Journal of Fertilization: In Vitro - IVF-Worldwide, Reproductive Medicine, Genetics & Stem Cell Biol
Open Access
ISSN: 2375-4508
ISSN: 2375-4508
Review Article - (2015) Volume 3, Issue 1
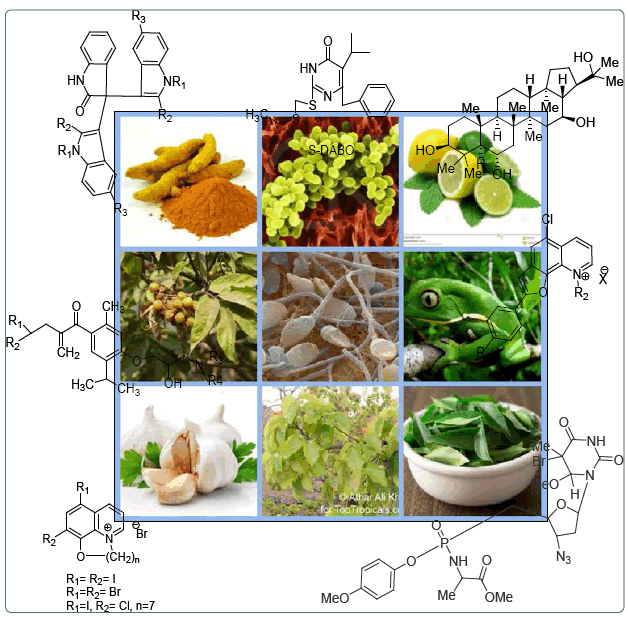
Spermicides came into existence as a method of contraception for over hundred years. Since then, investigations and developments in this field have led to more and more fruitful as well as promising results but still left enough scope for further studies. The titled article manifests a brief discussion on the development of spermicides from different natural and synthetic sources, a compilation of the promising molecules and even extracts and includes an outline of the basic physiology behind the bioactivity. Since spermicides are only one among several other methods of contraception adopted and practiced, an attempt has been made to probe the necessity and advantage of spermicides over other modes of contraception, emphasizing on the requirements and scope of future investigations in this field.
<Keywords: Spermicide; Contraception
The growing population is a global problem with grave implications for the future. A report of the United Nations dated October 2011 reveals that the earth’s population has passed seven billion [1]. The figure is double of that (3.5 billion) in 1968 and is estimated to increase by two more billions by the year 2050 [1]. Importantly, more than 90% of the world’s future population growth is projected to take place in the developing world, where countries are already struggling to provide their people with food, water, health care, education and jobs [2]. Moreover, nearly 215 million women in the developing world want, but do not have access to, modern contraception, which leads to unintended pregnancies, unsafe abortions, maternal and child mortality and morbidity, reduced access to education and a whole range of other negative consequences [3]. Unintended pregnancy is a fundamental problem asking for better, more accessible methods of contraception, and constitutes a fundamental public health need in today’s world. Nearly 60 percent of all pregnancies in the United States and anywhere from 24 to 64 percent of all pregnancies worldwide are unintended, either because they were mistimed or because they were not wanted at all [4]. Effective family planning facilities and newer contraceptive modalities are in great demand to combat this alarming situation. It is now generally accepted that the currently available methods of fertility regulation are inadequate to meet the varied and changing personal needs of couples at different times in their reproductive lives. The available contraceptive options are limited in their scope to respond to variability in individual and family situations, to cultural differences, to specific health problems and shifting personal preferences, and to life cycle stages and changing reproductive intentions across those stages. Although various physical and chemical methods apart from male and female sterilization have been in use to prevent unwanted pregnancies, none of the approaches can be considered as ideal. Though oral contraceptive pills are preferred by gynecologists as the safest drugs for preventing unwanted pregnancies, they fail to give protection against STIs. The barrier methods of contraception presently available, e.g., diaphragm, cervical cap, contraceptive sponge and spermicides, appear to put the users at higher risk of vaginal infection, urinary tract infection and possibly toxic shock syndrome. Vaginal contraceptive products that have been available for many years usually contain the membrane surfactant nonoxynol-9 (N-9) as one of the main ingredients [5]. However, the major drawback of using N-9 or other surfactants lies in their detergent-type cytotoxic effect on vaginal cells [6]. Besides, N-9 is also known to inactivate Lactobacilli, which form the normal flora in vaginal tissues [7]. Disturbance of the vaginal micro flora increases the vulnerability to vaginal infections, which in turn enhances the chances of STI/HIV transmission [8]. Hence, in the present global scenario with alarming population growth and increasing threats of AIDS and other STDs, development of vaginal spermicidal microbicides lacking detergent-type cytotoxicity may offer a significant clinical advantage over the currently marketed spermicides. We therefore decided to review the history of research in the field of vaginal contraceptives with special emphasis on the development of safer, more effective spermicides as summarized in this review.
Fertilization in mammals is a multi-step process that terminates in the fusion of the sperm and oocyte plasma membrane in the oviduct. During the menstrual cycle, mature egg released from the ovarian follicle enters and begins to travel through the fallopian tube and remains viable in the oviduct for about 24 hr. At ejaculation, sperm is deposited into the vagina and must overcome a series of barriers in their journey from vagina to oviduct, each of which eliminates a substantial proportion of the original population of sperm. It will live for an average of three days in the female reproductive tract and for successful fertilization, live and motile sperm has to reach the oviduct within this time. Sperm must locate and penetrate the awaiting egg while it is in the fallopian tube. Post-epididymal spermatozoa are motile cells, and sperm motility becomes critical at the time of fertilization because it allows or at least facilitates the passage of the sperm through the isthmus part of the oviduct at the ipsilateral side where ovulation takes place [9-11].
The basis of barrier methods of contraception is to prevent entry of sperm into the endo-cervical region of the reproductive tract. This can be achieved either by putting a mechanical barrier, or a chemical barrier that may render the cervico-vaginal milieu unfavorable for sperm survival or transport, thereby blocking the successful union of gametes. Also, the barrier methods are a good choice for couples that need a back-up method while waiting for another method to take effect, or after using oral contraceptives inconsistently, or having intercourse infrequently.
Barrier methods of contraception can be classified into three major categories as follows:
• Mechanical barrier: includes the male condom, female condom, diaphragm, cervical cap, and sponge.
• Chemical barrier or spermicides: Spermicides are agents that kill spermatozoa or render them incapable of normal function. A spermicide may act at or near the exocervix to kill spermatozoa before they enter the upper female genital tract. They are available in topical formulations as foams, creams, gels, films or suppositories, which are often used for contraception in conjunction with mechanical barriers and other devices.
In contrast to agents that must be taken orally or implanted in the body, vaginal contraceptives are known as coitus related or episodic products; in that they only need to be used when sexual activity is imminent. Thus, females are not exposed to the agent through the month, as they are with oral contraceptives, intrauterine devices, implanted inserts or depot injections. They are free from side effects of systemic exposure to the contraceptive agents. The barriers are the only devices that may afford some protection during a sudden necessity. Moreover, breastfeeding women who need contraception may use spermicides since these preparations usually increase vaginal lubrication, can be used immediately after childbirth, and have no hormonal side effects. These methods may be suggested for women over 40 and those with contraindications to oral contraceptives and IUDs (intrauterine devices)
• Combined physicochemical barrier: The spermicidal agents, when used alone, provide some contraceptive protection, but are best when used with another barrier method. This forms the basis of developing combined physicochemical barrier method of contraception. The effectiveness of barrier methods may be increased when two or more options are combined together. For example, latex condoms are available with a coat of spermicide. Use of dual protection is particularly attractive when there is a need to reduce the risk of sexually transmitted infections (STIs) including human immunodeficiency virus (HIV) along with preventing unwanted pregnancy. Multiple methods to eliminate STDs and improve contraceptive effectiveness, particularly where one or more methods is controlled by the woman, will increase consistent use of at least one.
Spermicides as discussed earlier are a biologically effective way of interrupting fertility and have the advantage that they do not depend on highly skilled personnel for their prescription and use. Spermicidal agents are defined as drugs that have the ability to immobilize or kill the sperm upon contact. An ideal spermicide should immediately and irreversibly produce immobilization of the sperm, be nonirritating to the vaginal and penile mucosa, not have adverse effects on the developing fetus, be free from long term topical and systemic toxicity, and should not be systemically absorbed. Hence, the spermicidal agents under development should be critically evaluated on these aspects.
Spermicides can be broadly classified into the following major divisions based on their origin:
Natural spermicides
This class includes all the spermicidal agents derived from natural sources like plants, microbes and animals. The isolated and identified compounds as well as extracts with established specific spermicidal properties are discussed below. Medicinal plants have been screened for decades in search of spermicidal compound/s. The compounds responsible for the spermicidal activity may act singly or through a synergistic action.
Gossypol: A di-sesquiterpene aldehyde, isolated from the seeds of cotton (Gossypium species) plant, is reported to be a spermicidal agent [12]. The MEC (minimum effective concentration) is estimated to be 40 mg/mL [13]. Gossypol (Figure 1) inhibits sperm motility by blocking ATP production and utilization. It acts on mitochondria, suppressing oxygen consumption, inhibiting the pyruvate dehydrogenase and ATPase activities, and probably acts on the motility apparatus both by blocking dynein ATPase activity and preventing protein phosphorylation [14].
Hederagenin derivatives: Saponins isolated from Sapindus mukorosii (reetha) have shown most potent spermicidal activity. The saponins reported are derivatives of hederagenin (Figure 2) namely mukurozi-saponins E1, G, X, Y1, Y2, Z1 and Z2 [15]. After incubation with saponins at 0.5 mg/mL for 1 min, the spermatozoa did not exhibit any significant morphological changes, though at the same concentration, immobilization of the sperms was observed. At higher concentrations of saponins (1-50 mg/mL) spermatozoa displayed marked disruption, vacuolation, vesiculation and erosion of the membrane covering the head region. Coiling of the tail was also noticeable with higher concentrations of saponins though no damage was evident under SEM in the flagellar region of the sperm [16,17]. These saponins were formulated into a contraceptive cream named ‘CONSAP’. This cream has completed Phase III clinical trials successfully in India [18].
Allitridium: Allitridium (Figure 3) isolated from garlic (Allium sativum) showed complete immobilization of sperms from human and animals within 20 sec at 7.5 mg/mL and within 3 min at 1.5 mg/mL. At the dose of 7.5 mg/mL, it showed no vaginal irritation reaction or other side effects. It had no bacteriostatic action on the lactic acid bacilli, so is unlikely to interfere with the growth of the bacilli in the vagina [19].
Acaciasides A and B: Mixtures of two difficult to separate triterpenoid saponins isolated from the powdered seeds of Acacia auriculiformis have shown spermicidal activity at the concentration of 0.35 mg/mL. The aglycone parts of these two saponins were characterized as acacic acid lactone and the monosaccharide constituents were identified as D-glucose, D-xylose, L-arabinose, and L-rhamnose. The complete chemical structures of these compounds are given in the Figure 4. Regarding their mode of action, electron microscopic observation showed that the plasma membrane was disintegrated and total dissolution of the acrosomal cap took place [20,21].
Mollugogenol A: The ethyl acetate fraction of Mollugo pentaphylla, a tropical herb, contains an antifungal triterpenoid saponin mollugogenol-A (Figure 5) which has demonstrated spermicidal activity at 300 μg/mL. Electronic microscopic observation showed that fragmentation or loss of plasma membrane, vesiculation of periacrosomal membrane and dissolution of the organelle took place, suggestive of sperm degeneration [22].
Salannin: A limonoid bitter principle of the seed oil of Azadirachta indica, it (Figure 6) showed antiulcer, antibacterial and spermicidal activities [23].
Curcumin: Curcumin (diferuloyl methane), a yellow pigment present in the rhizomes of turmeric (Curcuma longa) and related species used as spice, has a wide array of pharmacological and biological activities. Studies have demonstrated that curcumin (Figure 7) has anti-tumor, anti-inflammatory and anti-infective activities. It also inhibits the integrase activity of the HIV. When curcumin is used in the concentrations of 30 μg/mL and 100 μg/mL, the human sperm motility was reduced to 53.4% and 4.1% after 120 min. Full immobilization was achieved with a dose of 300 μg/mL at the end of 60 min. Curcumininduced change in sperm mitochondrial transmembrane potential indicate that this compound may interfere with sperm energy metabolism. Used in micro molar concentrations, it inhibits protein kinase C, which is present in human sperm and is believed to play a role in modulating human sperm flagellar movement [24].
14-Deoxy andrographolide: Andrographis paniculata is a small herb abundantly available in South East Asia particularly in Indian sub-continent and China, and is one of the commercially exploited traditional medicinal plants used for various ailments. 14-Deoxy Andrographolide (Figure 8), a labdane diterpene isolated from this plant, has been found to possess significant spermicidal potential [25]. The MEC of 14-deoxyandrographolide was found to be 200 μg/ml which was lower than standard spermicide N-9.
Mi-Saponin A: The seed extracts of Madhuca latifolia were reported to have spermicidal activity. Mi-saponin A (MSA) was found to be the most potent component among a mixture of saponins (Figure 9). The mean effective concentration of MSA that induced irreversible immobilization was 320 mg/mL for rat and 500 mg/mL for human sperm. The spermicidal effect involved increased membrane LPO leading to structural and functional disintegration of sperm plasma membrane and acrosomal vesicle. A comparative in vitro cytotoxicity study in human vaginal keratocyte (Vk2/E6E7) and endocervical (End/ E6E7) cell lines demonstrated that the 50% cell cytotoxicity (CC50) values, and consequently the safety indices, for MSA were ≥8-fold higher as compared to those of N-9 [26].
Oleanolic acid 3-β-D-glucuronide: Oleanolic acid 3-β-Dglucuronide (OAG) is an active principle isolated from root extracts of Sesbania sesban has been evaluated for its spermicidal activity by [27] and the spermicidal MEC was found to be 50 μg/mL. TEM and LPO revealed that OAG affected the sperm membrane integrity. OAG (Figure 10) declined fertility to zero, was nonmutagenic and was not harmful to Lactobacillus.
Asiatic acid: Asiatic acid (Figure 11) isolated from Shorea robusta, abundantly available in the forests of Southeast Asian countries and cultivated for its strong timber throughout the Indian subcontinent, possesses appreciable spermicidal and microbicidal potential [28].
Desgalactotigonin (DGT): Crude decoction of Chenopodium album seed showed spermicidal effect at MIC 2 mg/ml in earlier studies. Systematic isolation, characterization and evaluation revealed that the major metabolite Desgalactotigonin (DGT) (Figure 12) is the most effective principle in both in vitro and in vivo studies. The minimum effective concentration (MEC) of DGT that induced instantaneous immobilization in vitro was 24.18 mM for rat and 58.03 mM for human spermatozoa. Implantation was prevented in DGT treated uterine horn while no hindrance occurred in the untreated contra lateral side. Desgalactotigonin emerged 80 and 26104 times more potent than the decoction and Nonoxynol-9 respectively. It possesses mechanism based detrimental action on both human and rat spermatozoa and spares lactobacilli and HeLa cells at MEC which proves its potential as a superior ingredient for the formulation of a contraceptive safer/ compatible to vaginal microflora [29].
Plant extracts containing principles with spermicidal activities
Chenopodium album: Aqueous decoction of seeds of Chenopodium album, a small herb that grows all over India as a common agricultural weed, has been found to possess contraceptive efficacy in laboratory mammals [30]. The Chenopodium album decoction (CAD) was found to be an intimate mixture of two glycosides. Further studies indicated that both glycosides have the common genin, oleanolic acid, but differ in the interglycosidic linkage/aglycon–sugar linkage. The complete chemical structure (sugar-sugar and sugar-aglycon linkage) of the glycosides is yet to be established. The MEC for 100% immobilization of sperm was found to be 2 mg/mL. Sperm death mediated by CA extract was found to be due to oxidative damage of cellular macromolecules by in situ generation of ROS (reactive oxygen species) [31]. The safety standard evaluation for CA extract strengthens the candidature of CAD as a safe microbicidal spermicide. It is almost non-irritant to rabbit skin and rat vaginal tissues at doses 10 fold higher than its hemolytic index. However, CAD did not block the growth of Lactobacillus, although the size of individual colony was marginally reduced. It prevented the growth of the fungal pathogen Candida albicans at 20 mg/ml of CAD. [32]
Other plants: Other plants containing saponins, which have shown spermicidal activity, include Phytolacca dodecandra, Calendula officinalis, Acacia cassia, Acacia concinna, Trigonella foenum-graecum [33], and Cestrum parqui [34]. Saponins are naturally occurring and there is no report of their systemic toxicity. However, due to their capacity to reduce interfacial tension, they may alter the permeability of the vaginal membrane on frequent use. In addition, reduction in interfacial tension may, in fact, lead to decreased viscosity of the mucus and hence result in an increased rate of transfer of spermatozoa through the vaginal mucosa. Therefore, it is necessary to critically evaluate these effects before advocating the use of saponins as spermicidal agents [35].
Neem extracts: The neem tree, Azadirachta indica, is indigenous to the Indian subcontinent. Neem oil, oil extracted from the seeds of the neem tree, has been found to possess strong spermicidal activity. By the process of hydrodistillation, the volatile fraction of neem oil has been isolated and coded as NIM-76. A concentration of 25 mg/ mL of the compound was found to achieve total spermicidal effect in 20 sec. Vaginal irritation study conducted in rabbits, by intravaginal application of 15 mg of NIM-76 in 2 mL of gelatin jelly for 10 days, showed no irritation to the vaginal mucosa [36]. Khillare has revealed that the aqueous extract of old and tender neem leaves is a potent spermicide. The minimum effective concentration required to kill 1 million sperm in 20 sec was 2.91 mg and 2.75 mg for tender and old leaf extract, respectively (Table 1) [37].
| Sr. no | Name of the plant | Parts used | Types of plants extract/active principle | Animal model | Activities | Ref. |
|---|---|---|---|---|---|---|
| 1 | Acacia concinna DC | Stem bark | Acacic acid | Rat | Spermicidal and semen coagulation activities | 43 |
| 2 | Acacia auriculaeformis A. Cunn. | Triterpenesaponins | Sperm immobilizing effect | 20 | ||
| 3 | Acacia cassia Wight &Arn. | Fruit | Saponins | Sperm immobilizing effect | 44 | |
| 4 | Achyranthesaspera Linn. | Root | 50% ethanol extract | Rat | Spermicidal action | 45 |
| 5 | Albiziaprocera (Roxb.) Benth | Seed, root | Proceric acid and leanic acid | Rat | Spermicidal and semen coagulation activities | 43 |
| 6 | Anagallisarvensis Linn | Whole plant | Rat | Spermicidal and semen coagulation activities | 43 | |
| 7 | AzadirachtaindicaA.Juss | Seed | Seed oil | Rat | Spermicidal activity | 46 |
| Neem oil | Monkey, Human | Spermicidal activity | 47 | |||
| Leaves | Aqueous extract | Rat | Spermicidal activity | 37 | ||
| 8 | BurseraSp | Stem, leaf | Saponins, leaf extract | Human, Bovine | Sperm aggregation | 48 |
| 9 | Carica papaya Linn | Seed | chromatographic sub fraction of chloroform extract | Human | Spermicidal activity | 49 |
| 10 | CitrulluscolocynthisSchrad | Fruit | 50% ethanol extract | Rat | Impairment of sperm | 50 |
| 11 | Cyclamen persicum Mill. | Whole plant | Saponins | Spermicidal activity | 51 | |
| 12 | Diploclisiaeshinatus Linn. | Stem | Ecdysterone | Spermicidal activity | 52 | |
| 13 | EshinopseshinatusRoxb | Root | 50% ethanol extract | Rat | Sperm antimotility. reduces sperm density in cauda epididymis | 53-54 |
| 14 | EmbeliaribesBurm.f. | Berry | Embelin | Rat | Spermicidal activity | 55 |
| 15 | Eupatorium brevipes DC. | Brevipenin | Spermicidal activity | 56 | ||
| 16 | HederanepalensisK.Koch | Inflorescence | Immobilization of spermatozoa | 57 | ||
| 17 | Justicia simplexD.Don | Flower | Justicisasaponin | Sperm acrosomal membrane stabilizing action | 58 | |
| 18 | Melodinusfusiformis Champ. Ex Benth. | Solasodine (steroidal alkaloid ) |
Spermicidal activity | 59 | ||
| 19 | Ophiopogonintermedius (D,Don) Maxim | Rhizome | n-octacosanal, β-sitosterol | Spermicidal activity | 60 | |
| 20 | Pittosporumneelgherrense Wight &Arn | Plant without root | Pittosida-A and Pittosida-B | Spermicidal and semen coagulation activities | 61 | |
| 21 | Primula vulgarisHuds. | Saponins | Immobilization of spermatozoa | 62 | ||
| 22 | PyruscuspidataBetrol. | Plant without root | Extract | Spermicidal and semen coagulation activity | 43 | |
| 23 | Annonasquamosa | Seeds | Hydroalcoholic extract | human | Spermicidal activity | 63 |
Table 1: Summery of extracts of different medicinal plants with spermicidal activity (1980-2005).
Praneem polyherbal formulations: A combination formulation developed as “Praneem polyherbal cream”, which includes a purified extract from the dried seeds of Azadirachta indica (250 mg/mL), extract from the pericarp of fruits of Sapindus mukorosii (0.5 mg/mL) and quinine hydrochloride (3.46 mg/mL), has shown spermicidal activity in 20 sec. The formulation has shown high contraceptive efficacy in rabbits and in monkeys after intravaginal application. Also the formulation was found to be safe with no vaginal irritation when applied intravaginally for 30 days at a daily dose of 1 mL [38]. The Praneem polyherbal pessary and tablet formulated includes purified ingredients from neem leaves, Sapindus mukorosii and Mentha citrata oil. The vaginal pessary has shown potent spermicidal action of human spermatozoa in vitro and high contraceptive efficacy was demonstrated in rabbits of proven fertility [39,40]. Praneem polyherbal formulations have shown in vitro activity against HIV and sexually transmitted disease pathogens [40]. Praneem vaginal pessaries and tablets were found to be safe for once daily intravaginal use consecutively for 7 and 14 days in healthy women volunteers [41,42]
Spermicides from natural sources other than plants
Dermaseptins and magainins: These are two classes of cationic, amphipathic α-helical peptides that have been identified in the skin extracts of frogs and Xenopus laevis [64]. Magainins A and G, which are two natural peptides having 23 amino acids and differ by only two substitutions, have been found to have a wide spectrum in vitro antimicrobial activity against gram positive and negative bacteria, fungi, and protozoa. Considering their contraceptive activities and their effect against various STI-causing pathogens, it is believed that these two peptides are appropriate candidates for the evaluation of newer and safer microbicides spermicides in the future [65]. Magainin-A was found to be more potent than magainin-G. Intravaginal administration of magainin-A 200 μg to rats [66] and 1 mg to rabbits and monkeys once before mating resulted in 100% sperm immobilization [67,68]. Magainin-A does not have overt cytotoxic properties and is safe for intravaginal application. It is also active against various STI-causing pathogens but not against HIV-1 and HIV-2. It is reported that effectiveness of magainin as a contraceptive in vivo is possibly due in part to the removal of cholesterol from sperm membranes [69].
Microorganisms: Microorganisms are also known to inhibit sperm motility either directly by agglutinating the spermatozoa or excreting extracellular products that immobilize the sperms.
Nisin: It is a 34 amino acid, naturally occurring antimicrobial cationic peptide known to be produced by the bacteria Lactococcus lactis. Nisin has been used as a food preservative throughout the world and the World Health Organization (WHO) and US, Food & Drug Administration have conferred GRAS status to this peptide. At the dose of 300-400 μg, complete immobilization of human spermatozoa was observed within 20 sec. In vivo contraceptive efficacy studies in rats showed complete arrest of sperm motility and no pregnancy in any of the animals. At the contraceptive dose of 200 μg, Nisin did not alter the morphology of the vaginal epithelial cells, nor did it cause any histopathological lesions in the vaginal epithelium when administered intravaginally for 14 consecutive days. The mechanism by which Nisin exerts its rapid spermicidal action is not known. However, the existing evidence suggests that it possesses an overall positive charge and interacts preferentially with anionic phospholipids. The sperm plasma membrane contains high concentration of phosphatidylglycerol, a strong anionic phospholipid moiety, and thus Nisin may have high affinity towards spermatozoa [70].
Sophorolipids: Sophorolipids (SLs) are a group of microbial glycolipids produced by yeasts, such as Candida bombicola, Yarrowia lipolytica, Candida apicola, and Candida bogoriensis [71]. Various forms of sphorolipids produced by Candida bombicola showed spermicidal and virucidal activities. They occur naturally as the disaccharide sophorose linked glycosidically to the hydroxyl group at the penultimate carbon of primarily C18-chain-length fatty acids [72]. The sophorolipid diacetate ethyl ester derivative (Figure 13A) is the most potent spermicidal and virucidal agent of the series of SLs studied. Its virucidal activity against HIV and sperm-immobilizing activity against human semen are similar to those of nonoxynol-9. However, it also induced enough vaginal cell toxicity to raise concerns about its applicability for long-term microbicidal contraception. Its structureactivity relationship has been established for creating new analogs with less cytotoxicity and higher activity.
sophorolipid analogues prepared by amino acids conjugated by forming amide bonds between their R-amino moiety and the carboxyl group of ring-opened SL fatty acids (Figure 13B) resulted in a new series with improved activities.
The influence of different uropathogenic microorganisms such as Escherichia coli, Enterococcus, Pseudomonas aeruginosa, Staphylococcus saprophyticus, Candida albicans on human sperm motility has been studied in vitro by Huwe et al. [74]. Yin et al. showed that at high concentrations, Streptococcus viridians could induce sperm agglutination in vitro [75]. Jiang and Lu reported that Staphylococcus aureus significantly immobilizes the spermatozoa [76].
In 2005 Ohri et al. was successful in isolating of spermatozoal agglutinating factor was isolated from Staphylococcus aureus isolated from a woman suffering from unexplained infertility [77]. The contraceptive efficacy of SAF was further evaluated using mouse as an in vivo model by the same group. The results indicated that 2.5 micrograms of SAF was sufficient to arrest sperm motility and protect against pregnancy [78].
Synthetic spermicides
These include the synthetically derived compounds which have been proved to possess spermicidal properties. In several of the cases significant anti-microbial activities are also found and the products can be categorized as dual action spermicidal microbicide. The different classes of synthetic compounds which have shown spermicidal effects and are being used as spermicides or may be used in future are discussed below.
Non-ionic surfactants: In the category of non-ionic surfactants octoxynol and nonoxynol are the two commonly reported surfactants. Nonoxynol is more potent spermicide than octoxynol. Among the different nonoxynol derivatives designated as N1-N15, p-nonyl phenoxy polyethoxy ethanol (N-9) is reported to be the most potent spermicide [79]. At present N-9 (Figure 14) is the only marketed contact spermicide available worldwide as gel, cream, foam and pessary formulations in various strengths. At the dose of 500 μg/ mL N-9 completely abolishes all sperm movement within one minute of addition. Although, N-9 has been employed as a contact spermicide for the last 30 years and is well tolerated, reports have appeared suggesting that the frequent use of surface active spermicides can be associated with vaginal irritation and the appearance of lesions in the epithelium. It has also been shown that nonoxynol-9 kills the natural vaginal flora (Lactobacillus) [80-83] causing disturbance of the normal (acidic) vaginal pH and weakening the natural protection against STIs, reproductive-tract infection (RTIs) and urinary-tract infections (UTIs) [84].
More recent studies report that the use of N-9 as a microbicide or in limiting the transmission of STD’s should be discontinued since it interferes with the lipid bilayer of the vaginal epithelium and facilitates the process of absorption and transmission of the viral particle into the blood stream [85-88].
Ahmad et al. have designed a new bioadhesive suppository of N-9 called Long Acting, Sustained Release Spermicide (LASRS) that possesses advantages over the presently marketed formulations by having long-term efficacy and by forming a bioadhesive, protective layer over the genital tract epithelium [89,90].
Zidovudine derivatives: Zidovudine, i.e. 3’-azido-3’- deoxythymidine lacks in having spermicidal activity by itself, but two of its novel phenyl phosphate derivatives WHI-05 [5-bromo- 6-methoxy-5,6-dihydro-3’-azidothymidine-5’-(p-methoxy-phenyl) methoxyalaninyl phosphate] (Figure 15A) and WHI-07 [5-bromo- 6-methoxy-5,6-dihydro-3’-azidothymidine-5’-(p-bromophenyl) methoxyalaninyl phosphate] (Figure 15B) have been identified to exhibit potent anti-HIV and spermicidal activity [91,92]. They are dualfunctional microbicides lacking detergent-type membrane toxicity, which would have advantages over the currently available vaginal microbicides. Unlike, N-9, the spermicidal activity of WHI-05 and WHI-07 in mice and rabbits indicated these are non-cytotoxic and lack of inflammation-inducing properties [93,94].
D’Cruz et al. also demonstrated that an intravaginal application of 2% WHI-07 via a gel microemulsion in rabbit model resulted in marked contraceptive activity [95].
Vanadocenes: Spermicidal organometallic complexes of vanadium (IV) with bis(cyclopentadienyl) rings, called vanadocenes are a new class of experimental contraceptive agents. These are reported to have rapid, potent and selective sperm immobilizing activity (SIA) at nanomolar to micromolar concentrations. The SIA of representative vanadocenes was 400-fold more potent than that of N-9. Vanadocene dihalides immobilized human sperm in semen within 15 sec without affecting the sperm membrane integrity or viability of normal human vaginal or cervical epithelial cells. These features of vanadocenes fundamentally differ from those of currently used membraneactive detergent-type spermicides that are cytotoxic to genital tract epithelial cells at spermicidal concentration. The lack of detergent-type membrane toxicity of spermicidal vanadocenes suggests that they may have particular clinical utility as a new class of contraceptive agents. Spermicidal activity of vanadocenes were shown to be mediated by a unique mechanism involving membrane intercalation that was independent of dynein adenosine triphosphatase activity, protein tyrosine phosphatase activity, and the phosphocreatine/creatine kinase system. Among the 45 vanadocenes that were synthesized and evaluated for human spermicidal activity vanadocene acetylacetonato monotriflate (VDACAC) (Figure 16A) and vanadocene dithiocarbamate (VDDTC) (Figure 16B) were the most stable and potent spermicidal vanadocenes [96-103].
Repeated intravaginal application of gel formulations of VDACAC and VDDTC did not induce local inflammation, toxicity or retention of vanadium in the mice and rabbit vaginal irritation model. D’Cruz et al. demonstrated that the intravaginal application of a 0.1% VDDTC in rabbits and pigs results in remarkable contraceptive activity [104-107].
Carbodithionate and carbamodithionate derivatives: These constitute a dually active, nonsurfactant series of molecules (15 compounds) that are capable of killing Trichomonas vaginalis (both metronidazole-susceptible and -resistant strains). All of the novel compounds were found to be much safer than N-9 towards Human Cervical Epithelial Cells (HeLa) and vaginal microflora (lactobacillus). The most promising candidate, however, was the compound pyrrolidinium pyrrolidine-1-carbodithionate (Figure 17) which killed sperm and trichomonas at concentrations that were about 15 and 450 times lower than its IC50 against lactobacillus. The study clearly indicates a highly specific action and a much better safety index for the new compound compared to N-9 and warrants further investigation for the development of a safe microbicidal contraceptive [108]. These constitute a dually active, nonsurfactant series of molecules (15 compounds) that are capable of killing Trichomonas vaginalis (both metronidazole-susceptible and -resistant strains). All of the novel compounds were found to be much safer than N-9 towards Human Cervical Epithelial Cells (HeLa) and vaginal microflora (lactobacillus). The most promising candidate, however, was the compound pyrrolidinium pyrrolidine-1-carbodithionate (Figure 17) which killed sperm and trichomonas at concentrations that were about 15 and 450 times lower than its IC50 against lactobacillus. The study clearly indicates a highly specific action and a much better safety index for the new compound compared to N-9 and warrants further investigation for the development of a safe microbicidal contraceptive [108].
C31G: C31G is spermicidal formulation composed of an equimolar mixture of n-dodecyl-dimethylamine-N-oxide (C12-NMe2-O) and N-(n-dodecyl)-N-dimethyl-glycine (C12-betaine) with microbicidal/ virucidal properties. C31G has shown in vitro activity against a large number of gram-negative, gram-positive bacterial strains as well as few fungal strains. It is a potent virucidal agent with activity against HIV and herpes simplex virus [109]. A phase I double-blind randomized study of 1.2% C31G with hydroxyl ethyl cellulose (HEC) suggested that physical epithelial changes after seven consecutive days of product use were similar to changes seen with a marketed 2% nonoxynol-9 product (Gynol-II). The subjective symptoms of genital burning or heat, however, were much greater with the C31G HEC product, which limits its usefulness [110].
Disulphide esters of carbothioic acid: DSE-36 and DSE-37 synthesized by Jain et al. killed sperm 25 times more strongly and with a more precisely targeted action than nonoxynol-9 (N-9). The effects of DSE-36 (Figure 18A) and DSE-37 (Figure 18B) on human spermatozoa versus HeLa cells were examined to establish specificity and safety compared with N-9 [111-113].
Indole derivatives: 3,3-Diheteroaromatic oxindole derivatives (Figure 19) prepared by coupling indole-2,3-dione (isatin) with differently substituted indoles and pyrrole in presence of I2 in i-PrOH were evaluated for in vitro spermicidal potentials and the mode of spermicidal action of the synthesized analogues were evaluated. The derivative 3, 3-bis (5-methoxy-1H-indol-3-yl) indolin-2-one (3d) exhibited the most significant activity [114].
Carbaldehydes: Substituted isoxazolecarbaldehydes (Figure 20) were synthesized by Gupta et al. and established as a new class of compounds exhibiting both spermicidal and acrosin inhibitory activities simultaneously. The authors have indicated that 5- and 3-substituted isoxazole carbaldehydes are ‘first generation’ multifunctional, spermicidal molecules that hold promise for development as topical contraceptives with useful associated activities that can add considerably to their effectiveness, safety and prophylaxis [115].
Quinoline derivatives: A series of twenty two derivatives of 3-(1-alkyl/aminoalkyl-3-vinyl-piperidin-4-yl)-1-(quinolin-4-yl)- propan-1-one and their 2-methylene derivatives were synthesized from naturally abundant cinchonine. Tartarate salts of these compounds were prepared and evaluated for spermicidal activity. The most active compounds (Figure 21A-E) showing potent spermicidal activity were further evaluated against different strains of Trichomonas vaginalis for antimicrobial activity, in HeLa cell lines for cytotoxicity, and against Lactobacillus jensenii for eco-safety. The tartarate of 3-(1-pentyl-3- vinyl-piperidin-4-yl)-1-(quinolin-4-yl)-propan-1-one) was found to be more active than N-9 in spermicidal activity [116].
7-Membered oxazaquinolinium salts: Fused tricyclic oxazaquinolinium salts (Figure 22) were synthesized using Amberlite IRA 402(OH) in water and assessed for their sperm-immobilizing efficacy by various in vitro assays. Out of eleven derivatives three showed potent spermicidal effect. Antimicrobial efficacies of the potent derivatives, assessed by disc diffusion as well as by agar and broth dilution methods using human isolates of bacteria and fungi, revealed their moderate antimicrobial potential. The compounds, found to be nontoxic to rabbit erythrocytes by hemolytic assay, may be exploited as microbicidal spermicides [117].
Furo[3,2-h]quinolinium salts: 7-Aryl substituted furo[3,2-h] quinoliniums, which are the hybrids of quaternary pyridinium salts and benzo[b]furans, were synthesized in two steps from 5-chloro-8-hydroxy-7-iodo-quinoline and aryl acetylenes through a tandem Sonogashira alkynylation-cyclization pathway followed by quaternisation using methyl iodide/2-bromo acetophenone under MW irradiation using basic alumina. The spermicidal potentials of furo[3,2-h]quinoliniums 5d and 5e (Figure 23) are at least four to five times higher than the standard spermicide N-9, which signifies their possibility of being used as an alternative to N-9. The compounds destroyed the functional and structural integrity of the sperm plasma membrane with no impact on Lactobacillus sp. though these were toxic to common vaginal pathogens. Hence it is believed that these dually active molecules will find application in future formulations for microbicidal contraceptive preparations replacing nonoxynol-9 (N-9) [118].
Parabens: Parabens are a class of chemicals widely used as preservatives by cosmetic and pharmaceutical industries. These are effective preservatives in many types of formulations. These compounds and their salts are used primarily for their bactericidal and fungicidal properties. Methyl, ethyl, propyl and butyl paraben (Figure 24A-D) have shown potent spermicidal activity at the concentrations of 6, 8, 3, and 1 mg/mL respectively [119].
Gel microemulsions: In 2001, in a systematic effort to develop a dual-function intravaginal spermicide as well as a drug delivery vehicle against sexually transmitted pathogens, D’Cruz et al. formulated novel submicron (30-80 nm) particle, lipophilic and spermicidal gel-microemulsion (GM) formulations GM-144 and GM-4. Microemulsions are thermodynamically stable and isotropically clear dispersions of water, oil, and surfactants with potential as drug-delivery vehicles. GM-144 prepared from seven nontoxic pharmaceutical excipients (propylene glycol, Captex 300, Cremophor EL, Phospholipon 90G, Rhodigel, Pluronic F-68 and sodium benzoate) was found to show rapid sperm-immobilizing activity in human semen in less than 30 sec. GM-4 formulation containing eight pharmaceutical excipients (Captex 300, Cremophor EL, Phospholipon 90G, Propylene glycol, PEG-200, seaspan carrageenan, viscarin carrageenan and sodium benzoate) exhibited potent spermicidal activity in less than 2 min. When tested as vaginal contraceptives in standard rabbit model, GM-144 proved as effective as the commercially available N-9 formulation (Gynol II) and GM-4 was far more effective than Gynol-II. No toxic effect was observed on the vaginal mucosa of rabbits after daily exposure for 10 days [120-123].
Miscellaneous agents: New indolyl phthalazinones and phthalazine derivatives showed marked spermicidal activity, which was ten times that of N-9 [124]. 1, 4-Naphthaquinone was capable of generating reactive oxygen species (ROS) and showed spermicidal and antimicrobial activities [125]. Promethazine hydrochloride (Figure 25) showed spermicidal activity at 0.4 mg/mL concentration, and is more effective than propranolol on human sperm [126].
Dihydro alkoxy benzyl oxopyrimidine (DABO) derivatives (Figure 26) exhibited spermicidal activity as well as antiviral activity [127].
A new delivery system (ACIDFORM) was designed with acidbuffering, bioadhesive and viscosity-retaining properties to maintain the acidic vaginal milieu (the low pH inactivates many pathogens and spermatozoa), form a protective layer over the vaginal/cervical epithelium (minimizing contact with pathogenic organisms), and provide long-term vaginal retention [128]. A Phase I clinical study with ACIDFORM provided initial information about its safety and showed the formation of a layer over the vaginal/cervical epithelium [129].
The Na+-Ca2+ exchanger and Ca2+-ATPase pumps reported to be present on the sperm membrane are responsible for maintaining the intracellular Ca2+ concentration that is involved in regulation of sperm function. 2’,4’-Dichlorobenzamil hydrochloride, (Figure 27) a Na+-Ca2+ exchange inhibitor, showed spermicidal activity [130].
Octyl-D-glucopyranoside (OGP) can immobilize and kill the sperms depending on concentration. Osmond et al. concluded that the phenyl-substituted and cyclohexenyl-substituted thiourea derivatives (Figure 28) can act as potent anti-HIV agents with sperm immobilizing activity and reduced cytotoxicity when compared with N-9, and have the clinical potential to become the active ingredients of a vaginal contraceptive for women who are at high risk for acquiring HIV by heterosexual vaginal transmission [131].
Hexahydro indenopyridines (Figure 29) were synthesized as spermicides and antifungals [132]. Acylcarnitine analogues, (+)-6-carboxylatomethyl-2-alkyl-4, 4-dimethylmorpholiniums (Figure 30) show in vitro activities as spermicides, anti-HIV agents and inhibitors of the growth of Candida albicans. Activity improves with increasing chain length [133]. Maleimide derivatives (Figure 31) have been evaluated as spermicidal agents by inhibiting sperm motility [134].
Selective serotonin reuptake inhibitors (SSRI): Fluoxetine (Figure 32A) and paroxetine (Figure 31B) which are antidepressants binding with neuronal 5-HT transporter through sulfhydryl group, have been recently reported as non-detergent spermicides. Other SSRIs such as fluvoxamine maleate, citalopram hydrobromide, and sertraline hydrochloride also show non-detergent spermicidal activities [135].
Major Possible Pathways by Which the Spermicides Work
Change in calcium balance
The fertilization process consists of an acrosomal reaction and sperm-egg fusion, which require extracellular calcium [136-138]. This external triggering mechanism is regulated by a modification of the calcium balance, which is gated by Ca2+channels, and accompanied by a shift in intracellular pH [139]. Ca2+ and pH may in turn control the phosphorylation state of functional proteins in the flagellar axoneme activated directly through cAMP and cAMP-dependent kinase [140,141]. Therefore, each step in the calcium-mediated regulatory process could serve as a potential target site for spermicidal action [142]. To interrupt these steps using inhibitors or blocking agents could provide insight into the mechanisms of spermicidal action. For this purpose, we noted the application of chelates like ethylene diamine tetra acetic acid (EDTA), ethylene bis(oxyethylenenitrilo) tetra acetic acid, and gramicidin. They were found to exert spermicidal action against human sperm at the tested concentration range, impeding sperm penetration to the extended cervical space. Kumar et al [143] have studied the activities of sulfonylureas such as Glibenclamide and gliclazide as well as meglitinide analogues such as ripaglinide which produces a dose and time dependent decrease in viability. The reduction in sperm viability was accompanied by an elevation of Ca2+ is and was affected by removal of extracellular Ca2+. Studies conducted by Gulati et al. [144] with Miconazole nitrate, clotrimazole and loperamide hydrochloride furnished similar results where enhanced spermicidal activity of miconazole, clotrimazole and loperamide appeared to be due to further mobilization of Ca2+ from partially depleted intrasperm Ca2+ stores. Synergism of spermicidal activity and intrasperm Ca2+ elevation by miconazole or clotrimazole was observed when Ca2+ efflux from spermcells was simultaneously inhibited by 20,40-dichlorobenzamil hydrochloride, a Na+–Ca2+ exchange inhibitor. Gupta et al. [145] also studied the Influence of commonly used H2 receptor antagonists cimetidine, ranitidine and famotidine on sperm viability and intrasperm Ca2+ was evaluated in ejaculated human semen samples. All these drugs were found to reduce sperm viability in a dose- and time-dependent manner. This action was accompanied with elevation of intrasperm Ca2+. 2’, 4’-dichlorobenzamil hydrochloride (DBZ), a Na+–Ca2+ exchange inhibitor, that is known to elevate intrasperm Ca2+, potentiated the spermicidal action of H2-receptor antagonists.
Change in pH level:
The spermatozoa are motile between pH 6.7 to 8.5. The normal vaginal flora of healthy women of childbearing age is dominated by lactobacilli. Lactobacillus produces a number of compounds including lactic acid, hydrogen peroxide, lactacin, and acidolin that maintain a low, acidic pH (3.5–5.0) [146] and thereby protect against the pathogens that cause STIs including HIV [147,148]. When semen enters the vagina, the pH rises to above 6.0 because of the buffering activity of the ejaculate (pH 7.2-8.0) [149]. It is well documented that sperm are sensitive to low pH and acidic solution can immobilize sperm within minutes [150]. This explains the use of lemon juice in ancient times as spermicide, as well as of modern formulations like “ACIDFORM” [128,129].
Sulfhydryl binding agents
Proteins present in the plasma membrane, head and tail region are rich in disulfide linkages. The dynamic conversion of thiols to disulfide linkages forms an essential part of sperm maturation. Sulfhydryl binding agents exert their action by oxidation, alkylation or formation of mercaptides. Hydrogen peroxide, o-iodobenzoate and several hydroquinones are known to destroy the tertiary protein structure by converting the thiol group of cysteine to disulphide linkages. Phenyl mercuric acid is another mercaptide forming agent. Maleimide derivatives have also been evaluated as spermicidal agents by inhibiting sperm motility through sulfhydryl binding. [138].
Surfactants
Surfactants by definition are compounds that lower the surface tension (or interfacial tension) between two liquids or between a liquid and a solid. A common lipid bilayer, which contains external, internal and transmembrane proteins, is fundamental feature of the plasma membrane of the sperm. Natural or synthetic surface agents interact with this lipid bilayer, affect the glycoproteins of the cellular membrane, and modify the ionic transport across the membrane, leading to surface changes. These changes, namely vesiculation, vacuolation or dissolution of head region may occur due to stretching, loosening, or breakdown of the membrane and ultimate removal of the acrosome [16]. Saponins are the natural surface active agents widely occurring in many plants and are reported to have profuse spermicidal action as has been discussed earlier. Among the synthetic detergent type spermicides, Nonoxynol-9 is the most common and is present in many marketed formulations. Nandi et al suggested that the double bonds present in nonionic surfactants form allelic radicals that may react with the molecular oxygen present in the membrane and cause LPO [151].
Acrosin inhibition
Acrosin is the major proteinase present in the acrosome of mature spermatozoa. It is a typical serine proteinase with trypsinlike specificity. The active enzyme functions to cause lysis of the zona pellucida, thus facilitating penetration of the sperm through the innermost glycoprotein layers of the ovum. So inhibition of acrosin is one of the pathways by which certain spermicides work. Substituted isoxazole carbaldehydes, for example, act as spermicides by acrosin inhibition [115]
Membrane disruption
Comparable to the effect of typical detergent type spermicides, certain synthetic molecules caused distinct eruptions on the sperm surface in the form of blebbing, vesiculation or exfoliation that occur throughout the body of the spermatozoa or are confined to the acrosomal region. But these molecules being non-detergent in nature are non-irritant to the vaginal epithelium and hence hold promise for being better candidate as vaginal spermicide [28,117,118].
Lipid peroxidation
Mammalian sperm membrane comprises of high amounts of polyunsaturated fatty acids, plasmalogens, and sphingomyelins that render it highly susceptible to damage by reactions with molecular oxygen. ROS produced under normal conditions are efficiently scavenged by antioxidant enzymes such as SOD. However when ROS levels exceed the antioxidant capacity of sperm cells, it becomes detrimental. Many spermicidal and spermiostatic compounds act by generating ROS in sperm cells [152-154].
Each year, of the estimated 210 million pregnancies that occur worldwide, 40% are unplanned [155]; on the other hand, more than 90% of all adolescent and adult HIV infections have resulted from heterosexual intercourse [156]. Thus, there is a growing interest in combining contraception with protection against STIs/HIV. A new generation of dual-function spermicides that offer protection against STIs (including HIV) and pregnancy and whose action is mechanismbased are urgently needed by the society [157,158]. Taking into consideration the current global need, microbicidal property of any spermicide is of prime importance, but its adverse effects on vaginal health should never be underestimated. Any spermicide should not potentially disrupt the vaginal ecology while exerting its intended action. Especially, inactivating friendly microbes like Lactobacilli can bring severe detrimental effects to the normal vaginal ecology. So, it is extremely important to identify and evaluate new contraceptive antimicrobial agents that can be used vaginally in effective doses without causing overt vaginal irritation or other toxicity. This need for the new generation dual action spermicides is also augmented by the fact that currently the use of OCPs and IUDs is becoming restricted the world over due to increased awareness of the associated side-effects. The use of vaginal contraceptives as local (topical) agents in a needbased manner (not requiring regular intake/ application) makes them relatively much safer [159]. Male condoms being the most trusted and easy method of contraception suffers the drawback of not being women controlled. Moreover microbicidal spermicide can also be used as an adjunct to condoms or in medicating condoms to increase their efficacy and safety [160].
The above facts and evidence in the foregoing literature highlight that there is a huge vacant space in the field of contraceptive research to devise newer, safer, and more convenient agents to bring down fertility while providing protection against microbial infections. Vaginal spermicides appear to be the best choice from all these considerations. An ideal preparation is required for the users, especially for the women who can use it as per their own need and convenience, and it must meet following four criteria:
• Rapid action and effective in killing all sperm on contact or rendering them incapable of fertilization,
• Systemic nontoxicity, and nonirritating nature to vaginal and penile skin and mucosa,
• No embryotoxic or fetotoxic effects, and
• Absence of long-term toxicities.
The spermicides work by blocking entry of sperm into the uterus with foam or thick cream and creating an environment in which sperm cannot survive. In surveys of spermicide users, women have been found to appreciate spermicidal products because they not only prevent conception, but improve sexual satisfaction and are convenient to use. Male users also appreciated the additional lubrication the products provide. Inadequate lubrication during sexual activity is a major factor causing rupture of condoms; vaginal spermicides that contribute to vaginal lubrication reduce risk of pregnancy and STDs; and thus the spermicides are well accepted by a section of people [161]. However, with use of spermicides according to directions and at a rational interval, vaginal spermicides will be essentially free of adverse effects. People have used them for several decades and the relative paucity of reports is a testimony to a low incidence of adverse reactions. However, there are also some reported problems that are covered in the medical literature [162].
How well spermicides prevent pregnancy is highly variable depending on whether they are used correctly and consistently. Their effectiveness also depends upon whether they are used in addition to another barrier method, such as the diaphragm, cervical cap, or condom. If used perfectly, the failure rate may be as low as 3%. However, in typical users, the failure rate can be as high as 36%. Studies have shown that when spermicides are used alone, pregnancy usually occurs in 21-26% of women during the first year of spermicide use [163]. The number of pregnancies is significantly reduced when spermicides are used with another barrier method, particularly the condom. Future research therefore needs to be directed to develop new spermicides which will be virtually free of undesirable side-effects while being effective and possess microbicidal activity to prevent STDs but be benevolent to friendly bacteria. They need to be used in conjunction with physical barrier methods to ensure higher rate of success and greater acceptance to the population at large.