Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2023)Volume 14, Issue 2
Purpose: This study aimed to establish criteria associated with the application of Poly-L-Lactic Acid (PLLA) (ER) in the facial region as a collagen biostimulator. The inverted-F technique was used, consisting of a marking performed for safer and more standardized results.
Methods: Data were collected from 3 female patients. All were submitted to treatment with Poly-L-Lactic Acid (PLLA) (ER-Rennova Elleva®-Ghana R&D CO, LTD-South Korea), using the inverted-F technique, according to the individual needs of each patient. Photographic records were taken on the day of application and 60 days after. All data are expressed as mean ± Standard Error of Mean (SEM). All descriptive statistics were performed using the GraphPad Prism 9.0® software platform (United States).
Results: The data analysis demonstrated that the patients showed an increase in face lifting, greater volumization, and improved vascularity. It is suggested that further studies with a larger sample size be carried out, in order to provide further statistical clarification.
Conclusion: The increase in demand for facial rejuvenation has increased in popularity in recent years. This comprises a non-permanent injectable procedure that is able to restore and improve curves and contours.
Although statistical relevance has not been observed, the inverted-F technique optimizes the use of powerful biostimulators, particularly in patients who look for an accurate aesthetic result, with improved facial curves, lifting in the temporal and zygomatic region, and preserving areas of hyperdynamic muscle movement, as it is a safe and replicable technique.
Collagen; Aging; Antiaging; Rejuvenation; Facelift; Self-esteem; Beauty
The concepts of beauty have been present in society since primordial times, irrespective of gender, social standard, and cultural level of individuals. In modern times, the search for a young and healthy skin is increasing, which is routinely demonstrated by the number of individuals looking for alternatives to improve the texture of the skin, as well as a smooth and youthful appearance [1].
Currently, a number of options for products and/or procedures are commercially available, aimed at providing treatments and maintenance for the skin. Consequently, consumers have easy access to these treatments, including procedures performed in aesthetic clinics, peels, facial creams, and oral supplements, among others. Moreover, the search for products that stimulate collagen production has been common [2].
Collagen is one of the most abundant proteins in the human body. Among its various functions is its high relevance in the support and stability of human tissues [3]. Collagen synthesis is carried out by cells called fibroblasts. Over the course of an individual’s life, collagen reserves may undergo changes and suffer damage, resulting in changes in the architecture, firmness and organization of collagen fibers. This can lead to several changes in the skin, including wrinkles, aging, sagging, etc. [4,5].
With the aging process, there is a reduction in the synthesis and total amount of collagen, by about 1.5% per year, which begins around 25 years to 30 years of age. The neoformation and deposition of these fibers play a key role in the healing process, as the modulation of cell migration and proliferation ensures the effectiveness of tissue repair [6].
Biostimulation through injectable Poly-L-Lactic Acid (PLLA) can be considered a good alternative for collagen replacement, given that it is a safe, biocompatible and biodegradable component [7]. PLLA is able to enhance collagen production by stimulating physiological inflammation in the host. In patients who have collagen loss, replacement through injectable procedures may comprise a solution in the search for natural beauty [8]. The PLLA-based collagen biostimulator (ER-Rennova Elleva®-Ghana R&D CO, LTD-South Korea) currently stands out in the market, thanks to its production and lyophilization of spheres through the B3Homos+® technology.
In order to optimize the facelift process using places where aging declines are greater, such as the lateral, middle and medial malar compartments, an area of application of collagen biostimulators was designed to cover this entire area, reducing frequent adverse effects in the orbicularis oculi, rounding of faces (due to the indiscriminate placement of biostimulators), and worsening of the region of the cutaneous mandibular fat compartment-a phenomenon known as jowls.
This study aimed to establish criteria associated with the application of Poly-L-Lactic Acid (PLLA) (RE) in the facial region, as well as a description of the inverted-F technique, in a safe and standardized way.
Anatomy of the face: Superficial fat compartments
The superficial fat of the face, located in the subcutaneous area or hypodermis, is divided by the extent of the deeper retaining ligaments that attach to the skin. These ligaments form fibrous septa between the compartments where the vascular ramifications are located, instead of being diffused in the Submuscular Musculoaponeurotic System (SMAS) [9,10]. In the buccal third of the face, the occurrence of many vascular ramifications indicates an anatomical transition from one superficial fat compartment to another. The main superficial compartments include the lateral, medium, superficial malar, nasolabial and jowl (cutaneous mandibular) compartments, with the most relevant for this study being the lateral, medium and superficial malar compartments (Figure 1) [9-11].
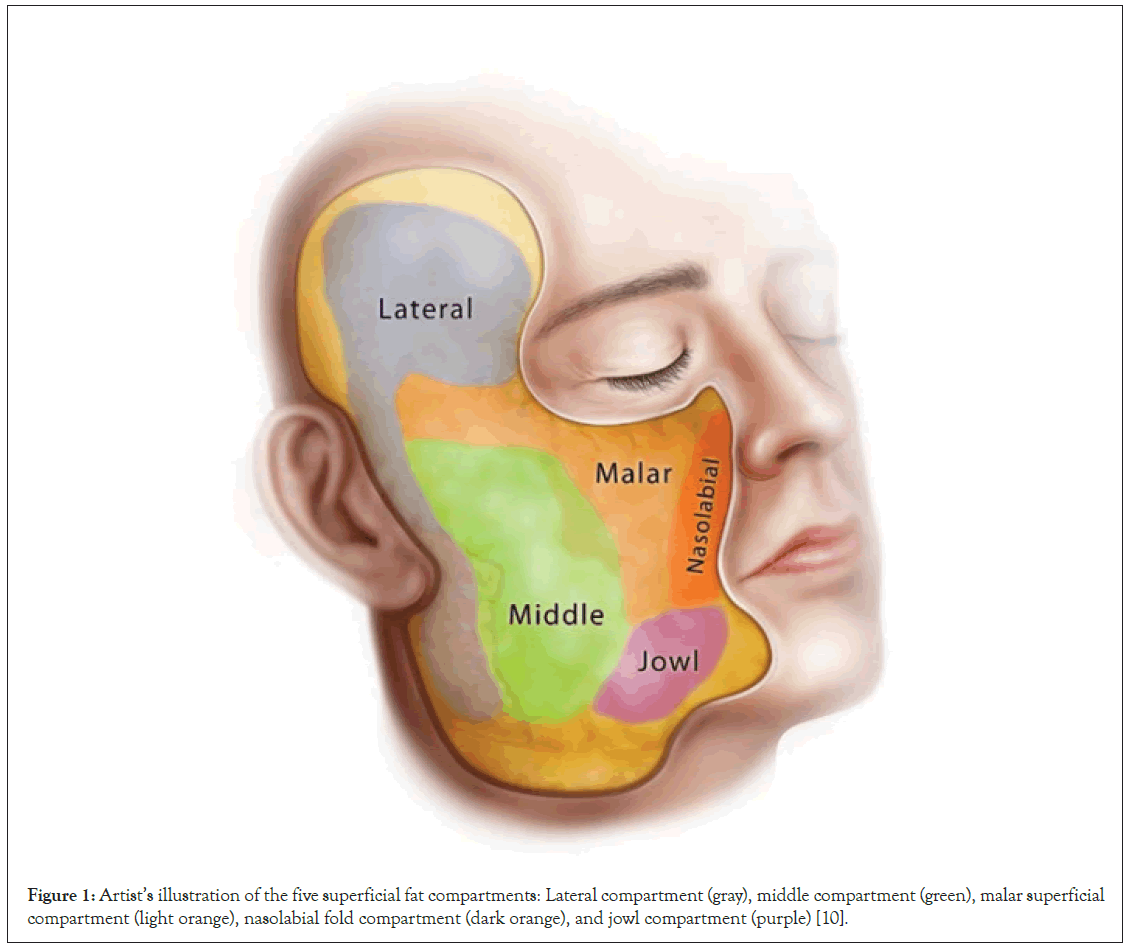
Figure 1: Artist’s illustration of the five superficial fat compartments: Lateral compartment (gray), middle compartment (green), malar superficial compartment (light orange), nasolabial fold compartment (dark orange), and jowl compartment (purple) [10].
Ethical considerations and study design
The procedures were carried out according to the established protocol, following the ethical standard proposed by the Declaration of Helsinki [12] of the World Medical Association. All participants agreed with the Free, Prior and Informed Consent (FPIC) Form, as well as the publication of their cases in scientific journals.
The following inclusion criteria were considered: Patients aged over 18 years; women; and patients with indication of treatment for sagging, improvement of the contour and quality of the skin. Exclusion criteria were: Age under 18 years; autoimmune diseases, bleeding disorders; gestation; people with inflammation or infection near or in the region of treatment; and patients with hypersensitivity to any component of the product.
ER reconstitution
ER [13], is supplied in a sterile, lyophilized form for injection in an amber glass vial. Each product kit consists of 1 vial per box. Each bottle has 520 mg in content, consisting of 210 mg of Poly- L-lactic Acid (PLLA), 132 mg of carboxymethylcellulose, and 178 mg of mannitol.
According to the recommendations for good clinical practice, for better use of the product, reconstitution can be manual or automated. Manually, the following procedure was performed: Adding 12 ml of water for injection to the RE vial; stirring for 1 minute; waiting for 10 minutes; shaking again for another 1 minute; waiting 10 minutes; and repeating these 6 cycles until completing 1 hour, forming the standard suspension.
At the end of the reconstitution process, 1.5 ml of the standard suspension and 0.5 ml of 2% lidocaine (without vasoconstrictor) were aspirated into a 3 ml syringe, totaling 2 ml. The total content of the reconstitution added to the anesthetic was enough to load the 3 ml syringe 8 times, containing 2 ml in each aspiration, totaling 16 ml of final reconstitution. The final concentration of the suspension (water+lidocaine) was 13.12 mg/ml.
Determination of application points
To determine the application points, the superficial fat compartments of the face were considered. The ones used in this study were the lateral malar fat compartment, medium malar fat compartment, and superficial malar fat compartment.
The lateral malar fat compartment is located in the preauricular region and appears as dense, fibrous and vascular adipose tissue. This compartment is located directly over the parotid gland and extends caudally along the lateral edge of the platysma (Figure 2A) [11]. The middle malar fat compartment is located medial to the parotid, between the lateral compartment and the anterior border of the masseter. In facelift surgeries, it is the compartment of choice for subcutaneous dissections of the middle third, as it is a relatively large, thick and avascular area (Figure 2B) [9,11,14]. The superficial malar fat compartment is located along the zygoma and extends anteriorly towards the paranasal region, providing volume to the anterior cheek (Figure 2C) [9,11,14].
Figure 2: Dissection of cadavers. (A) Lateral and nasolabial fat compartment highlighted. (B) Middle facial fat compartment, with the red arrow representing an attachment zone along the lateral zygoma, where the middle compartment meets the superficial malar fat compartment. (C) Superficial malar fat compartment, with the red arrow representing the attachment zone between the middle and malar compartment. [10].
Inverted-F technique
Through the evaluation of the facial anatomy and its fat compartments, the standardization of the inverted-F demarcation was determined. For execution of the marking, a distance of 2.0 cm anterior to the tragus was maintained, due to the location of the ascending branch of the facial artery, covering the sideburn line, ascending to the temporal region, and descending to the angle of the mandible and in a straight and continuous line in relation to the jaw angle.
The marking continues in the temporal area covering this muscle and, bordering the orbicularis oculi muscle (1.5 cm to 2.0 cm from the orbital bone margin), meeting the nasojugal groove. It descends along the nasojugal groove and continues obliquely to the lower border of the lateral part of the zygomatic bone, descending and leaving out the region of shadow caused by the prominence of the facial blush, forming the top model look, and descending to find the angle marking of jaw.
The marking of the buccal third is carried out on the edge of the mandible and protuberance of the zygomatic bone (cheekbone), which does not include the jowl area, as this would cause an increase in dermal thickness, subsequently, favoring ptosis in this region (Figure 3).
Figure 3: Five images detailing the marking of the Inverted F.
In the lower third, the marking of the base of the mandible is delimited, from the angle of the mandible to the anterior part of the masseter muscle, i.e., before the mandibular fat compartment (jowls) (Figure 4).
Figure 4: Exemplification of the “inverted F” demarcation. The white color represents the ports; black lines represent the injection direction of the biostimulator (retrograde injection); the orange color represents the demarcation.
Study participants
The inverted-F technique was tested in 3 patients. Patient 1 was a female patient, aged 56 years, who sought clinical care due to complaints related to facial flaccidity. Moreover, the patient had moderate folds in the nasolabial fold, severe marking in the periorbital fold, marionette lines, and bone loss, triggering a lack of facial contour. The patient had no history of previous procedures (Figure 5A).
Patient 2 was a 45-year-old female patient. The patient presented complaints related to the improvement of flaccidity and facial rejuvenation. The patient’s physical assessment showed that she had lost her facial contours, presenting flaccidity due to her age group and slight markings in the periorbital and nasolabial folds. The patient had a history of previously performed procedures, namely: Botulinum toxin and hyaluronic acid-based facial fillers (Figure 5B).
Patient 3 was a 58-year-old female patient. As a result of her age, she showed signs of collagen loss, which made it possible to observe facial flaccidity, the presence of very light marionette lines, and light markings in the nasolabial fold area. The patient had a history of a previous cosmetic procedure, also involving botulinum toxin (Figure 5C).
Figure 5: Photographic records of the patients before the inverted-F technique procedure. (A) Patient 1; (B) Patient 2; (C) Patient 3. Records made using the QuantifiCare software.
Recording of results
The follow-up of the results was performed using QuantifiCare: 3D aesthetic photography systems. The following assessments were performed: Records before and after 60 days of the procedure; lifting effect, volumization; and facial vascularization.
Statistical analysis
The facial lifting and volumization level of each region was compared through one-way ANOVA followed by Tukey’s post-hoc test. All data were expressed as the mean ± Standard Error of the Mean (SEM). Statistical analysis was performed using GraphPad Prism 9.0® software (United States).
Samples were collected from 3 female patients aged between 45 years and 58 years. All patients had aesthetic complaints mainly related to skin flaccidity and were treated with PLLA (ER) using the inverted-F technique. Considering that the technique seeks biostimulation, without the consequence of a “rounded” appearance of the face, some criteria were evaluated, including the facelift effect.
It was observed that there was a facelift effect across the regions where the PLLA application was performed in the 3 patients evaluated (Figures 6A and 6C). Furthermore, mainly in patient 2, lifting was demonstrated in the regions where the inverted-F technique was performed, demonstrating a satisfactory result (Figure 6B). There was a lifting effect of 8.63 mm on the malar of patient 1, 9.06 mm on patient 2, and 14.68 mm on the malar of patient 3.
Figure 6: Before and after the facelift procedure in the patients, the right side being before and the right side being 60 days after the first application. (A) Patient 1; (B) Patient 2; (C) Patient 3.
Face lifting was evaluated in the study participants. The assessments were performed in the following regions: Lateral, malar, nasolabial, and jowls. Statistical relevance was observed in 4/5 regions analyzed (malar, nasolabial, and jowl) (p<0.05) (Figure 7).
Figure 7: Mean facelift effect in different facial regions according to the QuantifiCare software, after 60 days of collagen stimulation. Data were expressed as mean ± SEM and analyzed by one-way ANOVA followed by Tukey’s post-hoc test, p<0.05. Note: *: p<0.05 vs. lateral region.
The evaluation of facial regions with facial volumization showed that there was no statistical significance when comparing volumization in facial regions and the inverted-F technique (Figure 7).
The analysis of the vascularization before the application of PLLA and after 60 days showed that there was an increase in facial vascularization after the application. It is possible to observe that such an increase in vascularization occurred mainly in the areas where biostimulation with ER occurred (Figure 8).
Figure 8: Before and after facial volumization in patients, with the right side being before and the left side being 60 days after the first application.
Facial aging is an inexorable multicentric process related to age, which causes a number of physiological and morphological changes in facial structures, its relevant causes being the loss of volume and sagging of soft tissues [15]. The process of facial aging is characterized by the loosening of the ligaments that support the face, flaccidity involving the tissues, a skin that is less able to support muscle forces, and reabsorption of supporting bone structures, generating the appearance of wrinkles and static marks, which vary according to the individual characteristics and lifestyle of each individual [16,17].
Retaining ligaments comprise support structures formed by fibrous septa that separate fat compartments, and changes in the bone structure, fat tissue and ligaments result in loss of volume and tissue flaccidity in the face, characterizing the aging process. Another key component is the loss of support in muscle stability and interaction-a young facial structure provides convexity to the muscle fibers, which allows a powerful contraction of the levator muscles. In the aging process, the underlying muscle support is lost, with subsequent ptosis of the facial structure [11].
Changes in the dermal connective tissue essentially correspond to a reduction in the extracellular matrix, which are the major causes of wrinkling and sagging of the skin, as they determine profound changes in its mechanical properties, leading to the appearance of wrinkles. A number of studies have shown that aging processes affect the enzymatic activities that determine the synthesis, remodeling, and process of loss of dermal extracellular matrix components (collagen, elastin, and glycosaminoglycans). Thus, aging processes promote a reduction in the extracellular matrix density, as well as its quality [18].
Individuals wish to age with quality, without exaggeration, in a gradual and natural manner. Collagen biostimulators comprise procedures that promote a subclinical and physiological inflammatory process, which recognize, after neutrophils, microparticles injected into the subcutaneous tissue or deep dermis of patients. These cells are then converted into macrophages, which, in order to protect the body, encapsulates all microspheres. In this process, fibroblasts-cells known for making up human endogenous and natural collagen-approaches these microspheres and gradually use them to form a firmer, more organized, elastic and structured collagen network [19]. This process normally takes 1 month to 3 months, and has a duration of at least 1 year, bringing firmness to the face.
Collagen biostimulators are a great option in the treatment for facial rejuvenation, given their ability to stimulate the formation of new collagen through a local inflammatory process. This mechanism of action was investigated by who confirmed this human tissue response [20,21].
There was statistical evidence of the relevance between the facelift process and the application of PLLA (ER), and it is noteworthy that there was an increase in the patients’ facelift effect. Such observations are extremely relevant, as the facelift has a strong influence on rejuvenation, as well as increase and elevation of soft tissues, among other effects [22,23]. Considering the evidence of the association between increased facelift and application of PLLA on the face through the inverted-F technique, further studies are suggested, with a larger sample of patients.
There was no statistical association between volumization. Such results are extremely relevant, as the volumization caused by the application of PLLA (ER) may consequently lead patients to the sensation of a rounded face, and it is the goal of the inverted-F technique to avoid this occurrence. Such characteristics provide several advantages, including a personalized protocol according to the patient’s individual needs [17,24].
An increase in facial vascularity was observed before and days after PLLA treatment (ER). This increase was still perceptible in the jowl region of patient 3. It is speculated that the increase in vascularization subsequently leads to the stimulation of collagen production. Moreover, several other benefits are observed, including intensified blood flow in the region, delivering more growth factors, and increase in cell proliferation, among others [23].
This treatment, which was initially aesthetic in nature, has now become an essential component in the pursuit of happiness, restoring self-esteem by meeting the expectations of a large number of patients, always prioritizing associations of beauty and function, which are facilitated by experienced and qualified professionals [25-27].
Several treatment options are available for collagen biostimulation, with varied benefits. This paper demonstrates that the Inverted-F technique is a new, effective, simple, safe and easily reproducible procedure to provide an accentuated facelift, reduced nodules and anatomical intercurrences, and a reduction of facial roundness, providing satisfactory results. Recent clinical evidence demonstrates that the use of this procedure has a huge impact on facial contouring, communication, and individuals’ confidence.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Bastos B, Nascimento C, Pretel H, Pretto D (2023) Inverted-F Technique: Safety and Optimization Protocol for Collagen Biostimulators. J Clin Exp Dermatol Res.14:633.
Received: 29-Mar-2023, Manuscript No. JCEDR-23-22637; Editor assigned: 31-Mar-2023, Pre QC No. JCEDR-23-22637 (PQ); Reviewed: 14-Apr-2023, QC No. JCEDR-23-22637; Revised: 21-Apr-2023, Manuscript No. JCEDR-23-22637 (R); Published: 28-Apr-2023 , DOI: 10.35841/2155- 9554.23.14.633
Copyright: © 2023 Bastos B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.