Reproductive System & Sexual Disorders: Current Research
Open Access
ISSN: 2161-038X
ISSN: 2161-038X
Research Article - (2022)Volume 11, Issue 5
Background: Maternity Waiting Homes (MWHs) are residential facilities located near a health facility to accommodate women in their final weeks of pregnancy to bridge the geographic gap in obstetric care between rural and urban areas and areas with poor access to a facility. The world health organization adopted it as one component of a comprehensive package to prevent maternal morbidity and mortality. Yet, there is a shortage of information on the magnitude of intention and utilization of MWH among pregnant women in the study area. The purpose of the study was to assess intention to use MWH and associated factors among pregnant women.
Methods: Community based cross-sectional study was conducted from February 20-March15, 2019 and structured questionnaire was used to collect data by face to face interview from 556 pregnant women. The data were entered into EPI data version 3.1 and binary logistic regression analysis was performed using SPSS version 20 to determine significant factors related to intention to use MWH. Adjusted Odds Ratio (AOR) was used to assess the strength of association between independent and dependent variables.
Results: A total of 556 pregnant women were participating in the study with a 99% response rate and 44.6% pregnant women were intended to use MWH with 95% CI(41%, 48%). After adjusting for possible confounders, educational status ((AOR)=4(95% CI: 2.1,8.2)), ANC visits (AOR=3.7(95% CI: 2,7.2)), experience of MWH (AOR=2.6(95% CI:1.6, 4.3)), direct attitude (AOR=2.3(95% CI:1.5, 3.5)) and direct perceived behavioral control (AOR =3.3(95% CI:2.1, 4.9)) were significant predictors of intention to use MWH.
Conclusion: Educational status, ANC visit, the experience of MWH, direct attitude and direct perceived behavioral control were predictors of intention to use MWH. To scale up the mothers intention about utilization of MWH and to overcome the challenges, the district and community should focus on health education and raising awareness about the usefulness of MWH, promoting ANC visit, promoting family and community support, and mitigating logistical barriers.
Maternity waiting home; Intention to use; Pregnant women; Antenatal care
AOR: Adjusted Odd Ratio; ANC: Antenatal Care; APH: Ante Partum Hemorrhage; EOC: Emergency Obstetric Care; FMoHE: Federal Ministry of Health in Ethiopia; IUFD: Intrauterine Fetal Death; HDAL: Health Developmental Army Leaders; MCH: Maternal and Child Health; MMR: Maternal Mortality Ratio; MWH: Maternity Waiting Home; MDG: Millennium Development Goals; MBDHO: Misrak Badewacho District Health Office; PNC :Post-Natal Care; SDG: Sustainable Development Goals; TPB: Theory of Planned Behavior; UNICF: United Nation International Child Fund; WHO: World Health Organization
As a World Health Organization estimate shows, globally there were 303,000 maternal deaths occurred in 2015. Thus, in developing countries, maternal mortality ratio (MMR) was 230 per 100, 000 live births, whereas in developed countries MMR was only 16 per 100,000 live births [1]. Only two regions of WHO contributed about 86% of maternal death, namely sub-Saharan (62%) and southern Asia (24%). In country level, two developing countries accounted one-third of maternal mortality: India and Nigeria accounted for 50000 (17%) and 40000 (14%) maternal deaths respectively [2].
Overall, maternal deaths are due to three delays; delay in decision making to get maternal health service, delay on getting access towards health facilities and delay in receiving maternal health services after reaching facilities [3-5].
WHO adopted Maternity Waiting Home (MWH) to reduce maternal and neonatal morbidity and mortality specially to prevent second delay. Also, it is aimed to improve access to skilled birth attendance and emergency obstetric care which ultimately results in reduction of maternal and prenatal mortality, particularly for women in rural and remote areas. Also MWH increases access to ANC visits, postnatal care and health information about family planning and child vaccination by a health professional [6-10].
MWHs are residential facilities located near a health facility to accommodate women in their final weeks of pregnancy to bridge the geographic gap in obstetric care between rural and urban areas and areas with poor access to a facility [6,11,12]. Globally MWH was started at the beginning of the 20th century in Europe and Northern America to facilitate waiting home for pregnant mothers in remote geographic area voluntarily [13].
In Africa, after the introduction of MWH maternal and still birth dramatically decreased and health facility deliveries were improved. In Nigeria maternal death in health facility was decreased by 90% and still birth by 85%. In Uganda MWH helped to lower maternal mortality by 50% and in Cuba MWH increased institutional deliveries by 36% [10]. After initiation of MWH in Eritrea health facility delivery was increased by 49%. In Zimbabwe, Tanzania, Ghana, Sothern Malawi and Zambia ANC, skilled birth attendant and health facility deliveries were increased and maternal and neonatal deaths and home delivery were decreased after the introduction of MWH [6,10,14-16].
In Ethiopia, at Attat Hospital after the introduction of MWH in 1985 there was remarkable improvement of maternal health. The maternal mortality was 89.9 per 100,000 live births among MWH users when compared with non-users (1333.1 per 100,000 live births) as well still birth rate for women using MWH was 17.6 per 1000 live births and 191 per 1000 live births not-using MWH [17,18].
Reaching global target of less than 70 maternal mortality per 100, 0000 live births in 2030 requires the annual maternal death reduction of 7.5%, that means almost it requires more than the double rate of achievement between 2000 and 2015 [19]. However in sub-Saharan Africa only half live births were assisted by skilled health professional and still reduction of maternal mortality is low to achieve the targeted maternal mortality reduction for 2030. Early initiation of antenatal care follow-up, skilled care during labor and delivery and postnatal care will prevent most catastrophic maternal and child death [19-21].
There are improvements in maternal health service in Africa after introduction of MWHs. However; still the maternal health services such as ANC, institution delivery and PNC were low. In rural district of Ghana only one out of 25 women were stayed one night at MWH in the first year. The studies showed that in Kenya only 10% of mother’s who gave birth at hospital were used MWH and in Zimbabwe only 33% were used it [22]. The qualitative study in Zambia showed that only 6(27.3%) out of 22 respondents were utilized MWH and almost two third of mother’s didn’t used MWH [6,10,14].
Many studies showed the willingness of pregnant women to stay MWH when they were asked. But some difficulty was hindered them from using MWH in Africa. The study from Kenya reported that the lower rate of MWH users were due to lack of women’s decision to use it and 95% mothers want husband permission to use MWH [22]. This holds true for other countries, the studies from Zambia, Ghana, Nigeria, Malawi, Zimbabwe and Eritrea pointed out that lack of food, social support, family permission, negative attitude towards nurses, high direct and indirect cost of MWH, cultural barriers and inexpensiveness of home delivery were the top problem toward MWH usage among pregnant women [6,10,23,24].
According to 2016 EDHS, only 26% of pregnant women gave birth to their last pregnancy at health facilities and MMR were 412 deaths per 100,000 live births [25]. To improve maternal health the government of Ethiopia adopted different strategies such as giving free maternal health services, extended community health worker program in urban and rural community to reach target for 2020 [21,26]. In addition to this the government also designed MWH to scale up health facility deliveries, to reduce maternal and infant deaths for those pregnant women from remote areas to overcome geographic barriers that prevent pregnant women from getting Emergency Obstetric Care (EOC). But still the progress is low to achieve stated target accordingly [11,26-28].
The national conducted survey in Ethiopia showed that only 17% of mothers were intended to use MWH [27]. The study from eastern Gurage and Jimma district showed that still intention to use MWH is low among pregnant women. The most frequently mentioned reasons for their non-using of MWH were inaccessible of transportation, direct and indirect MWH cost, lack of family support, lack of knowledge, high dependency on family or husband for decision and cultural beliefs [11,29]. Also, another study from Attat hospital in Ethiopia indicated that despite increment of health facility delivery, only 5% of delivery was reported after introduction of MWH. Various levels of fee were needed for staying at MWH; for example, at Attat, Wolisso and Arbminch hospitals, MWH stay fee were 50, 40 and 20 Ethiopian Birr respectively for onetime [18,30].
In 2014, the Federal Ministry of Health Ethiopia (FMoH) designed a policy and strategy which promotes the implementation of MWHs [31]. Almost all (99%) health institutions with MWHs or rooms received some support either from the community, faith-based organizations, NGOs, the health institution itself, or a combination of those sources. The most common source of support was from the community 82%, followed by NGOs 63%. Still low utilization of MWH resulted from socioeconomic, demographic, facility related and culture and custom related constraints in Ethiopia [12].
In southern Ethiopia, about 57% of health facilities have MWHs however, only 2% of mothers were intended to use MWH [9,12]. At Misrek Badewacho District, MWH was established 3 years ago, however, it is still not well organized and its role in improving obstetric care and mother’s intention to use MWH was not studied yet. Thus the behavioral intention to use MWH is predicted by indirect factors (Socio-demographic and health seeking behavior) and proximal factors (pregnant woman's attitude, subjective norms and perceived behavioral control) [32-38]. Therefore, this study tried to show the intention of pregnant women towards the use of MWH by applying the theory of planned behavior.
Increasing health facility delivery and reducing maternal and infant deaths are targeted issue with the Sustainable Development Goal (SDG). Therefore the finding of this study will provides a contribution for attaining SDG through identifying the predictors of intention to use maternity waiting home.
Despite studies showed that utilization of MWH reduces maternal and neonatal mortality; there are limited studies conducted in Ethiopia, particularly in Misrek Badewacho district no study was conducted regarding about the issues. Thus, this study will provide further information on the utilization, intention and predictors of MWH. The maternal waiting homes act as a proxy for facility based births [39-45]. Hence intention to use MWH is crucial to its utilization. Also, this study will generate evidence based information which is useful for Misrek Badewacho district health office and Hadiya zone health department for implementing interventions that could increase MWH utilization. As well, the results obtained from this research can be used as a baseline for researchers who are interested to examine further in this area.
A Community based cross-sectional study was conducted in Misrak Badewacho district from February 20 to March 15, 2019. It is one of the rural districts in Hadiya Zone, southern Ethiopia. The district was located 97 km far from its Zonal capital, Hosanna and 121 km from capital of southern Ethiopia, Hawassa. It is located 277 km from Addis Ababa. According to 2007 Ethiopia census projection, the District had an estimated total population of 135,277 of which 67,206(49.68%) males and 68,071(50.31%) females [46,47]. Second quarter of 2018/2019 report of Misrek Badewacho district health office, showed the total number of pregnant women in the district were about 4,680. Regarding infrastructure; there are 27 health posts and all six health centers has functional MWHs.
All pregnant women found in Misrak Badewacho district were source population for this study and all pregnant women found in selected 10 kebeles during study period where the study population for this study. A pregnant woman who was registered in health post pregnant women registration book was included and pregnant women who had severe illness and unable to communicate with interviewer (who were critically ill i.e. couldn’t talk or listen) were excluded from the study.
The sample size was calculated using Epi Info Version 7 for both objectives under different assumptions and the largest sample size was taken as the final sample size. For the first objective, the sample size was calculated using single population proportion formula based on the following assumptions; 57.3% prevalence of intention to use MWH among pregnant women from a study conducted in South West Ethiopia and 95% confidence level and margin of error of 5% [11]. Accordingly, the calculated sample size was 368. But there were a total of 4680 pregnant women identified from the second quarter MBDHO report which constituted the source population. By applying the finite population correction formula, adding 10% non-response rate and 1.5 design effect the final sample was 561 pregnant women.
For the second objective the sample size was determined using double population proportion formula based on the following assumptions; 95% confidence level, Power of 80%, ratio of unexposed to exposed=1 and considering different factors which were predictors of intention to use MWH from a study conducted in South West Ethiopia and Zambia. Accordingly, factors such as place of delivery transport to and from the MWH and history of pregnancy complication were significantly associated with intention to use MWH [24].
The largest sample size of 346 was calculated for history of pregnancy complication as shown in the table below which was the sample size of the second objective. But 561 was the sample size determined for the first objective that was a larger sample size from the two sample sizes and became the final sample size required for this study (Table 1).
| Independent variable | % of outcomes in unexposed group | AOR | Sample size required | Sample size with non-response rate (10%) | |
|---|---|---|---|---|---|
| Place of delivery [24] | Home | 67.2 | 1 | 154 | 169 |
| HF | 3.36 | ||||
| Transport to and from the MWH [29] | Not affordable | 10.2 | 1 | 158 | 174 |
| Affordable | 3.61 | ||||
| History of complication [29] | No | 80.6 | 1 | 210 | 231 |
Table 1: Sample size calculation for different factors associated with intention to use MWH among pregnant women in Misrak Badewacho District, Hadiya Zone, Southern Ethiopia, 2019.
Multi-stage sampling technique was used. Among 27 rural Kebeles 10 kebele was selected with Probability Proportional to Size (PPS). Then sample size, 561 pregnant women was allocated to selected 10 kebeles with population proportion to size allocation (Figures 1 and 2).Then the participants were selected by using a simple random sampling technique from the pregnant women registration book found in health posts. After drawing the participants, interviews were conducted by face to face in their home (Figure 1).
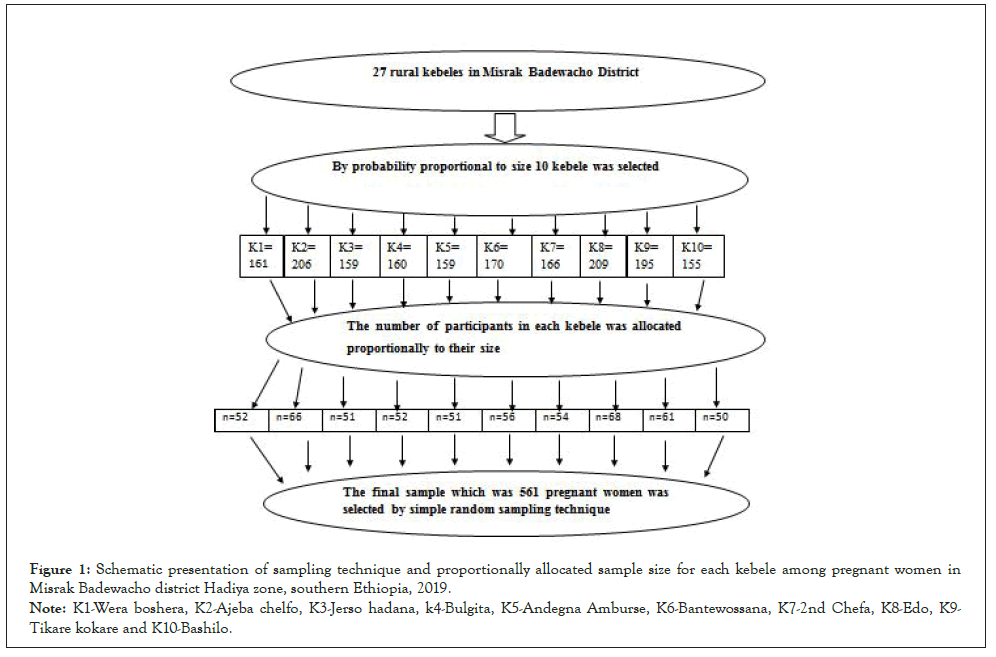
Figure 1: Schematic presentation of sampling technique and proportionally allocated sample size for each kebele among pregnant women in
Misrak Badewacho district Hadiya zone, southern Ethiopia, 2019.
Note: K1-Wera boshera, K2-Ajeba chelfo, K3-Jerso hadana, k4-Bulgita, K5-Andegna Amburse, K6-Bantewossana, K7-2nd Chefa, K8-Edo, K9-
Tikare kokare and K10-Bashilo.
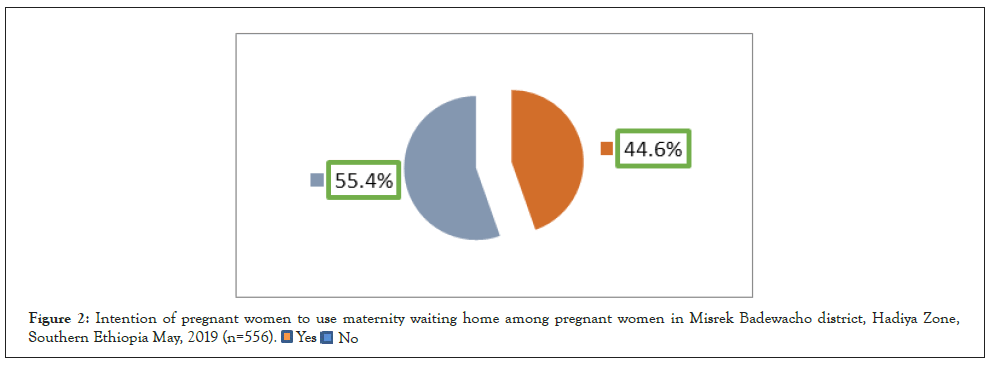
Figure 2: Intention of pregnant women to use maternity waiting home among pregnant women in Misrek Badewacho district, Hadiya Zone,
Southern Ethiopia May, 2019 (n=556).
The pretested and structured questionnaire was used as a data collection tool which was based on the variables described by the theory of planned behavior and as well as findings from a previous Jimma district study [11,32,33]. After general instructions were provided, socio-demographic variables (i.e. age, marital status, religion, educational status, occupation and family monthly income) were measured. Maternal health services utilization (gravidity, giving birth, ANC visits, pregnancy complication, place of delivery, past experience of MWH, days of staying in MWH and reason to stay at MWH) was assessed. The last section consisted of the measures of the psychosocial variables attitude, perceived social norms, and perceived behavioral control. The main outcome variable was intending to use a MWH during current pregnancy. To measure TPB component, 52 item questionnaires that consisted of four major constructs were included.
7 Attitude toward behavioral beliefs and 7 evaluation of outcomes of indirect measure items, and 4 direct measure items); subjective norm (6 normative beliefs and 6 motivation to comply indirect measure items, and 4 direct measure items); perceived behavioral control (5 control beliefs and 5 perceived power indirect measures items and 4 direct measure items); and the intention (4 items) [11,32].
Attitude towards to use MWH was measured both indirectly and directly. Indirect attitude was assessed in terms of two aspects: 7 behavioral beliefs about to use MWH (i.e., “staying in MWH for institutional delivery 15 days before giving birth will help me to get health child.”) and, 7 corresponding outcome evaluations of use to MWH (i.e., “For me, getting healthy child is,…”). The belief items had possible responses ranging from 1=“strongly disagree to 5= strongly agree” while the corresponding evaluation outcome items had possible responses ranging from 1=”very bad” to 5=”very good”. The score for the assessment of indirect attitude was calculated by multiplying the numerical value of each of the behavioral beliefs items by the numerical value of its corresponding outcome evaluation items, and then summing the multiplied scores across all items. Total scores could range from 7 to 175, with higher scores indicating positive beliefs and outcome evaluations with regard to use MWH during institutional delivery. Direct attitude toward MWH use was assessed with 4 items that consisted of bipolar adjective pair (bad/good, useless/useful, unpleasant/pleasant and boring/interesting). Each item assessed using 5 point semantic differential response range (i.e. 1=extremely negative direction to 5=extremely positive direction). A total score for direct attitude, ranging from 4 to 20 was observed by summing across all items and higher scores indicated a more positive attitude toward MWH use during pregnancy.
The same principle was applied for subjective norm which was measured with both indirect SN (normative beliefs and motivation to comply with total score was ranging from 12 to 150) and direct SN range from 4 to 20. With higher scores reflecting greater influence of significant others regarding whether women should use MWH during institutional delivery. Regarding perceived behavioral control indirect PBC (control beliefs and perceived power with total score was 5 to 125) and total score of direct PBC was ranging from 4 to 20. By summing across all direct PBC items and higher scores indicated a more positive PBC toward MWH use among pregnant women. But to get more positive indirect PBC towards MWH the items were reverse coded and then the higher score indicated the more favorable indirect PBC towards MWH. Finally intention was assessed by four Likert scale items with a total score ranged from 4 to 20 with higher scores reflecting a greater intention to use MWH during institutional delivery.
First, the questionnaire was developed in English, translated into Hadiyissa and Amaharic by an independent bi-lingual expert, and then back-translated into English. The data were collected from respondents through face-to-face interviews with selected participant in their home with pre-tested structured questionnaire. The final version of the questionnaire was in Hadiyissa but Amaharic questionnaire was used for those respondents who were unable to respond by Hadiyissa. Six diploma nurses who were fluent in speaking Hadiyissa language recruited as data collectors from health centers and two diploma nurses were recruited as supervisors. They were trained for two days by the principal investigator on the study instrument, consent form and data collection procedure.
Data were coded and entered into Epi data statistical software version 3.1 and exported to the Statistical Package for the Social Sciences (SPSS) version 20 soft-ware for statistical analysis. Descriptive statistics (frequencies, percentages, mean values, and standard deviations were calculated for socio-demographic, health service utilization and direct and indirect components of TPB used to describe the data. The mean split procedure on the psychosocial measures such as intention to MWH, direct attitude, direct SN direct PBC and indirect TPB components were performed and those scored below mean were low and above the mean were high. All independent variables with p-value <0.25 in the crude analysis were entered into the multivariable logistic regression model to assess the association between dependent and independent variables. Then the multivariable logistic regression model was used to identify independent factors associated with intention to use MWH among pregnant women by controlling the effect of confounders. The model fitness was assessed by Hosmer– Lemeshow goodness-of-fit statistic test. Adjusted Odds Ratios (AORs) with 95% CI were used to measure the magnitude and significance of associations.
Data quality was assured by carrying out the careful design of data extraction formats, appropriate recruitment of data collectors and by giving adequate training and follow-up for data collectors and supervisors. Before actual data collection the questionnaire was pretested on pregnant mothers from non-selected kebele of the district in 28 (5%) of the final sample. The Likert scale items had Cronbach’s Alpha value is 0.89. The investigator and supervisors did intensive supervision during the whole period of data collection. To confirm the reliability of data during data collection, the investigator reviewed a random sample of questionnaires and the supervisors made random cross checks for their completeness, accuracy, and consistency.
Ethical clearance was obtained from the Institutional Review Board of the College of Medicine and Health Sciences of Hawassa University before conducting the study. After securing ethical clearance from the board, MBDHO was informed about the objective of the study through a support letter from the School of Public Health and written permission was obtained from the district health office before starting data collection. To keep the confidentiality of the study subjects’ information, personal identifiers were not included in the data collection format and all recorded data were kept in a very secure area where only principal investigator can access to it.
A total of five hundred fifty six pregnant women were participating with a response rate of 99.1%. The mean age of participants was 27.63 (SD ± 5. 282) years. Two hundred nineteen (39.3%) were age category between 25-29 years. Five hundred thirty two (95.68%) were protestant religion followers and around 489 (88%) participants were Hadiya. One hundred ninety four (34.9%) participants had secondary education. Five hundred forty three (97.6%) were married and 419 (75.4%) participants were house wife in their job. Two hundred nineteen (39.4%) respondents had earned monthly family income from 500 to 999 Ethiopian Birr (Table 2).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Age in years | |||
| 15-24 | 173 | 34.5 | |
| 25-29 | 219 | 39.4 | |
| 30 and above | 164 | 26.1 | |
| Religion | |||
| Protestant | 523 | 94.1 | |
| Others* | 33 | 5.9 | |
| Ethnicity | |||
| Hadiya | 489 | 88 | |
| Kembata | 35 | 6.3 | |
| Wolaita | 18 | 3.2 | |
| Others** | 14 | 2.5 | |
| Marital status | |||
| Married | 543 | 97.6 | |
| Widowed | 13 | 2.4 | |
| Educational status | |||
| No formal education | 80 | 14.4 | |
| Primary education | 175 | 31.5 | |
| Secondary | 194 | 34.9 | |
| Preparatory and above | 107 | 19.2 | |
| Current occupation | |||
| House wife | 419 | 75.4 | |
| Government employee | 46 | 8.3 | |
| Merchant | 91 | 16.4 | |
| Monthly income | |||
| ≤499 birr | 200 | 36 | |
| 500 to 999 birr | 219 | 39.4 | |
| ≥1000 | 137 | 24.6 | |
Note: others*, Orthodox= 16, Catholic = 10, Musilm =7, others**, Amhara =8, Halaba =6
Table 2: Socio demographic characteristics of pregnant women in Misrak Badewacho District, Hadiya zone southern Ethiopia, May, 2019 (n=556).
Regarding maternal health service utilization, 286 (51.4%) participants had one to two pregnancy experiences. Three hundred thirty one (75%) participants gave birth to their last child at the health facility. Four hundred seventy nine (86.2%) pregnant women did not develop pregnancy complications. Two hundred seventy one (48.7%) respondent had three or above ANC visit. One hundred thirteen (20.3%) participants had past MWH experience and 69 (61%) pregnant women were staying less than 15 days. About 96 (85%), 66(58.4), 43(38) and 35(31%) of the respondents who ever used MWH mentioned reasons to use MWH was to get better health service, due to distance, due to past pregnancy complication and no/ low cost respectively (Table 3).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Gravidity | |||
| Primgravida | 115 | 20.6 | |
| Multigravida | 286 | 51.4 | |
| Grandmultigravida | 155 | 28 | |
| Giving birth | |||
| Yes | 441 | 79.3 | |
| No | 115 | 20.7 | |
| Place of delivey(n=441) | |||
| Heath facility | 331 | 75 | |
| Home | 110 | 25 | |
| Pregnancy complications | |||
| Yes | 77 | 13.8 | |
| No | 479 | 86.2 | |
| ANC visit | |||
| No visit | 61 | 11 | |
| One or two | 224 | 40.3 | |
| Three or above | 271 | 48.7 | |
| Past MWH experience | |||
| Yes | 113 | 20.3 | |
| No | 443 | 79.7 | |
| Length of stay at MWH(n=113) | |||
| <15 days | 69 | 61 | |
| ≥ 15 days | 44 | 39 | |
Table 3: Health service utilization of pregnant women Misrak Badewacho District, Hadiya zone southern Ethiopia, May, 2019 (n=556).
Three hundred sixty five (65.6%) pregnant women had a good attitude toward MWH with mean the score of 12.8 (SD+5.26). Regarding individual item score three hundred ninety eight (71.5%) respondents were reported that MWH is good. Three hundred (54%) respondents were reported that MWH is boring.
Regarding subjective norm 230 (41.4%) respondents had favorable subjective norm toward MWH with a mean score of 14.1 (SD+5.57). Two hundred eighty five (51.3%) respondents were reported that most people who are important to me will think that I should stay in MWH.
Two hundred fifty four (45.7) pregnant women had favorable PBC with a mean score of 13.3 (SD+5.41). Regarding the individual item score 286 (51.4%) and 270 (48.6%) pregnant women reported staying in MWH is difficult and easy respectively (Table 4).
| variable | Category | Frequency | percent |
|---|---|---|---|
| Direct attitude | Good | 365 | 65.6 |
| Poor | 191 | 34.4 | |
| Direct SN | Favourable | 230 | 41.4 |
| Unfavourable | 326 | 58.6 | |
| Direct PBC | Favourable | 254 | 45.7 |
| Unfavourable | 302 | 54.3 |
Table 4: Direct theory of planned behavior components measurement result of pregnant women in Misrak Badewacho District, Hadiya zone southern Ethiopia, May, 2019 (n=556).
More than two third (74.3%) of respondents were agreed to stay at MWH will help to get delivery service by a health professional and prevent from pregnancy complications. The evaluation outcome result showed that three hundred fifty three (63.5%) respondents agreed that using MWH is important to get healthy child (Table 5).
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Indirect attitude | Good | 347 | 62.4 |
| Poor | 209 | 37.6 | |
| Indirect SN | Favourable | 247 | 44.4 |
| Unfavourable | 309 | 55.6 | |
| Indirect PBC | Favourable | 314 | 56.5 |
| Unfavourable | 242 | 43.5 |
Table 5: Indirect theory of planned behavior components measurement result of pregnant women in Misrak Badewacho District, Hadiya zone southern Ethiopia, May, 2019 (n=556).
Three hundred twenty four (58%) pregnant women agreed that Health Extension Workers (HEWs) think pregnant women should stay in MWH. The strength of normative belief evaluated using motivation to comply of each normative belief also showed that; Two hundred ninety seven (54%) pregnant women reported that their husband's approval for using maternity waiting home was very important.
Almost two third (66%) of respondents were agreed that lack food makes difficult to staying in MWH. About three hundred thirty (59.4%) pregnant women were reported that the lack of individual that can take them in to MWH made use of MWH very hard. The result of the power of control belief measurement also indicates that about 411 (73.9%) participants was answered availability of food will make easier the use of in MWH. Three hundred thirty nine (61%) respondents agreed that the presences of persons that can give care for family members make easy use MWH mentioned in Table 5.
The mean scores of Direct attitude, subjective norm and perceived behavioral control, were 14.1 (SD+2.85) 12.8 (SD+3.24) and 13.3 (SD+5.41) respectively. Indirect attitude, indirect subjective norm and indirect perceived behavioral control had mean scores of 99.82(SD+27. 89), 85.23(SD+24. 37) and 58.09(SD+25. 9) respectively. The outcome variable, intention had mean score of 12.55(SD+6.5).
About 248(44.6%) pregnant women were intended to use MWH with 95% CI(41%, 48%). And the mean score of respondents was 12.55(SD+6.5) (Figure 2).
As Bivariate analysis shows that variables such as respondent age, educational status, monthly income, gravidity, giving birth, ANC visit, and pregnancy complication, past experience of MWH, direct attitude, subjective norm and direct perceived behavioral control were significantly associated with intention to use MWH (Table 6).
| Intention to use MWH | ||||
|---|---|---|---|---|
| Variable | Yes (%) | No (%) | COR(95% CI) | p-value |
| Age in year | ||||
| 15-24 | 73(29.7) | 100(32.5) | 1 | |
| 25-29 | 94(38) | 125(40.5) | 1.03(0.68, 1.5) | 0.39 |
| 30 and above | 81(32.3) | 83(27) | 1.3(1.07, 2.05) | 0.186* |
| Marital status | ||||
| Married | 241(97) | 302(98) | 1 | |
| Widowed | 7(2.8) | 6(2) | 1.4(0.48, 4.4) | 0.5 |
| Educational status | ||||
| No formal | 31(12.5) | 49(16) | 1 | |
| Primary | 40(16) | 135(43.8) | .0.46(0.26, 1.02) | 0.89 |
| Secondary | 98(38.5) | 96(31.2) | 1.6(0.95, 2.7) | 0.77 |
| Preparatory and above | 79(32) | 28(9) | 4.5(2.4, 8.3) | <0.001* |
| Occupation | ||||
| House wife | 195(79.4) | 224(72.7) | 1 | |
| Gov. employer | 19(7.6) | 27(8.7) | 0.8(0.46, 1.4) | 0.5 |
| Merchant | 34(13) | 57(18.6) | 0.68(0.43, 1.092) | 0.45 |
| Monthly income | ||||
| ≤ 499 birr | 82(32.2) | 118(38.3) | 1 | |
| 500- 999 birr | 92(37) | 127(41.2) | 1.042(0.70, 1.5) | 0.834 |
| ≥1000 | 74(29.8) | 63(20.5) | 1.7(1.2, 2.62) | 0.019* |
| Gravidity | ||||
| Primgravida | 47(19) | 68(22) | 1 | |
| Multigravida | 126(50.8) | 160(52) | 1.13(0.73, 1.76) | 0.57 |
| Grandmultigravida | 75(30.2) | 80(26) | 1.3(1.08, 2.2) | 0.01* |
| Ever given birth | ||||
| Yes | 208(84) | 233(75.6) | 1.6(1.092, 2.6) | 0.18* |
| No | 40(16) | 75(24.4) | 1 | |
| ANC visits | ||||
| No visit | 22(8.8) | 39(12.6) | 1 | |
| One or two | 71(28.6) | 153(49.6) | 0.82(0.45, 1.5) | 0.52 |
| Three or above | 155(62.6) | 116(37.8) | 2.4(1.33, 4.2) | 0.003* |
| Pregnancy complication | ||||
| Yes | 43(17.3) | 34(11) | 1.7(1.041, 2.75) | 0.034* |
| No | 205(82.7) | 274(89) | 1 | |
| Place of delivery (n=441) | ||||
| Heath facility | 166(76.5) | 165(73.6) | 1.16(0.75, 1.79) | 0.45 |
| Home | 51(23.5) | 59(26.4) | 1 | |
| Experience of MWH | ||||
| Yes | 73(29.4) | 40(13) | 2.79(1.18, 4.3) | <0.001* |
| No | 175(70.6) | 268(87) | 1 | |
| Length of saty (n=113) | ||||
| <15 days | 45(62.2) | 24(60) | 1.07(0.68, 1.87) | 0.35 |
| ≥15 days | 28(37.8) | 16(40) | 1 | |
| Direct attitude | ||||
| Good | 191(77) | 174(62.7) | 2.6(1.8, 3.7) | <0.001* |
| poor | 57(23) | 134(37.3) | 1 | |
| Direct SN | ||||
| Favourable | 115(46.4) | 115(37.3) | 1.4(1.089, 3.5) | 0.032* |
| Unfavourable | 133(54.6) | 193(62.7) | 1 | |
| Direct PBC | ||||
| Favourable | 144(58) | 110(35.7) | 2.5(1.7, 3.5) | <0.001* |
| Unfavourable | 104(42) | 198(64.3) | 1 | |
| Indirect attitude | ||||
| Good | 162(65.3) | 185(60) | 1.25(0.885,1.8) | 0.27 |
| poor | 86(34.7) | 123(40) | 1 | |
| Indirect SN | ||||
| Favourable | 122(49.6) | 125(40.6) | 1.4(0.86, 3.0) | 0.92 |
| Unfavourable | 126(50.4) | 183(59.4) | 1 | |
| Indirect PBC | ||||
| Favourable | 138(55.6) | 176(57.1) | 0.941(0.672, 1.3) | 0.72 |
| Unfavourable | 110(44.4) | 132(42.9) | 1 | |
Note: *= p <0.25
Table 6: Factors associated with intention to use MWH in bi-variate analysis, among pregnant women in Misrak Badewacho District, Hadiya zone southern Ethiopia, May, 2019 (n=556).
Multivariate analysis showed that respondent educational status, ANC visit, past experience of MWH; the direct attitude and direct perceived behavioral control were significantly associated with pregnant women intention to use MWH. Those respondents who educated preparatory or above were 4 times more intended to use MWH than those who had no formal education (AOR=4, 95%CI: 2.05,8.6). Respondents with three or above ANC visits were 3.7 times more likely intended to utilize MWH than those who had no ANC visit (AOR=3.7,95%CI: 2,7.2). Past experience of utilizing MWH home were significantly associated with intention, those who used MWH at previous delivery were 2.6 times more likely expressed their intention to use MWH than non-users (AOR=2.6,95% CI: 1.6,4.3). Pregnant women with a good attitude towards use of MWH were 2.3 times highly intended to use MWH when compared with those who had a poor attitude towards MWH (AOR=2.3,95% CI: 1.5,3.5). Those respondents who had favorable perceived behavioral control were 3.3 times more intended to use MWH than those with unfavorable perceived behavioral control (AOR=3.4, 95%CI: 2.1, 4.9) (Table 7).
| Intention to use MWH | ||||
|---|---|---|---|---|
| Variable | Yes(%) | No (%) | COR(95% CI) | AOR(95%CI) |
| Age in years | ||||
| 15-24 | 73(29.7) | 100(32.5) | 1 | 1 |
| 25-29 | 94(38) | 125(40.5) | 1.03(0.68, 1.5) | 0.96(0.59, 1.5) |
| 30 and above | 81(32.3) | 83(27) | 1.3(1.07, 2.05) | 1.6(0.9,2.8) |
| Educational status | ||||
| No formal | 31(12.5) | 49(16) | 1 | 1 |
| Primary | 40(16) | 135(43.8) | 0.46(0.26,1.02) | 0.56(0.30, 1.06) |
| Secondary | 98(38.5) | 96(31.2) | 1.6(0.95,2.7) | 1.7(0.9,3.2) |
| Preparatory and above | 79(32) | 28(9) | 4.5(2.4, 8.3) | 4(2.1, 8.2)** |
| Monthly income | ||||
| ≤499 birr | 82(32.2) | 118(38.3) | 1 | 1 |
| 500- 999 birr | 92(37) | 127(41.2) | 1.042(0.70, 1.5) | 0.85(0.52, 1.3) |
| ≥1000 | 74(29.8) | 63(20.5) | 1.7(1.2, 2.62) | 1.3(0.77, 2.3) |
| Gravidity | ||||
| Primgravida | 47(19) | 68(22) | 1 | 1 |
| Multigravida | 126(50.8) | 160(52) | 1.13(0.73, 1.76) | 1.02(0.6, 1.75) |
| Grandmultigravida | 75(30.2) | 80(26) | 1.3(1.08, 2.2) | 1.6(0.8, 3.2) |
| Ever given birth | ||||
| Yes | 208(84) | 233(75.6) | 1.6(1.092, 2.6) | 1.4(0.8, 2.3) |
| No | 40(16) | 75(24.4) | 1 | 1 |
| ANC visit | ||||
| No visit | 22(8.8) | 39(12.6) | 1 | 1 |
| One or two visit | 71(28.6) | 153(49.6) | 0.82(0.45, 1.5) | 1.4(0.73, 2.8) |
| Three or above | 155(62.6) | 116(37.8) | 2.4(1.33, 4.2) | 3.7(2, 7.2)** |
| Pregnancy complication | ||||
| Yes | 43(17.3) | 34(11) | 1.69(1.041,2.75) | 1.7(0.97, 3) |
| No | 205(82.7) | 274(89) | 1 | 1 |
| Experience of MWH | ||||
| Yes | 73(29.4) | 40(13) | 2.7(1.18, 4.3) | 2.6(1.6, 4.3)** |
| No | 175(70.6) | 268(87) | 1 | 1 |
| Direct attitude | ||||
| Good | 191(77) | 174(62.7) | 2.58 (1.8, 3.7) | 2.3(1.5, 3.5)** |
| Poor | 57(23) | 134(37.3) | 1 | 1 |
| Direct SN | ||||
| Favourable | 115(46.4) | 115(37.3) | 1.4(1.089, 1.9) | 1.3(0.85, 2) |
| Unfavourable | 133(54.6) | 193(62.7) | 1 | 1 |
| Direct PBC | ||||
| Favourable | 144(58) | 110(35.7) | 2.5(1.7, 3.5) | 3.3(2.1, 4.9)** |
| Unfavourable | 104(42) | 198(64.3) | 1 | 1 |
Note: *= p <0.25
Table 7: Factors associated with intension to Use MWH in multivariate analysis among pregnant women in Misrak Badewacho District, Hadiya zone southern Ethiopia, May, 2019 (n=556).
The aim of this study was to highlight intention to use maternity waiting home among pregnant women in the Misrek Badewacho District, Hadiya Zone. Despite the existence of MWHs in Ethiopia for more than three decades, the prevalence of intention to use MWH was very limited. In the study area which showed that only 248(44.6%) pregnant women were intended to use MWH.
The finding of this study was comparable to the study from Kenya, which revealed that only 147(45%) women were intended to use MWH [22]. The possible reasons for this comparable achievement could be most of the respondents were dependent on important persons such as their husbands to use or not to use and also both countries economically have low income.
The result of this study was higher than the survey conduct at four regions of Ethiopia, which revealed that only 22(17%) respondents were intended to use MHW [27]. The variation could be due to geographical coverage; this study was conducted on specific areas, whereas the pervious was conducted in four regions, socio-demographic, economic and cultural difference between the two groups.
The result of this study was lower than other findings which was done in the Eastern Gurage Zone and Jimma district with a result of 235(55.1) and 219(57.3%) respectively [11,29]. The variation could be due to the difference between study population; in this study those women who had visible pregnancy regardless of number of ANC visits were included, whereas, the previous studies included pregnant women who had at least ANC one. The other reasons might be study setting; this study was community based, whereas the study from Jimma was facility based and sample size; both previous studies had small sample size and social demographic, economic and cultural variability between the study settings could increase the variation.
Overall, the finding of this study was lower when compared with the findings of cross sectional survey from the rural district of Zambia; which assessed the behavioral intention to use a MW between health facilities with and without MWH [24]. The utilization study from Kalabo district of Zambia revealed that almost all respondents 322(97%) were expressed their willingness to stay in MWH if it was available. Another cross sectional study from Zambia, on personal and environmental predictors of the intention showed that 567(57.1) respondents were intended to use MWH [38]. In a rural district of Ghana, Zimbabwe and Zambia 90%, 66.6% and 94% of participants were expressing their willingness to stay in MWH respectively [10]. Despite the high cost of MWH, the result from rural Kenya showed higher willingness 234(61.1%) of women to use MWH [42]. The most probable variation of this result could be that due to sample size; except a Zambian study, almost all studies had smaller sample size, due to study setting this study was community based were as all studies were facility based and may be the variation in health policy and social background between countries.
This study showed that among the socio-demographic variables respondent educational status had statistically significant association with the intention to use MWH. Those respondents who had preparatory and above educational level were 4 times more intended than those who had no formal education.
This result was parallel with the result of the Eastern Gurage Zone, Debra Markos, Zambian and Peru which showed that the intender group was those mothers with secondary or higher level than mothers with no formal education [4,24,29,39]. This is due to that maternal education strongly associated with all types of health behavior. These include increased knowledge of the benefits of MWH and awareness of health services, higher approach to new health-related information, and better communication with the husband, more decision-making power, increased self-worth and self-confidence.
Among health service utilization ANC visit was predictor of intention to use MWH among pregnant women. Those pregnant women who have three or above ANC visits had 3.7 times more likely intended to use MWH than those who haven’t ANC visits.
The finding of this study was consistent with the study from Debra Markos Town, the two studies from Zambia, Ghana and Zimbabwe which revealed about almost all of MWH intended women had ANC visits [10,24,38,39]. This might be those pregnant women with more ANC visits had the opportunity to know about usefulness of MWH, heard about dinger signs of pregnancy and labor and delivery complication during their visits, which in turn informs their decisions on where to deliver.
The finding of this study revealed that 113(20.3%) of pregnant women had past experience of maternity waiting home. Those who used MHW in pervious pregnancy were 2.6 times more intended to use MWH again at current pregnancy than non-users.
This result showed that there was a relatively improved utilization experience among respondents than the result from Jinka hospital and Ghana in 86(16.7%) and one (4%) of mothers had used MWH respectively [9,10]. The variation could be due to residency of respondents; the study from Jinka hospital included respondents both from urban and rural whereas this study included respondents from only rural and the lower achievement in rural district of Ghana could be due to strong financial barriers: home delivery was less expensive; Costs of living were higher in a MWH and in addition, women could not take care of their families and their farms but instead of this study there were no direct costs for MWH and facility delivery services in study area. Also the other reasons could be existence of health developmental army, HEWs, community involvement and variation in social background between groups.
But the finding of this study was lower than studies done in Jimma and Tanzania, Zimbabwe and the qualitative and quantities studies from Zambia [10,11,16,24,41]. The variation could be attributed to difference in study setting; this study is community based whereas the previous studies were facility based, also may be cultural and socio-demographic variations between the study settings could increase the variation and except study from Jimma district, the difference in countries health policy might influence the variation.
This study showed that direct attitude was significantly associated with intention to use MWH. Those who had good attitude toward intention to use MWH were 2.3 times more likely expressed their willingness toward MWH than those who had poor attitude.
The result of this study was in line with the cross sectional studies from Jimma, wolaita soddo and the two studies from Zambia which revealed that high intenders were those who had favorable/good attitude toward maternal health services [11,24,37,38]. These similarities could be due to respondents had good awareness about their health, usefulness of maternal health services, involvement of community, hard work on health extension packages and they were informed about the danger signs of pregnancy and where to give birth during ANC visits.
But this study was in contrast with the qualitative study from rural Zambia that showed most respondents had a negative attitude toward service utilization [43]. The variation might be due to that Zambian health professional’s lacks Compassionated and Respectful Care (CRC) and they may disrespect pregnant women when they had contact but the Ethiopian government emphasized on CRC. The other reasons may be cultural, socioeconomic and demographic variation between the countries.
Four hundred thirteen (74.3%) respondents were reported staying at MWH help me to get delivery service by a health professional and prevent me from pregnancy complication. The evaluation outcome result showed that three hundred and fifty three (63.5%) respondents agreed that using MWH is important to get healthy child.
The finding from this study revealed that direct perceived behavioral control was statistically associated with intention to use maternity waiting home. Those pregnant women who had favorable direct perceived behavioral control were 3.3 times more likely expressed their intention to use MWH than those who had unfavorable direct perceived behavioral control.
The finding of this study was comparable to the study of Jimma district and Zambian study, which showed perceived behavioral control being the strongest predictor of intention [11,38]. The result revealed that, even the intended respondents were reported that they perceived several internal and external barriers which made them more likely to perceive less control over the intended behavior. Thus, examination of the variations between intenders and non-intenders showed that non intenders experienced more barriers to use the services. Thus, these findings lead to improving women’s perceived behavioral control could significantly raise women’s intentions to use MWH.
This study showed that about 286(51.1%) pregnant women reported that using MWH was difficult and almost two third (66%) of respondents were agreed that food insecurity makes the difficulty of staying in the maternity waiting home. The finding was higher than the study done in Jimma and the two studies conducted at national level [11,12,27]. This variation was due to study setting; this study was conducted at the community level where as the previous were conducted at health institutions, thus, pregnant women who visited health facilities and had ANC follow up were more informed about MWH regardless of their food security. Also the other reasons could be the respondent sample size, past exposure to MWH, cultural, socioeconomic and demographic factor may increase the variation between the studies.
However, there are some limitations, in this study, that need to be taken into consideration when utilizing the results. First, these findings are based on interviewer-administered questionnaires. The respondents’ responses may have been influenced by the interviewer’s presence, the manner in which the questions were posed. In addition, the cross-sectional design of the study made it not possible to identify causal relationships between intention and the hypothesized predictor variables from the TPB model.
The study revealed that nearly half (44.6%) of pregnant women were intended to use MWH, Considering these findings, the following conclusions can be made. To conclude respondents preparatory or higher education, three or above ANC visit, past MWH experience, favorable attitude and favorable perceived behavioral control were significantly associated with the intention of pregnant women to use MWH. These results can serve as a basis for public health interventions focusing on improving access to facility-based skilled birth attendance.
[Google scholar] [Pubmed]
Citation: Obola TD, Leimengo TY, Herut BM, Kebede DL (2022) Intention to use Maternity Waiting Home and Determinant Factors among Pregnant Women in Misrak Badewacho District, Hadiya Zone, Southern Ethiopia: A Cross Sectional Study. Reprod Syst Sex Disord.11:322.
Received: 30-May-2022, Manuscript No. RSSD-22-17677; Editor assigned: 02-Jun-2022, Pre QC No. RSSD-22-17677(PQ); Reviewed: 22-Jun-2022, QC No. RSSD-22-17677; Revised: 30-Jun-2022, Manuscript No. RSSD-22-17677(R); Published: 08-Jul-2022 , DOI: 10.35248/2161-038X.22.11.322
Copyright: © 2022 Obola TD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.