International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Review Article - (2023)Volume 11, Issue 10
Heart failure is a pervasive and debilitating condition that demands a holistic approach to management. Cardiac rehabilitation has emerged as a vital component of this continuum of care, aiming to enhance patient well-being through structured interventions. This review article provides a comprehensive exploration of the journey from in-hospital care to post- discharge support, shedding light on key insights that shape heart failure management. Highlighting the acute management of heart failure, the role of multidisciplinary teams, pharmacological strategies, and vital cardiac function assessments are detailed, providing the foundation for comprehensive care. Components of cardiac rehabilitation has the closer look at exercise therapy, nutritional counseling, medication optimization, psychological support, and patient education underscores the holistic approach that rehabilitation programs embrace. We explore the vital role of structured exercise programs and educational interventions within hospital settings, along with strategies to promote patient adherence. Recognizing the pivotal role of post-discharge care, we underscore the importance of personalized care plans and seamless patient information transfer. Outlining outpatient, home-based, and telehealth rehabilitation options, we examine the growing role of caregivers and family support in sustaining progress. The review delves into key performance indicators, patient progress monitoring, and outcomes data analysis, essential for evaluating program effectiveness. Common challenges in program implementation and strategies for overcoming disparities in access are discussed, acknowledging the need for innovative solutions. As we glimpse into the future, emerging technologies, research initiatives, and the potential for personalized treatment approaches in cardiac rehabilitation are explored. In closing, we recap the critical insights gleaned, affirming the significance of comprehensive cardiac rehabilitation in heart failure management. A call to action echoes through these pages, urging healthcare providers and policymakers to prioritize and evolve rehabilitation as an essential pillar in heart failure care.
Cardiac rehabilitation; Heart failure; Chronic heart disease; Cardiac exercise therapy; Multidisciplinary care; Post-discharge support; Cardiopulmonary rehabilitation; Rehabilitation programs; Exercise training; Pharmacological management; Patient education; Nutritional counseling; Psychological support; Outpatient rehabilitation
Heart Failure (HF) is a chronic and progressive clinical syndrome characterized by the inability of the heart to pump enough blood to meet the body’s metabolic demands. It is a global health problem, affecting over 64 million people worldwide, with a prevalence of 2%-3% in the general population [1]. The prevalence of HF increases with age, and it is estimated that 10% of people over the age of 65 will develop HF [2].
Cardiac rehabilitation has emerged as a pivotal and multifaceted approach to addressing heart failure. Beyond traditional pharmacological treatments, cardiac rehabilitation offers a holistic method to enhance the well-being of heart failure patients. It combines structured interventions, including exercise therapy, nutritional counseling, medication optimization, psychological support, and patient education, to improve patient outcomes and quality of life [3].
The purpose of this review article is to provide a comprehensive exploration of the role of cardiac rehabilitation in managing heart failure. We will delve into the key insights and developments that shape heart failure management, focusing on the journey from in-hospital care to post-discharge support. By identifying these critical aspects, we aim to underscore the significance of cardiac rehabilitation as a foundation in improving the lives of individuals living with heart failure.
Heart failure and cardiac rehabilitation
Heart failure, a multifaceted cardiovascular condition characterized by the heart’s inability to effectively pump blood to meet the body’s demands, encompasses a spectrum of classifications, ranging from preserved ejection fraction (HFpEF) to reduced ejection fraction (HFrEF). Understanding these classifications is fundamental in creating effective management strategies for heart failure patients [2].
Cardiac rehabilitation, an essential part of modern heart failure management, is designed with specific goals in mind. Beyond the traditional focus on symptom relief and disease management, it aims to optimize the physical, psychological, and social well-being of patients. These goals encompass improving exercise tolerance, enhancing quality of life, reducing hospital readmissions, and minimizing the overall burden of heart failure [4].
While cardiac rehabilitation is now recognized as an integral component of heart failure care, its historical evolution defines its enduring relevance. Over the decades, cardiac rehabilitation has transformed from a specific intervention to a well-established and evidence-based approach [5]. This historical perspective underscores its ability to adapt and remain a crucial asset in addressing the evolving challenges posed by heart failure in modern healthcare. By understanding the definitions, classifications, goals, and historical context of cardiac rehabilitation, we can better appreciate its pivotal role in the comprehensive management of heart failure patients [6].
Exercise intolerance in HF is due to reduced exercise capacity, which is often estimated using screening tools like the NYHA classification or tests at submaximal effort like the 6-minute walk test. The most accurate measure of exercise capacity is peak oxygen consumption, also known as maximal aerobic capacity or peak VO2. This is the amount of oxygen that the body can consume at maximal effort. Peak VO2 can be measured during Cardiopulmonary Exercise Testing (CPX), which is a standard first step after referral to cardiac rehabilitation. CPX measures a number of physiological parameters, including heart rate, blood pressure, and oxygen consumption. Peak VO2 is calculated using the Fick equation, which is a mathematical equation that describes the relationship between cardiac output and oxygen consumption [7].
Peak VO2=(HR × SV) × [C(a-v) O2]
Where, HR=Heart rate; SV=Stroke volume; C(av)=The difference in arterial and venous oxygen concentration. Peak VO2 is often reported in mL/kg/min to allow for comparisons between people of different weight.
In-hospital care for heart failure patients
In the critical phase of heart failure management, which begins with hospitalization, the focus is on acute management and stabilization. This stage involves a concerted effort to alleviate symptoms, optimize hemodynamic stability, and address potential life-threatening complications. Physicians and healthcare teams employ a range of interventions to achieve these objectives, including diuretics to alleviate fluid overload, vasodilators to reduce afterload, and inotropic agents to improve myocardial contractility [8]. One key aspect of in-hospital care is the collaborative approach facilitated by multidisciplinary teams. Cardiologists, nurses, dietitians, physiotherapists, and psychologists work in concert to provide comprehensive care. This interdisciplinary approach ensures that not only the physical symptoms but also the psychosocial aspects of heart failure are addressed, promoting a more holistic and patient-centered approach to care [9].
Pharmacological interventions are another important aspect of in-hospital care for heart failure patients. Physicians carefully select medications based on the type and severity of heart failure, aiming to alleviate symptoms, reduce cardiac workload, and improve overall cardiac function. These treatments may include ACE inhibitors, beta-blockers, aldosterone antagonists, and angiotensin receptor blockers, among others [2].
In addition to medication management, continuous monitoring and assessment of cardiac function are integral components of in-hospital care. Physicians and healthcare teams employ various diagnostic tools, such as echocardiography and hemodynamic monitoring, to evaluate cardiac performance, identify any potential complications, and adjust treatment strategies accordingly. In-hospital care for heart failure patients is a critical phase in their management journey. It encompasses acute interventions to stabilize patients [10].
Components of cardiac rehabilitation
Cardiac rehabilitation programs offer a comprehensive and multifaceted approach to managing heart failure, with several key components at the forefront of patient care.
Exercise therapy and physical conditioning form a core component of these programs. Change in exercise regimens help patients improve their cardiovascular fitness, strengthen their muscles, and enhance their overall physical capacity. This not only contributes to symptom relief but also plays a fundamental role in boosting patients’ confidence and quality of life [11].
Dietary and nutritional counseling is another vital aspect of cardiac rehabilitation. Nutritionists and dietitians work closely with patients to develop individualized dietary plans that promote heart-healthy eating habits. These plans are designed to manage fluid retention, control sodium intake, and optimize nutritional status, all of which are essential for heart failure management [12].
Medication management and optimization are integral components of cardiac rehabilitation. The review and adjustment of medications ensure that patients receive the most effective pharmacological therapies to control heart failure symptoms, reduce the risk of exacerbations, and improve cardiac function [12].
Psychological and emotional support is dominant in addressing the psychological burden often associated with heart failure. Patients may experience anxiety, depression, or stress related to their condition. Counseling and support groups provide avenues for patients to cope with these emotional challenges, promoting overall well-being [12].
Education and lifestyle modification complete the holistic approach of cardiac rehabilitation programs. Patients receive information about heart failure management, symptom recognition, and self-care strategies. Lifestyle modifications, including smoking cessation, weight management, and adherence to a heart-healthy diet, empower patients to take an active role in their recovery and long-term well-being (Figure 1) [12,13].
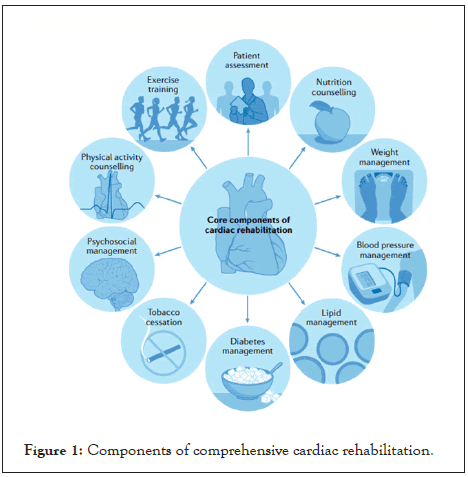
Figure 1: Components of comprehensive cardiac rehabilitation.
Intra-hospital cardiac rehabilitation programs
In-hospital care is not only about acute interventions but also represents an opportune moment to initiate elements of cardiac rehabilitation. Intra-hospital cardiac rehabilitation programs play a important role in the holistic management of heart failure patients during their hospital stay [14].
Structured exercise programs during hospitalization are a cornerstone of intra-hospital cardiac rehabilitation. These programs are modified to each patient’s condition, focusing on early mobilization, gradual physical conditioning, and safety. Engaging patients in supervised exercises within the hospital setting not only contributes to improved cardiovascular fitness but also encourages them to appreciate the benefits of physical activity in their recovery journey [4].
Patient education and counseling are equally vital components of intra-hospital cardiac rehabilitation. During their hospital stay, patients are educated about heart failure, its management, and lifestyle modifications. This empowers them with knowledge and skills needed to make informed decisions about their health. Additionally, counseling sessions provide opportunities for patients to discuss their concerns and gain valuable insights into managing the emotional aspects of their condition [15].
Strategies for promoting adherence to rehabilitation protocols are integral to the success of intra-hospital programs. Healthcare teams work collaboratively with patients to set realistic goals and develop personalized rehabilitation plans. Establishing rapport and trust is key, as it fosters a sense of partnership between patients and their healthcare providers. Furthermore, involving family members and caregivers in the rehabilitation process can enhance patient motivation and adherence [3].
The transition from in-hospital care to post-discharge is a pivotal phase in the management of heart failure patients, and it carries immense significance for their long-term well-being. This segment of the review article underscores the essential components of this transition.
Transitioning to post-discharge care
The importance of post-discharge care in heart failure management cannot be overstated. It represents the bridge between acute intervention and ongoing support for patients living with heart failure. During this phase, the focus shifts from stabilizing acute symptoms to equipping patients with the tools and resources they need to manage their condition effectively in the community. Post-discharge care aims to reduce the risk of readmissions, optimize medication adherence, and promote overall patient autonomy [16].
Developing personalized care plans for heart failure patients is a central aspect of this transition. Recognizing that each patient’s journey with heart failure is unique, healthcare providers work collaboratively with individuals to design care plans tailored to their specific needs and circumstances. These personalized plans encompass medication regimens, dietary recommendations, exercise routines, and strategies for monitoring symptoms. Such customization empowers patients to actively participate in their care and adhere to their prescribed therapies [8].
Fundamental to the success of post-discharge care is the seamless handover of patient information and coordination with outpatient facilities. Timely and accurate transfer of medical records, treatment plans, and follow-up appointments ensures continuity of care. Effective communication between hospital- based teams and outpatient providers is the most important, allowing for a smooth transition and minimizing disruptions in care delivery. This coordination fosters a patient-centric approach that places the individual’s well-being at the forefront of heart failure management [17].
The continuum of care for heart failure patients extends far beyond the confines of the hospital, and this phase of the review article highlights the critical elements of post-discharge support that contribute to long-term success in managing this complex condition [18].
Post-discharge support
Outpatient cardiac rehabilitation programs play a pivotal role in post-discharge care. These structured programs offer a structured and supervised environment for patients to continue their recovery journey after leaving the hospital. They typically include exercise therapy, education, and ongoing support, with healthcare professionals monitoring progress and adjusting treatment plans as needed. Outpatient rehabilitation not only enhances physical fitness but also provides patients with a sense of community and ongoing guidance in managing their condition [10].
For some patients, home-based rehabilitation options provide a convenient and effective means of post-discharge support. These programs are designed to cater to individuals who may face barriers to attending outpatient sessions, such as transportation or mobility issues. Home-based rehabilitation typically involves different exercise regimens and remote monitoring, allowing patients to engage in their recovery from the comfort of their own homes. These programs promote independence while ensuring that patients continue to receive the essential components of cardiac rehabilitation [19].
The growing role of remote monitoring and telehealth in post- discharge care is also a noteworthy development. Telehealth platforms enable healthcare providers to connect with heart failure patients in real-time, offering consultations, medication management, and symptom monitoring remotely. This approach not only enhances patient access to care but also allows for more proactive and timely interventions, reducing the risk of hospital readmissions [20].
In conclusion, this comprehensive review article has explored the multifaceted landscape of heart failure management, from in-hospital care to post-discharge support. Cardiac rehabilitation has emerged as a pivotal component in this continuum of care, emphasizing the importance of structured interventions to enhance patient well-being.
We began by delving into heart failure’s classifications, its goals, and its historical evolution, underscoring the enduring relevance of cardiac rehabilitation in modern healthcare. In-hospital care was examined, highlighting acute management strategies, the essential role of multidisciplinary teams, pharmacological interventions, and meticulous monitoring of cardiac function as the foundation for comprehensive care.
The components of cardiac rehabilitation were then scrutinized, emphasizing the holistic approach that encompasses exercise therapy, nutritional counseling, medication optimization, psychological support, and patient education. Intra-hospital rehabilitation emphasized the vital role of structured exercise programs, educational interventions, and strategies to promote patient adherence.
Transitioning to post-discharge care was underscored as pivotal, emphasizing the importance of personalized care plans and seamless patient information transfer. Post-discharge support offered a glimpse into the growing role of outpatient programs, home-based rehabilitation options, and the integration of remote monitoring and telehealth, highlighting the evolving landscape of heart failure management.
Throughout this journey, it became evident that cardiac rehabilitation is not just a singular intervention but rather a dynamic and patient-centered approach that adapts to the unique needs and circumstances of each individual. As we recap the critical insights gleaned, we affirm the significance of comprehensive cardiac rehabilitation in heart failure management.
A resounding call to action echoes through these pages, urging healthcare providers and policymakers to prioritize and evolve rehabilitation as an essential pillar in heart failure care. By embracing the multifaceted approach encompassed in cardiac rehabilitation and by continually seeking innovative solutions, we can collectively strive toward improved patient outcomes, reduced hospital readmissions, and an enhanced quality of life for those living with heart failure. This journey from in-hospital care to post-discharge support serves as a compass guiding us toward a brighter future in heart failure management.
Citation: Erickatulistiawan LNG, Tjahjono CT, Mayangsari V (2023) Managing Heart Failure through Rehabilitation: Insights from In-Hospital Care to Post-Discharge Support. Int J Phys Med Rehabil. 11:698.
Received: 10-Oct-2023, Manuscript No. JPMR-23-27490; Editor assigned: 12-Oct-2023, Pre QC No. JPMR-23-27490 (PQ); Reviewed: 30-Oct-2023, QC No. JPMR-23-27490; Revised: 07-Nov-2023, Manuscript No. JPMR-23-27490 (R); Published: 15-Nov-2023 , DOI: 10.35248/2329-9096.23.11.698
Copyright: © 2023 Erickatulistiawan LNG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.