Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Paper - (2019)Volume 8, Issue 4
Background: In Ethiopia cervical cancer (CC) is a common and leading cause of death from cancer among women. CC is preventable and curable if identified in its early stage. Studies have shown that HIV positive women are at increased risk of cervical cancer. There is limited available evidence in Ethiopia on knowledge about CC and screening practices among women living with HIV.
Objective: To assess the overall knowledge about CC, screening practices and associated factors among women living with HIV in public hospitals of West Shoa zone, Ethiopia, 2016.
Methods: A cross-sectional study was conducted from April to June 2016. A simple random sampling technique was utilized to select 423 study subjects. Both bivariate and multivariate logistic regressions were used to identify associated factors.
Results: Almost half 210(49.6%) of them had good overall knowledge about CC, only 9(2.1%) of them were ever screened. Those who had heard about CC from mass media (AOR=28.2,CI:14.18-56.1), heard about CC from health workers (AOR=23.3,CI:5.69-96.1), knowing patients with CC (AOR=26.23,CI: 7.53-89.9), being older (AOR=21.2,CI:3.17-141.6), higher income (AOR=6.58,CI:2.39-18.05) and perceiving as at risk of CC (AOR=10.9, CI:4.83 24.6) were factors significantly associated with having good overall knowledge.
Conclusion: Overall knowledge of women living with HIV about CC was low and insignificant numbers of women were screened. Therefore establishing screening centers and providing health education on the importance of CC screening and risk perceptions for women living with HIV during their follow-up and through mass media are recommended.
Knowledge; Practice; Cervical cancer screening; HIV; West Shoa Zone
AIDS: Acquired Immune Deficiency Syndrome, CC: Cervical Cancer, HIV: Human Immuno-Deficiency Virus, VIA: Visual Inspection with Acetic Acid, WHO: World Health Organization
Globally, an estimated 35.3 million people were living with HIV and the number of AIDS deaths is declining in 2012 [1]. Cancer is the second leading cause of death globally which was responsible for 8.8 million deaths in 2015 and in which 70% of deaths were in low and middle-income countries [2]. Cervical cancer is the 4th most common cancer affecting women with 528 000 new cases every year and causes of cancer death in women (266 000 deaths in 2012) worldwide, 85% of these deaths occur in the developing world [2,3].
Cervical cancer is the second most frequent form of cancer (over 4,600/year) and the leading cause of cancer deaths (more than 3,300/ year) among Ethiopian women. Another estimate in 2013 indicated that every year 7,095 women are diagnosed with cervical cancer and 4732 dies from the disease. About 80% of reported cases of cancer are diagnosed at advanced stages when very little can be done to treat the disease [4-7].
HIV infection is associated with several comorbidities including opportunistic infections, and cancers that are responsible for AIDSassociated mortality [8,9]. Many studies have shown a higher prevalence of Cervical Intraepithelial Neoplasia (CIN) among HIV-positive women than among HIV-negative women [10]. Cervical cancer has a pre-invasive stage (about 10-20 years) in immune competent women, but the progression of the precancerous stage to cervical cancer is higher among women living with HIV [2,3,9,10]. The 534,000 women over age 15 living with HIV in Ethiopia are among the most vulnerable to cervical cancer [5].
The coverage of cervical cancer screening in developing countries is on average 19%, compared to 63% in developed countries, and ranges from 1% in Bangladesh to 73% in Brazil [11]. From a study done in Abuja Nigeria among HIV positive women who offered Visual Inspection with Acetic acid (VIA) screening it was positive in 6.5% women [12]. A study was done on the prevalence of precancerous cervical cancer lesions among HIV infected women in Southern Ethiopia showed that 22.1% of HIV infected women were found to be positive for precancerous cervical cancer [13].
Many studies indicated different levels of knowledge of cervical cancer and its screening practices which vary in different areas. Challenged by low funding, few trained personnel, limited tools available for prevention, early detection, and treatment. Screening methods like the Pap smear have very limited availability; shortage of trained health care providers, absence of symptoms, high cost, lack of awareness of tests, lack of injunction from their health workers, often came at an advanced stage and travel distance for necessary follow-up visits. However, a single-visit approach where a woman can be screened and then treated in the same visit has proven effective in low-resource health settings like Ethiopia [5,6,14-28].
In Ethiopia only 0.6% of all women aged 18-69 years screened every 3 years for cervical cancer, with 1.6% of urban and 0.4% of rural women aged 18-69 years were screened every 3 yrs [7]. A report of the Ethiopia road map on Cervical and Breast cancer overview showed among 1,517 women screened through VIA 152 (10.02%) of them were VIA‐Positive [29]. A study done in Addis Ababa among women living with HIV 34.2% of participants knew cervical cancer and 62.7% were willing for the test though only 24.8% were accepted the test and about 11(29.7 %) were positive for the test. The independent variables significantly associated with acceptance of screening were educational level, source of information, awareness for the test and preventability of the disease [30].
Despite cervical cancer is a major public health problem, there are no well-organized prevention, education, screening, and curative care programs in the health care system of Ethiopia. In a country where the incidence is high and late presentation of cervical cancer is predominant, there is a need for increasing the level of practice of cervical cancer screening among women living with HIV is very crucial. Few studies have been conducted about cervical cancer in Ethiopia, but data on knowledge about Cervical Cancer (CC), screening practice and associated factors among women living with HIV is lacking. Therefore there is a need to conduct this study on knowledge about CC and screening practice and associated factors among women living with HIV in the study area.
Study design and area
An institution-based cross-sectional study was conducted in West Shoa zone of the Oromia region, central Ethiopia from April 1st to June 30th, 2016. According to information from the zonal health office, there are 4 hospitals namely Ambo, Gedo, Gindeberet and Gudar Hospitals and 18 other health centers, currently providing ART services in West Shoa zone. The total number of people enrolled to ART and Pre-ART in the zone were 15,319 of which 7,798 are following at Ambo, 784 at Gindeberet, 403 at Gedo and 173 at Guder hospitals. All Women who 18 years of age and were above, who are living with HIV and who have a follow-up at public hospitals in West Shoa zone for at least 6 months prior to data collection were considered for the study. Women who have no follow up at current treatment centers were excluded.
Sample size and sampling procedure
The sample size was determined by using single population proportion formula with the assumptions of 50% proportion (P) of knowledge of cervical cancer screening among women living with HIV since there is no previous similar study, with a level of significance 5%, 95% confidence interval, a margin of error 5%. By considering a 10% non-response rate, the final sample size used was 423. After the list of all women living with HIV aged 18 years and above were prepared and entered into SPSS window version 20 by using their Pre ART registration numbers from the health management information system database. Computer generated Simple random sampling technique was utilized at each hospital to select the study subjects. The number of study respondents was allocated proportionally for all three hospitals based on their total number of patients.
Data collection tools, procedures and measurements
The questionnaires for data collection were initially prepared in English, and translated to Afan Oromo and back to English to check for its consistency by a language expert. Data were collected through an exit interview by using a pre-tested structured Afan Oromo version questionnaire. The questions included in the questionnaire were adapted from previously done related literatures and variables identified to be measured. The questionnaire consisted of socio-demographic characteristics, awareness of CC and its risk factors; and CC screening techniques and practices [17,19,21,30-33]. The training was given for data collectors and supervisors by investigators for one day.
The pre-test of the questionnaire was done on 22 women living with HIV at Guder Hospital and the necessary correction was made a week before the actual data collection. Those women who scored mean value and above for knowledge assessing questions were considered as having a good overall knowledge of CC and those women who had ever been screened for CC before were considered as practiced CC screening.
Data processing and analysis
The returned questionnaires were checked for completeness, cleaned manually, coded and entered into EPI Info 3.5.4 version and then transferred to SPSS windows version 20.0 for further analysis. Bivariate analysis was used primarily to check which variables have association with the dependent variable individually. Variables that were found to have an association with the dependent variables were entered into Multivariable logistic regression.
Ethical considerations
Ethical clearance was obtained from the Ethical review committee of Ambo University, College of Medicine and Health Sciences. Formal letter of cooperation was written to respective hospitals and verbal informed consent from each study participants was obtained after the nature of the study is fully explained in their local languages as it is attached in the questionnaire. The right to refuse was respected and information collected from this research project was kept confidential.
Socio-demographic characteristics of respondents
A total of 423 respondents were interviewed in this study making a response rate of 100%. The mean age of respondents was 34.68years with the standard deviation of +7.21(from 18 to 65 years). Almost half 199 (47%) of them were married and the majority of them 252 (59.6%) were orthodox by religion. Majority of respondents were from urban 346 (81.8%), have primary education 192 (45.4%) and 136 (32.1%) were a housewife (Table 1).
| Socio Demographic Variables | Categories | Frequencies (N=423) | Percent (%) |
|---|---|---|---|
| Age (years) | 18-29 | 103 | 24.3 |
| 30-39 | 208 | 49.2 | |
| 40-49 | 95 | 22.5 | |
| > 50 | 17 | 4 | |
| Marital Status | Single | 15 | 3.5 |
| Married/Living with partner | 199 | 47 | |
| Divorced | 69 | 16.3 | |
| Widowed | 82 | 19.4 | |
| Separated | 58 | 13.7 | |
| Religion | Orthodox | 252 | 59.6 |
| Protestant | 162 | 38.3 | |
| Others* | 9 | 2.1 | |
| Educational status | No Formal Education | 109 | 25.8 |
| Primary Education(1-8) | 192 | 45.4 | |
| Secondary education(9-12) | 95 | 22.4 | |
| Diploma and above | 27 | 6.4 | |
| Occupational status | Housewife | 136 | 32.1 |
| Government Employee | 57 | 13.5 | |
| Farmers | 44 | 10.4 | |
| Daily laborers | 73 | 17.3 | |
| Merchant | 101 | 23.9 | |
| Others** | 12 | 2.8 | |
| Place of Residence | Urban | 346 | 81.8 |
| Rural | 77 | 18.2 | |
| Family monthly income | = 300 Birr | 140 | 33.1 |
| 301- 500 Birr | 95 | 22.5 | |
| 501-1000 Birr | 119 | 28.1 | |
| > 1000 Birr | 69 | 16.3 | |
| With Mean of 788.2 ± 825.7 SD, Ranges from 70 to 6000; *Others: Muslim, wakefata, Catholic; **Others: Private jobs, no jobs, students | |||
Table 1: Socio-demographic characteristics of women living with HIV at public Hospitals in West Shoa zone, central Ethiopia, 2016.
Knowledge about cervical cancer, risk factors, and screening practices
Out of total respondents only 259(61.2%) had ever heard about CC (95%, CI: 56.3-65.7); of which 186 (44%) of them heard from radio/ television, only 28 (6.6%) from health professionals, 78 (18.4%) from friends & relatives and 7 (1.7%) heard from other sources. Two (0.5%) of the respondents had ever been diagnosed with cervical cancer, for which they got treatment. Forty-nine (11.6%) knows someone diagnosed with cervical cancer of which 19 (4.5%) were their friends, 18 (4.3%) relatives, 3 (0.7%) family members and with 9 (2.1%) have the other relationship.
Among all respondents, only 186 (44.0%) of them were able to mention one or more risk factors for cervical cancer, 64 (15.1%) of them don’t know and 9 (2.1%) mentioned as there is no risk factor (Figure 1). But only 2 (0.47%) has mentioned the human papillomavirus as a risk factor for developing CC.
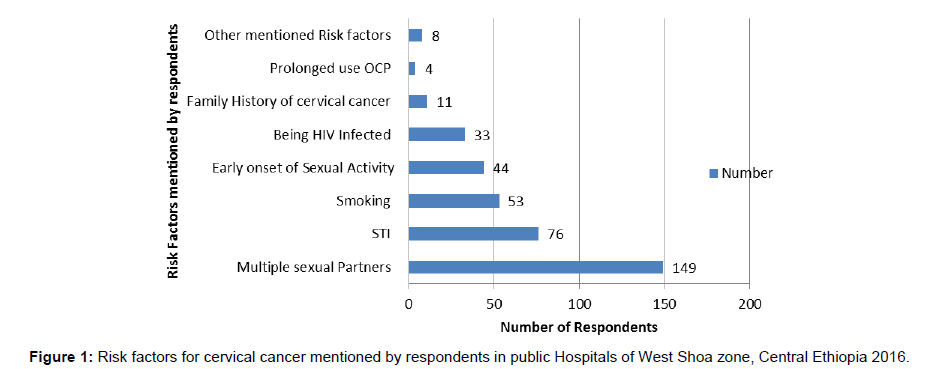
Figure 1: Risk factors for cervical cancer mentioned by respondents in public Hospitals of West Shoa zone, Central Ethiopia 2016.
Regarding early symptoms of cervical cancer, only 165 (39.0%) of respondents were able to mention at least one early symptom. From which 113 (26.7%) of them mentioned offensive vaginal discharge, 96 (22.7%) don’t know the symptoms, 59 (13.9%) excessive discharge, 44 (10.4%) abnormal bleeding between periods, 29 (6.9%) bleeding after intercourse, 23 (5.4%) post-menopausal bleeding and 11 (2.6%) mentioned other symptoms.
Almost all respondents 413 (97.6%) have at least additionally one or more risk factors for cervical cancer in addition to being HIV positive, with 50 (11.8%) have one risk factor, 115 (27.2%) two, 135 (31.9%) three, and 113 (26.7%) have four or more risk factors in the study area. The mean age at first sexual intercourse among study subjects was 17.7 years with a standard deviation of 2.9 years and 259 (61.4%) of them had more than one sexual partner (Figure 2).
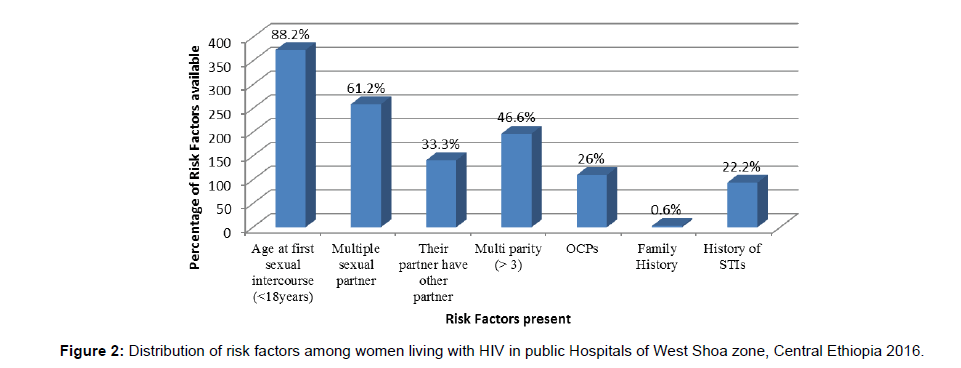
Figure 2: Distribution of risk factors among women living with HIV in public Hospitals of West Shoa zone, Central Ethiopia 2016.
When respondents were asked about risk perceptions of women living with HIV for cervical cancer; 265 (62.6%) considers themselves as at risk of cervical cancer, whereas 134 (31.7%) don’t know risk status and 24 (5.7%) considers as not at risk of cervical cancer.
Regarding respondent’s perception about how to prevent CC; 137 (32.4%) of them perceive that cervical cancer can be prevented, 62 (14.7%) don’t know and 60 (14.2%) responded as it can’t be prevented. Only 109 (25.8%) of them mentioned regular checkups and 12 (2.8%) of them mentioned through a vaccine or delaying sexual debut as prevention measures for CC. But only 74 (17.5%) of them know as screening tests were available for CC.
Almost half of the respondents 210 (49.6%) who have scored more than five (mean value) were considered as having good overall knowledge about cervical cancer (95% CI: 44.9-54.4) in the study area.
Surprisingly only 9 (2.1%) of respondents had ever been screened for CC (95% CI: 0.9% -3.5%), of which only 1(0.2%) was screened at Ambo Hospital and 8(1.9%) of them were screened at other sites. Five (1.2%) & 4 (0.9%) were seen with Pap smear and visual inspection respectively. More than half 221 (52.2%) mentioned a lack of knowledge of screening tests or didn’t ordered to do so for not being screened (Table 2).
| Variables | Number | Percent (%) |
|---|---|---|
| Had ever been screened (N=423) | ||
| Yes | 9 | 2.1 |
| No | 414 | 97.9 |
| Places Screened (N=423) | ||
| At the current Hospital | 1 | 0.2 |
| Other Sites/Hospitals | 8 | 1.9 |
| Had abnormal Result (N=423) | ||
| Yes | 3 | 0.7 |
| No | 6 | 1.4 |
| Methods used for screening (N=423) | ||
| Pap Smear | 5 | 1.2 |
| Visual inspection | 4 | 0.9 |
| Number of Pap Smear tests (N=423) | ||
| Once | 4 | 0.9 |
| Twice and more | 2 | 0.4 |
| Last time you had Pap Smear (N=423) | ||
| Within the last one year | 3 | 0.7 |
| Before one year | 3 | 0.7 |
| Reasons for not screened for CC (N=423) | ||
| Didn’t ordered to do so or Lack of knowledge on screening tests |
221 | 52.2 |
| Screening tests were not available | 63 | 14.9 |
| Not feeling at risk | 59 | 13.9 |
| Lack of symptoms | 246 | 58.2 |
| Other reasons | 17 | 4 |
Table 2: Cervical cancer screening practices among women living with HIV in Public Hospitals’ of West Shoa zone, Central Ethiopia, 2016.
Among those respondents who were not screened for CC, almost all 392 (92.7%) of them are willing to be screened for CC in the future.
Factors associated with knowledge of cervical cancer
Multivariate analysis, revealed that respondents Age, average monthly income, who have heard about CC from Mass media and health workers, knowing patients with CC and perceive HIV positive women as at risk of CC were significantly associated with having good overall knowledge about CC. But on multivariate analysis there is no variable that was found significantly associated with CC screening practice.
This study identified that those women whose age were 50 or more were 21 times more likely to have good knowledge than those who were young (AOR=21.2, CI: 3.17-141.6) and those whose average monthly income was greater than 1000 Ethiopian Birr were 6.58 times more likely to have good knowledge than those with the lowest quartile (AOR=6.58, CI: 2.39-18.05).
In current study women who have heard about CC from Mass media were 28 times more likely to have good knowledge about CC than those who didn’t (AOR=28.2, CI: 14.18-56.1) and those who have heard about CC from health workers were 23 times more likely to have good knowledge than those who didn’t (AOR=23.39, CI: 5.69-96.1).
This study also revealed that a woman who knows patients with CC were 26 times more likely to have good knowledge about CC than those who didn’t (AOR=26.23, CI: 7.53-89.9) and those who perceives women living with HIV as at risk of CC were almost 11 times more likely to have good overall knowledge about CC than those who didn’t knows the risk status (AOR=10.9, CI: 4.83-24.6) (Table 3).
| Independent Variables | Good Knowledge about CC | Crude OR(95%CI) | Adjusted OR(95%CI) | P-Value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age of respondents in years | |||||
| 18-29 | 44 | 59 | 1 | 1 | 0.015 |
| 30-39 | 101 | 107 | 1.26(0.78-2.03) | 1.40(0.65-2.99) | 0.38 |
| 40-49 | 53 | 42 | 1.69(0.96-2.97) | 1.90(0.75-4.8) | 0.17 |
| > 50 | 12 | 5 | 3.21(1.05-9.80) | 21.2(3.17-141.6) | 0.002* |
| Average monthly income | |||||
| = 300 Birr | 52 | 88 | 1 | 1 | 0.003 |
| 301- 500 Birr | 43 | 52 | 1.39(0.82-2.37) | 1.29(0.53-3.13) | 0.56 |
| 501-1000 Birr | 66 | 53 | 2.10(1.28-3.46) | 1.45(0.64-3.27) | 0.36 |
| > 1000 Birr | 49 | 20 | 4.14(2.22-7.73) | 6.58(2.39-18.05) | 0.000* |
| Heard about CC from health workers | |||||
| Yes | 25 | 3 | 9.45(2.81-31.84) | 23.39(5.69-96.1) | 0.000* |
| No | 185 | 210 | 1 | 1 | |
| Heard about CC from Mass Media | |||||
| Yes | 157 | 29 | 18.79(11.39-30.9) | 28.2(14.18-56.1) | 0.000* |
| No | 53 | 184 | 1 | 1 | |
| Knows women diagnosed with CC | |||||
| Yes | 44 | 5 | 11.02(4.27-28.43) | 26.0(7.53-89.9) | 0.000* |
| No | 166 | 208 | 1 | 1 | |
| Perceives HIV +ve women as at risk of CC | |||||
| Yes | 181 | 84 | 13.88(7.93-24.30) | 10.9(4.83-24.6) | 0.000* |
| No | 11 | 13 | 5.45(2.12-14.01) | 4.0(1.00-16.0) | 0.05* |
| I don’t know | 18 | 116 | 1 | 1 | 0.000* |
| *Were those found to be significantly associated (p-value<0.05) | |||||
Table 3: Multiple logistic regressions results of factors associated with overall knowledge about CC among women living with HIV in public Hospitals of West Shoa zone, Central Ethiopia, 2016.
On the bivariate analysis age of respondents, those who heard about CC from health professionals, and knowing risk factors for CC were associated with practice of cervical cancer screening. But on multivariate analysis there, was no variable that was found significantly associated with CC screening practice.
This study revealed that almost half of respondents 49.6% were having good overall knowledge about CC (95% CI: 44.9-54.4). Which is almost in line with the study done in Lao PDR 54.4% of women at HIV treatment centers, Congo Kinshasa 43% of the women obtained a sufficient score on knowledge and in eastern Uganda, 55.4% of women had high knowledge about cervical cancer and its risk factors [19,21,34]. But it is higher than the study done in Gondar town 31.0% of them were found to have comprehensive knowledge about cervical cancer, Bhutan 30.1% of university graduates have found to possess above average knowledge and Kilimanjaro Tanzania 19.2% of women reported to have a high level of knowledge [17,25,35]. This might be due to the difference in study setting in which those women living with HIV who are on follow-up were more likely to get information’s and health educations, perceive the severity and have more knowledge than others which is also supported by a study done in Lao PDR [21].
Only 2.1% of respondents had ever been screened for cervical cancer (95% CI: 0.9% -3.5%), 1.2% & 0.9% were seen with Pap smear and visual inspection respectively and more than half 52.2% mentioned lack of knowledge of screening test or didn’t ordered to do so. In agreement with this survey done in Ethiopia only 0.6% (1.6% of urban & 0.4% of rural) of all women aged 18-69 years screened every 3 years for cervical cancer, a study done in rural Northeast Nigeria 2.3% had Pap smear test and Uganda 4.8% had been ever screened [7,18]. But lower than studies done in Addis Ababa among HIV positive women 11.5%, Congo Kinshasa 8.6%, Masaka Uganda 7%, Burkina Faso 11.07% and Kisumu Kenya 17.5% of respondents underwent at least one cervical screening in their lifetime [19,20,24,28,30]. These differences might be due to the difference in the study area, population and setting in which there were no available screening services in the current study areas women tend to go to the capital Addis Ababa for CC screening.
This study identified that those women who were older than 50 years were 21 times more likely to have good knowledge than those who were younger than 29 years. Those whose average monthly income was greater than 1000 Ethiopian Birr were 6.58 times more likely to have good knowledge than those with less than or equal to 300 Ethiopian Birr. This is may be due to those women who are more than 50years were more likely to have different symptoms which lead them to seek health care during their follow-up at chronic care clinic and those with higher monthly income might have access to different sources of information which enhances their knowledge about CC.
In current the study, those women who have heard about CC from Mass media and health workers were 28 and 23 times more likely to have good knowledge about CC than those who didn’t respectively. Those women who know the patient with CC were 26 times more likely to have good overall knowledge than those who didn’t. Similarly, a study done in Gondar indicated knowing someone with cervical cancer is more likely they are knowledgeable (AOR=4.91) [17]. This indicates that providing information and education about cervical cancer and its screening practices plays a vital role in the prevention of cervical cancer and its early detection, which is also supported by a study done in Gondar and Lao PDR [17,21].
Those women who perceive women living with HIV as at risk of CC were almost 11 times more likely to have good overall knowledge than those who didn’t know the risk status which is in line with the study done in Lao PDR among women living with HIV [21]. This is may be due to those who know early symptoms or risk factors were more likely to perceive the risk status and have good knowledge about it.
From this study, the overall knowledge of women living with HIV about CC was low compared with their susceptibility to the problem and the available risk factors among study subjects. Very low or insignificant numbers of women were screened for CC. But, almost all of the respondents are willing to undergo the screening test if available. Having heard about cervical cancer from mass media and health workers, being older, having higher average monthly income, knowing patients with cervical cancer and considering women living with HIV as at risk of cervical cancer were factors associated with having a good overall knowledge of CC screening. Based on the findings of this study; Federal Ministry of Health, Regional Health Bureau together with hospitals, health professionals & other stakeholders would be better establish screening centers, integrate the service with HIV Chronic care, supporting and providing health education on the importance of CC screening and risk perception for women living with HIV during their follow up by health care providers and through mass Medias to enhance their knowledge thereby to promote and ensure compliance with CC screening practices. Further large scale studies would be better conducted on the general population and those who are at high risk of cervical cancer.
Conflict of interest disclosed was none.
This research was fully funded by Ambo University, Office of Research and community services Vice president.
GAB, conceptualized the study, designed the study instrument and conducted the data analysis and wrote the first draft and final draft of the manuscript as principal investigator. DBD and KBD participated in the design, data analysis, revised subsequent drafts of the paper and involved in critical review of the manuscript. All authors read and approved the final manuscript.
We are grateful to Ambo University, College of Medicine and Health Sciences for approval of the study and providing us with financial support. We would like to extend our gratitude for the Hospitals and West Shoa zone health office for giving us the necessary information and support during the development of a proposal and data collection period and women who participated in this study
Citation: Bulto GA, Demmissie DB, Daka KB (2019) Knowledge about Cervical Cancer, Screening Practices and associated factors among Women Living with HIV in Public Hospitals of West Shoa Zone, Central Ethiopia. J Women’s Health Care 8:467. doi: 10.35248/2167-0420.19.8.467
Received: 01-Nov-2018 Accepted: 25-Jun-2019 Published: 30-Jun-2019
Copyright: © 2019 Bulto GA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.