Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2020)Volume 11, Issue 5
Cutaneous tuberculosis is rare, it accounts for 2% of all extrapulmonary tuberculosis and is one of the multiple
clinical presentations of extrapulmonary tuberculosis.
The lupus vulgaris is a particular clinical form and is often represented by a single lesion, the multiple forms
associated with pulmonary tuberculosis are rare.
We present a new case of multiple skin lesions of the face of a lupus vulgaris revealing pulmonary tuberculosis.
Cutaneous tuberculosis; Lupus vulgaris; Apyrexia
A 47-year-old patient presented for skin lesions, evolving for several years in a context of weight loss, asthenia and apyrexia. On examination, we had objectified, annular and maculopapulous lesions, the lesions were strictly localized on the face [1].
The scalp, the nails and the mucous membranes were without abnormality, as well as the rest of the clinical examination. The first skin biopsy was in favour of non-specific inflammatory infiltrate, a second anatomopathological examination of the forehead lesion showed an epitheliogigantocellular granuloma with caseous necrosis in favor of tuberculosis.
The radiological assessment objectified lesions that suggested pulmonary tuberculosis [2-4].
The Koch bacillus research was negative on the skin and in sputum. Dermo reaction of Tuberculin was positive. A chest scanner found a tuberculosis barracks. Skin and lung lesions have progressed favourably under tuberculosis treatment.
Lupus vulgaris is an extremely chronic, progressive form of cutaneous tuberculosis. The earliest description of lupus vulgaris was given by Erasmus Wilson in 1865 [5]. It usually occurs through contiguous extension of the disease from underlying affected tissue or hematogenous or lymphatic spread [6].
The initial lesion is a small, reddish-brown papule or nodule which later forms larger plaques by peripheral enlargement and coalescence that show evidence of healing and scarring in one area and activity in another [7]. Lupus vulgaris comes in different clinical aspects, sometimes misleading. His favourite seat is the face, especially the nose and cheeks (Figures 1, 2).
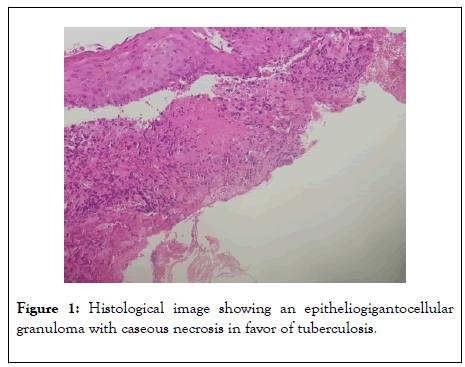
Figure 1: Histological image showing an epitheliogigantocellular granuloma with caseous necrosis in favor of tuberculosis.
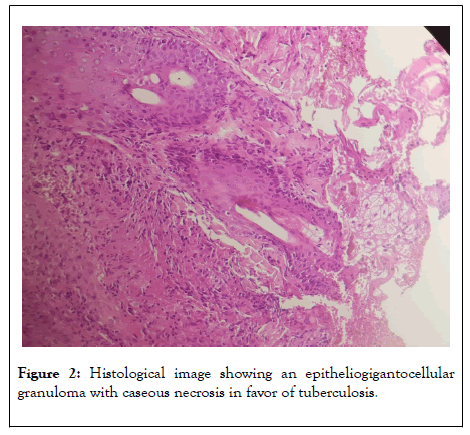
Figure 2: Histological image showing an epitheliogigantocellular granuloma with caseous necrosis in favor of tuberculosis.
More rarely, it can occur on the trunk and extremities of the limbs. It is often unique, rarely multiple [2,3]. The common variants are: plaque form, ulcerative and mutilating form, vegetative form, papular and nodular form and tumor-like (hypertrophic) form. The plaque form is the common type that presents as flat plaques with irregular or serpigenous edges, surface may be smooth or covered with psoriasiform scale. Large plaques may show irregular areas of scarring with islands of active lupus tissue, the edge may be thickened and hyperkeratotic [6].
Lupus vulgaris can be confused with leishmaniasis, leprosy, tertiary syphilis, deep fungus, sarcoidosis etc; [4]. In this particular form of skin tuberculosis, the bacillus enters the skin through the bloodstream or contiguousness [1]. Histopathology shows tuberculoid granulomas composed of lymphocytes, plasma cells, epitheloid cells and giant cells, scant or absent central caseation, in the superficial dermis. The epidermis is usually hyperplastic, but may be atrophic or ulcerated.
Tubercle bacilli are difficult to demonstrate [8]. The curative treatment of tubertic lupus is identical to the others forms of tuberculosis. He is based on immediate polychemotherapy to avoid any form of resistance. The pattern used for our patient was (6 months), includes Rifampin plus Isoniazid plus Pyrazinamide, for 2 months, then Rifampin plus Isoniazid for 4 months [4].
Our patient illustrates the difficulties and delay in the diagnostic of this form of skin tuberculosis. The multiplicity of lesions and their localization, the presence of a caseous necrosis in histology, the association with progressive pulmonary tuberculosis are, in fact, not usual in lupus tuberculosis.
No conflicts of interest
Citation: Belmourida S, Mehsas Z, Palamino H, Meziane M, Ismaili N, Benzekri L, et al (2020) Lupus Vulgaris Revealing Pulmonary Tuberculosis. J Clin Exp Dermatol Res. 11:530. DOI: 10.35248/2155-9554.20.11.530
Received: 11-Jul-2020 Accepted: 21-Jul-2020 Published: 28-Jul-2020 , DOI: 10.35248/2155-9554.20.11.530
Copyright: © 2020 Belmourida S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.