intervening tissues cannot go through in a straight way and will undergo multiple reflections and absorptions in the structured elements of skin before exiting. A significant portion of that light is captured by the detector. The resulting electrical signal is amplified as needed and is read-out at a voltage meter for further processing (Figure 3). The light sensor is schematized in Figure 4. The light sensor is a phototransistor (PT534) which is connected as given in Figure 4.
| Vi Light Power – Setting | Vi | P.10-3 (W) | Depth of penetration (mm) | Location |
|---|---|---|---|---|
| 1 | 1.85 | 1.14 | 1.65 | Superficial dermis (ID) |
| 2 | 2.50 | 3.18 | 3.30 | Deep dermis |
| 3 | 4.67 | 10.60 | 6.60 | Upper hypodermis |
| 4 | 10.50 | 30.12 | 10.60 | Deep hypodermis (SC) |
Table 1: Intensity of NIR light and depth of penetration.
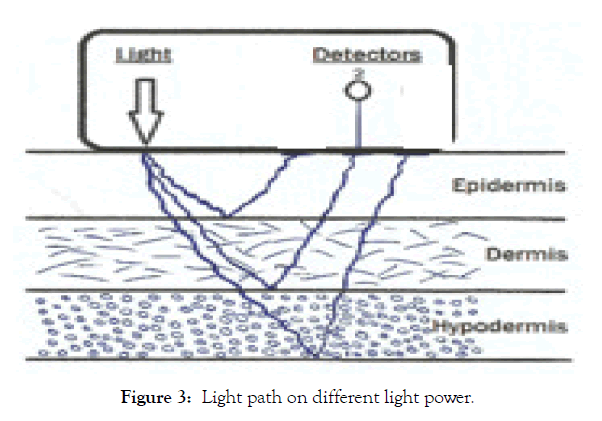
Figure 3: Light path on different light power.
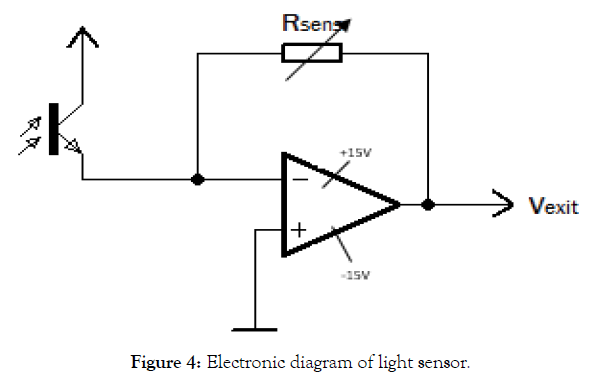
Figure 4: Electronic diagram of light sensor.
Rsens: The sensitivity of the sensor phototransistor
Vexit: Voltage related to the incident light intensity
Rsens, Expressed in KΩ has 4 settings for sensitivity (Table 2).
| R Sensitivity -setting | Rsens (KΩ) |
|---|---|
| 1 | 120 |
| 2 | 180 |
| 3 | 240 |
| 4 | 300 |
Table 2: Sensitivity of the detector.
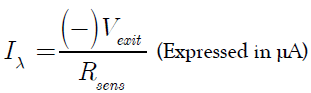
The light received Iλ is linear to the light emitted P.
The sensitivity of the light detector is given by the electrical power Iλ through it.
The opto-electrical transfer function (OTF) is expressed in units and means the intensity of the received light (Iλ) per light emitted (P). This can be done in the reflective (RTF) or in the transmitted mode (TTF). OTF is the general term for RTF or TTF and means the IR-translucency to light.
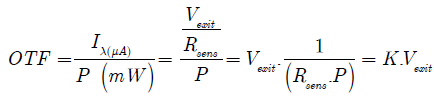 For practical purpose we multiply K with 10³.
For practical purpose we multiply K with 10³.
 A list of values is included in Table 3A and Table 3B.
A list of values is included in Table 3A and Table 3B.
| Setting of power | Light Intensity (mW) P | K’ factor |
|---|---|---|
| 1 | 1,14 | 7,30 |
| 2 | 3,18 | 2,62 |
| 3 | 10,60 | 0,79 |
| 4 | 30,12 | 0,28 |
Table 3A: K’ for different light intensities at the sensitivity of sensor Rsens = 120KΩ
| Setting | Rsens | K’ |
|---|---|---|
| 1 | 120K | K’ |
| 2 | 180K | K’ x 0,67 |
| 3 | 240K | K’ x 0,50 |
| 4 | 300K | K’ x 0,40 |
Table 3B: K’ at difficult settings of Rsens.
Art 1: Effect of distance between light source and sensor
The experimental in vitro work is done on fresh commercial chicken legs at room temperature. Normal saline and other fluids are injected subcutaneously in different quantities, imitating edema. The intensity of the diffusely reflected or transmitted NIR light is measured. The increase of light path through the tissues gives information on tissues crossed (Figure 3).
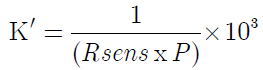
The setting (0) of 1.5 mm is not used because most of the incident photons bounce back as specular reflectance without spectral information of the tissue [4]. Some light is also absorbed in the epidermis and corneal layers of the dermis and is wasted for the study. Depending on the thickness of the tissue the settings 2 and 3 measure the interesting layers of the dermis and setting 3 even penetrates into the hypodermis. It is obvious that with lighter emitted (P) a higher Vexit is obtained. Vexit decreases on a wider distance between emitter and receptor (Figure 5).
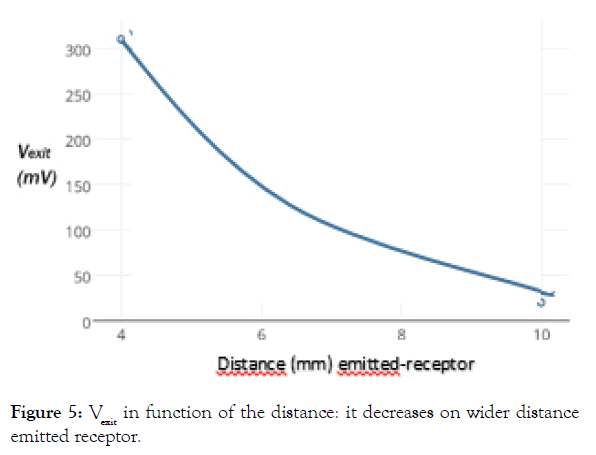
Figure 5: Vexit in function of the distance: it decreases on wider distance emitted receptor.
Art 2: Effect of water content as imitation of edema
For imitation of edema, normal saline is infused SC below the skin surface of a chicken leg. The diffusely reflected light is measured as Vexit and is expressed as OTF. For the different quantities of fluid infused we measured OTF as seen in Figure 6, at the depths 1 to 4 as listed in Table 1. For the depth (Setting 4) more light is applied and is reflected proportionally, than on the surface (Setting 1) for the same quantity of fluid (ml) infiltrated.
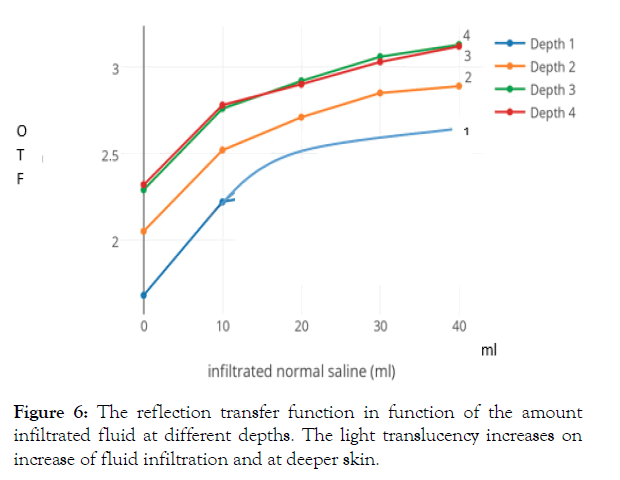
Figure 6: The reflection transfer function in function of the amount infiltrated fluid at different depths. The light translucency increases on increase of fluid infiltration and at deeper skin.
On subcutaneous fluid infiltration of 10cc of normal saline, about 10% more light is reflected at all depths and this process continues on further fluid infiltration. The change in reflection occurs gradually over 10 minutes, with most of it within 2 minutes.
We have the impression that on fluid infiltration the reflective and scattering structures, as collagen fibers and cells, are dispersed, allowing this way the light to shine through better and so to be reflected more. On the contrary on straight light transmission, the received infrared light decreases at the increase of fluid infiltration (Figure 7). The TTF in function of the infiltrated amount of normal saline of fluid decreases with the amount of injection, due to the increase in quantity of the translucent medium.
Figure 7: Transmission transfer function in function of the amount of infiltrated fluid. Translucency decreases on more infiltration fluid and at the superficial skin.
Art 3: Effect of different fluids for subcutaneous infiltrations
SC water increases the intensity of light reflectance. At 650 nm and at 950 nm the increase is around 10% for SC infiltration of 10 ml. On transmission we noticed a decrease; moistering the skin already decreases the exit voltage. It acts as an additional filter for the IR light. We found no difference on the exit voltage of reflectance between normal saline or plain water.
SC injection of 10 ml of a 20% sugar solution also increases the exit voltage for about 10%, the same as for water. On the contrary, an injection of 10 ml of a 20% NaCl solution gradually decreases the exit voltage for 10% at 20 minutes and 20% at 1.5 hours. This is due to a sol/gel transition of the colloid nature of the tissue which changes in the presence of electrolytes, jellifying the plasma.
In order to imitate edema more closely, we infiltrated the chicken leg skin with human plasma [5]. The effect matches the infiltration with normal saline or water, causing a similar increase of OTF (Figure 8). However subcutaneous infiltration with 2.5 ml uncoagulable EDTA-treated blood decreases the OTF at all depths due to presence of microscopic of structured elements (Table 4). Ethylene glycol decreases Vexit a little, for reflection on all depths. Kitchen oil also decreases the reflection of light. For red light the decrease is around 10%, for infrared light the decrease is even 20%. We noticed here that in the transmission mode the light intensity increases. The effect of gasoline approaches the effect of water and also increases the OTF around 10% on an infiltration of the 10 ml fluid.
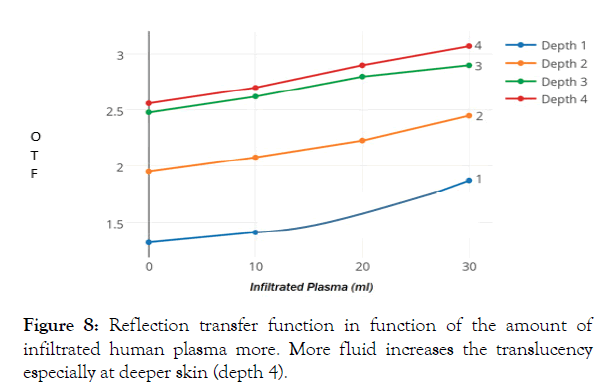
Figure 8: Reflection transfer function in function of the amount of infiltrated human plasma more. More fluid increases the translucency especially at deeper skin (depth 4).
| Pemitter / Rsens = 120KΩ | OTF Normal | OTF Blood Infiltrated |
|---|---|---|
| 1 | 3.70 | 2.48 |
| 2 | 5.07 | 3.28 |
| 3 | 6.11 | 3.91 |
Table 4: Diluted blood decreases OTF significantly.
Art 4: Effect of temperature
Chicken legs and the IR sensor are kept together at the different temperatures. The measurement of OTF between 10°C and 30°C varies around 25% at all depths (Figure 9). On increased temperature the measurement of light reflectance seems to decrease. However, we noticed that the collector power dissipation of the phototransistor PT534 also decreases linearly at the temperatures studied. Obviously, there cannot be a physiological difference on a small temperature change in a dead tissue and the changes must be caused by the effect of temperature on the instrumentation. Indeed, similar measurements were seen at different temperatures applied only to the IR sensor without a tissue.
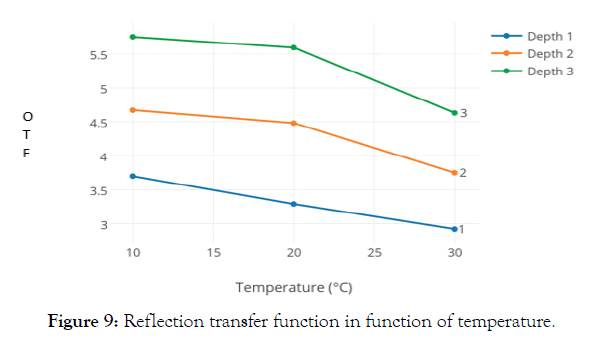
Figure 9: Reflection transfer function in function of temperature.
Art 5: Effect of pressure
For practical purposes the effect of pressure to the sensor overlaying the skin is important. These measurements were done on human volunteers. The effect of direct pressure is done by a blood pressure cuff applied over the device at the upper arm and is expressed in OTF for the reflective mode (Figure 10). We noticed that a direct pressure to the sensor increases the light reflection for 40% at the surface (Setting 1) and 34% for the deeper tissues (Setting 3). For this reason, we decided in the clinical measurements to glue on the sensor to the tissues rather than to press it on. The occlusion of the upper arm by a blood pressure cuff, applied proximally to the measuring device increases the OTF, making the tissues more translucent. We presume this is due to the decrease of circulating red blood cells.
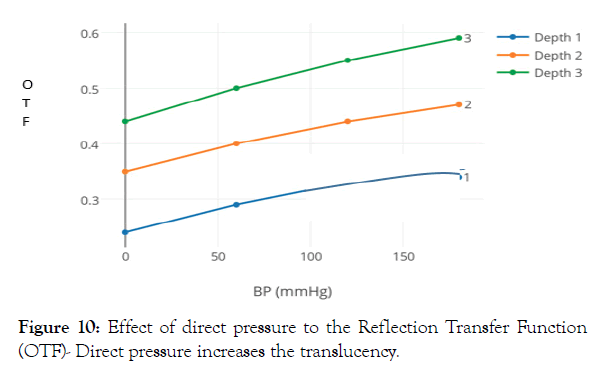
Figure 10: Effect of direct pressure to the Reflection Transfer Function (OTF)- Direct pressure increases the translucency.
This clinical part is a pilot study in the reflective mode on a large variety of healthy patients with only localized edema. Local control is eventually done on a contralateral skin surface. Measurements of the perimeters at the limbs are eventually performed bilaterally for comparison and later reference.
Art 1: Blepharoplasties
Measurements of a typical case: We noticed that the swelling decreases the light reflection in OTF. The OTF and the aspect also are normalized again in 3 weeks (Table 5).
| Variables | Light Power Setting 1 | Light Power Setting 3 | ||
|---|---|---|---|---|
| Left | Right | Left | Right | |
| Pre-op | 3.04 | 3.33 | 5.75 | 6.14 |
| 1 week post-op | 1.59 | 2.57 | 3.30 | 4.46 |
| 3 weeks post-op | 3.00 | 3.27 | 5.71 | 6.00 |
Table 5: On blepharoplasty, swelling and OTF normalize in time.
Art 2: Venous phlebitis
Measurements below the knee: With medical treatment the situation at the pathological side improved within 2 weeks. We noticed that in phlebitis the circumference of the leg increases and the OTF decreases markedly. On healing the OTF increases again and precedes the clinical improvement with normalization of leg perimeter (Table 6).
| Depth | OTF end of pregnancy | OTF 1 month after delivery |
|---|---|---|
| 1 | 2.06 | 3.03 |
| 2 | 3.14 | 4.57 |
| 3 | 3.99 | 5.48 |
| 4 | 4.17 | - |
Table 6: Gradual improvement of phlebitis of lower leg, with decrease in circumference and increase in OTF.
Art 3: Breast augmentation
The infiltration of local anesthesia before surgery increases also the local swelling and so the OTF. 1 week after breast implant, there was no more swelling and the OTF of the skin became again almost normal.
Art 4: Hand trauma
This elderly lady fell on her left hand and the RX examination did not show a fracture. Nevertheless, she had a significant swelling and pain at the dorsum of the hand with decreased OTF.
Measurements: (Table 7)
| Below Knee | Above Knee | Above Knee | |||
|---|---|---|---|---|---|
| Circumference 26.5 cm | Normal Side | Circumference 33.5 cm | Pathological Side | Circumference 31.5cm | Pathological side after 2 weeks |
| Depth | OTF | Depth | OTF | Depth | OTF |
| 1 | 2.19 | 1 | 0.94 | 1 | 2.10 |
| 2 | 2.96 | 2 | 1.34 | 2 | 2.86 |
| 3 | 3.63 | 3 | 1.60 | 3 | 3.65 |
Table 7: Pain and swelling gradually decreased with increase in OTF and almost normalized in one month.
Later on, pain and swelling gradually decreased with increase in OTF and they almost normalized in a month later.
Art 5: Arthrosis (slight) of ankle
OTF is significantly decreased and the ankle was slightly swollen.
Art 6: Edema after lymphatico-venous reconstruction
This lady had a lymphomatous swelling of the left leg what was treated with a groin dissection. Because of hindering swelling she had twice a lymphatico-venous reconstruction. 6-month postop significant swelling of the leg persisted with decreased OTF above the knee (+5 cm) and below (-10 cm).
Although the patient feels some improvement and had a lowered OTF, she had a long way to go.
Art 7: Edema in pregnancy
A few days before delivery we measured the OTF at the swelling of the ankles and compared it 6 months after delivery (Table 8).
| Normal Right Hand | Traumatized Left Hand | Traumatized Left Hand After 1 month | |||
|---|---|---|---|---|---|
| Depth | OTF | Depth | OTF | Depth | OTF |
| 1 | 2.38 | 1 | 1.58 | 1 | 2.13 |
| 2 | 3.07 | 2 | 2.16 | 2 | 2.80 |
| 3 | 3.84 | 3 | 2.83 | 3 | 3.43 |
Table 8: The swelling at the ankles at the end of the pregnancy causes a temporary drop in OTF.
The presented method for measurement of edema is a single point technique with diffusely reflected NIR light. An extension would be an imaging device with a camera which takes a digital image of a large area of interest from a suitable distance. We also performed studies with NIR light transmission where the light source and the sensor were inserted in the area of edema. These experiments cannot be applied clinically and do not allow repeated measurements. The majority of accepted techniques are invasive. Wet-to-dry measurement requires a tissue sample to be desiccated; lymphography and fluorescent techniques are more difficult. Popular non-invasive methods include limb circumference changes and electrical ohmic measurements. These techniques do not measure a water content directly. However, NIR measures the content of free water from the simple reflectance of light at superficial skin layers and as captured at a silicon-based detector of 970 nm, typical for a chemical OH-stretch.
Clinically the water content of tissue indicates the degree of hydration. Previous studies have shown that the main edema fluid is located at the subcutaneous level. This implies that in a burn injury with edema mainly the deeper skin layers are affected [2].
Theoretically on transmission of light, plain water absorbs an intensity proportional to the length of the light path (d), according to the well-known Beer-Lambert law:
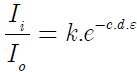
In a biological multilayered medium as skin, scattering of light will occur on all organic structures as red blood cells, cell particles and especially collagen fibers. The light measured is the sum of a spectrum due to the water in the tissue, the scattering due to tissue components and a baseline offset. This changes the above absorption formula somewhat.
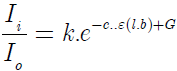
l.b. is the adjusted length of the optical path of complex scattering (b=2 to 5)
G is a correction factor for the diffraction
The indirect reflection of light needs scattering on structured elements before diffusely exiting to the photodetector. However, the light has to come first through the tissues by transmission what implies that finally reflection and transmission are interrelated. This is called transflectance.
We noticed that light reflection decreases on thicker fluids as oil and glycerin. It increases on thinner fluids as water or gasoline. The scattering is reduced in edema due to the dilution by all the surrounding structural elements in the tissues especially collagen fibers. Other involved structures are several types of cells a.o. white blood cells. Edema fluid also contains a significant portion of floating cellular and subcellular fragments. According to the "Mie scattering theory” [6], the diffuse reflectance increases sharply on the decrease of the microscopic diameter of fragments. From this study it became obvious that edema fluid is not only water. A subcutaneous increase in fluid increases the OTF-value of reflectance whereas in any type of edema, OTF decreases much alike a SC-infiltration with diluted blood.
A disadvantage of NIR measurement is the great number of variables contributory to the reflected spectrum. Measurements are influenced a.o. by the color, the particle size and composition of the sample. Therefore, precise analysis needs a very specific site of calibration as reference method. So, the method does not follow an absolute mathematical scheme. The results are relative to a set example.
Because edema implies the accumulation of extra-cellular water, we would expect that the reflective OTF of the applied light should be increased. However, we noticed that it is decreased in all clinical cases. This is seen a.o. in post-op swelling of blepharoplasties, after trauma, on thrombophlebitis. Dermal scattering is reduced in edema due to the interference of structured elements with a decrease of OTF [5]. The same applies to some extent to the infiltration with diluted blood.
Seroma and hematoma at the deeper tissues cause no NIR change at the surface; such a deeper fluid collection should be detected through other means as ultrasonic US-echography. Considering the importance of the microscopic constituents of edema, one can speculate on a more adequate therapy for superficial recent edema before its fibrotic alteration.
This method of NIR measurement can quantify edema in standardized conditions. Medical applications are multiple and can guide therapy or allow following the evolution of an edematous condition. The decrease in diffusely reflected NIR light of 970 nm quantifies the degree of edema of superficial tissues. Edematous fluid is optically closer to diluted blood than serum or plasma. This is due to the microscopic structures contained and makes it essentially different from plain fluids.
• There was no sponsorship for this study. Measurement was done at the office of the author.
• The author has no financial interest in relationship to the content of this research article.
• The study was approved by the local institutional medical committee.
• The principles outlined in the Declaration of Helsinki have been followed.
• All participating patients gave written informed consent for the unanimously usage of the measurements in this study.
We thank J. Vandepitte, MD - Pathologist and E. S’Heeren, MS - Chemistry for proofreading the text and for their valuable commentary. Vandeput M, MS – Economy took care of the secretarial work.
Citation: Vandeput JJ (2019) Measurement of Near-Infra-Red translucency for Evaluation of Edema. J Biomed Eng Med Devic 4:140. doi: 10.24105/2475-7586.4.140.
, DOI: 10.35248/2475-7586.20.5.140
Copyright: © 2019 Vandeput JJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.