International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2023)Volume 11, Issue 1
Background: The purpose of this study was to compare the return to sport outcomes at six months after ACLR between meniscus procedures, ACLR (ACLR-only), ACLR with meniscectomy (ACLR-resect), and ACLR with meniscal repair (ACLR-repair) for bone patellar tendon bone grafts and hamstring tendon grafts, separately.
Methods: This cross-sectional study included 314 participants (168 female; mean ± SD age, 19.7 ± 4.8) with ACLR with a BPTB or HT. Patients were divided into three groups depending on meniscal procedure. Multivariate analysis of covariance compared differences between meniscal procedures on the battery of tests, and for each statistically significant variable, an analysis of covariance assessed the effect of meniscal procedure within each graft type. Logistic regression assessed the influence of meniscal procedure on tests’ pass rates defined as 90% of limb symmetry index (90% LSI). Tests that were statistically significant were independently analyzed by a separate logistic regression for each graft type.
Results: BPTB: ACLR-only had greater hamstring strength than ACLR-resect (p=0.05) and ACLR-repair (p=0.005). ACLR-only was more likely to pass the hamstring strength test than ACLR-resect (OR (95% CI) (2.52 (1.32, 4.82), p=0.01) and ACLR-repair (2.29 (1.07, 4.90), p=0.01). HT: ACLR-only (p=0.03) and ACLR-resect (p=0.003) had higher IKDC scores than ACLR-repair.
Conclusion: The influence of meniscal repair on clinical outcomes is dependent on the graft choice. Rehabilitation following ACLR with BPTB and a meniscal procedure should emphasize hamstring function for optimal short-term recovery.
Anterior cruciate ligament; Bone-patellar tendon-bone graft; Meniscus injuries; Muscle strength
Anterior Cruciate Ligament (ACL) injuries commonly occur among the athletic population. ACL Reconstruction (ACLR) is the choice of treatment especially for those who intend to return to sport. In 2006, an approximated 100,000 individuals underwent ACLR in the United States [1], and the current total is certainly larger as the incidence rate increased by roughly 20% between 2002 to 2014 [2]. Rupture of the ACL often involves concomitant injuries to the meniscus, other ligaments and articular cartilage [1]. Specifically, the prevalence of meniscal involvement varies from 44-65% [2,3].
Optimal graft choice for ACL reconstruction has been a subject of debate in the literature, and it is often individualized accounting for the patient’s physical demands, patient/surgeon preferences, and desired post-operative outcomes [4]. Bone Patellar Tendon Bone (BPTB) and Hamstring Tendon (HT) grafts are traditional choices for reconstruction autografts among surgeons. Bone patellar bone is associated with decreased knee extension strength until two years post-surgery [5,6]. Similarly, HTs are known to result in decreased knee flexion strength at two years post-surgery [6]. Strength deficits in the muscle group corresponding to graft site at 6 months seem intuitive based on donor site morbidity and strengthening precautions in the early post-operative rehabilitation stage. Early ACLR strengthening is dependent on donor choice and acknowledgment of graft site morbidity and healing concerns. Hamstring graft restrictions include avoidance of resisted hamstring activities for up to 12 weeks after surgery. Similarly, early rehabilitation limitations apply to open kinetic quadriceps strengthening for bone patellar bone at increased knee flexion ranges to reduce excessive strain on the healing graft [7].
The influence of meniscus repairs and meniscectomies on clinical outcomes has been studied less. A systematic review and meta-analyses reported that isolated meniscal surgery resulted in moderate quadriceps and hamstring strength deficits [8], however quadriceps and hamstring strength had become comparable to the contralateral side at two-years post-operatively [8]. Early postoperative rehabilitation and strengthening will differ based on graft type and level of meniscal involvement [7]. If a meniscal repair is performed in conjunction with the ACL reconstruction, modification to rehabilitation often include limited weight bearing and restricted range for knee flexion for the first 6 weeks [7]. Based on location of meniscal tear and/or surgeon preference, variations exist between protocols including percentage of weight bearing, post-operative bracing, and range of motion during the early rehabilitation period following a meniscal repair [9]. Therefore significant differences in strengthening exist based on graft site and meniscal involvement in first 3 months of rehabilitation. The research is not conclusive regarding the impact of meniscal procedures on ACLR outcome at 6 months post-surgery. Given the isolated influences of meniscal procedures and graft choice on strength, clinicians may wish to consider the influence of each combination of graft type and meniscal procedure on all outcomes.
The effects of various patient-specific factors, such as age [10,11], sex [11,12], and time post-surgery [11,13], on ACLR outcomes have been described. As previously mentioned, surgery-specific factors, especially graft type and meniscal procedure, on clinical outcomes post-ACLR have been described in isolation. But, the combined influence of these factors has not been reported to our knowledge. Understanding the combined impact of graft choice with meniscal involvement in the presence of patient- specific factors may facilitate the development of patient specific rehabilitation protocols following ACLR. Therefore, the current study aimed to compare the post-operative outcomes at six months after ACLR between the levels of concomitant meniscal procedure (ACLR-only, ACLR-resect and ACLR-repair) while accounting for confounding factors, especially graft type. We hypothesized that regardless of graft type ACLR-only and ACLR-resect groups will have greater knee extension and flexion strength and will perform better on the hop tests and patient-reported outcomes than the ACLR-repair group.
Study design
This was a cross-sectional study conducted in a controlled laboratory setting as part of a large point-of-care collaborative research program. Written and verbal consent was obtained for each participant, and the university’s Institutional Review Board for Health Science Research approved this study.
Participants
Three hundred and fourteen patients with a history of ACLR were included for analysis. All patients had to have undergone a primary unilateral uncomplicated ACLR with a BPTB or HT autograft between 5 and 12 months prior to testing. Patients were excluded if they had a prior history of surgery on lower extremity, contralateral graft harvesting, treated articular cartilage lesion, or multiple ligament injury.
Surgical technique and rehabilitation protocols
Surgeons performed the ACLR arthroscopically using either HT or BPTB autografts. HT were fixated by means of interference or hybrid techniques, and surgeons used interference screws to fixate all patellar tendon autografts. The decision to repair or to respect the injured portion of the meniscus was left to the discretion of the physician based on meniscal tear characteristics and the consequent potential for healing and to optimize outcomes. Surgeons performed meniscal repairs by either an all-inside or an inside-out technique. They used an arthroscopic shaver to resect meniscal tears that were determined to be irreparable while maximizing the preservation of the uninjured part of the meniscus.
All patients were prescribed physical therapy following the surgery. Physical therapists received a protocol specific to the involvement of the meniscus procedure as well as graft specific recommendations to guide the progression of weight bearing, range of motion and exercise type. Regarding graft considerations, if a participant received a HT, isolated hamstring strengthening was delayed until 3 months post-operatively, as opposed to immediate hamstring strengthening being permissible in the cases of BPTB. Also, participants who received a BPTB were permitted to progress toward full weight-bearing running at 3 months post-operatively as compared to those who had a HT were encouraged to wait until 4 months post-operatively. Rehabilitation protocols specific to the meniscal procedure are summarized (Table 1).
| ACLR-only with/out resection | ACLR-meniscal repair | ACLR-meniscal root repair | |
|---|---|---|---|
| Weight Bearing | No limitations | 6 Weeks: 50% body weight maximum then progress to FWB | 6 Weeks: 25% body weight maximum then progress to FWB |
| Bracing | None | Yes: 4-6 weeks | Yes: 6 weeks |
| ROM | No limitations | 6 Weeks: Maximum knee flexion < 90 degrees | 6 Weeks: Maximum knee flexion < 90 degrees |
Table 1: Rehabilitation guidelines per meniscal procedure.
Procedures
Prior to being cleared for full participation by the surgeon, participants reported to the university research laboratory. All tests were performed during a single session. Participants performed a standardized warmup of walking on a treadmill at a self-selected speed at a minimum 3.0 MPH for 5 minutes followed by a period of self-directed stretching. Testing occurred in a consistent order for all participants.
Isokinetic strength testing: Quadriceps and hamstring strength were measured via peak torque during concentric extension and flexion, respectively, at a speed of 90°/second using a stationary multimodal Biodex systems IV dynamometer (System 3, Biodex Medical Systems, Inc, Shirley, NY). Participants were seated with their hip in 85 degrees of flexion, and a lap belt secured across their hips. Participants’ knees were flexed to 90° with a leg pad attached to the shank at approximately 4 cm proximal to the Achilles tendon insertion. Investigators instructed participants to keep their arms crossed and their head and shoulders upright during testing. To become familiar with the device, participants performed a minimum of three submaximal repetitions. During testing, investigators instructed the patients to provide maximal effort for a total of 8 repetitions. Verbal encouragement and visual feedback on a monitor was provided during the testing. For analysis peak torque for extension and flexion was normalized to body mass (Nm/kg).
Single-leg hop tests: To assess functional performance, participants completed the Single-Leg Hop for Distance (SLHD) and 6-meter Timed Hop Tests (THT) as previously described [14,15]. Participants completed 3 trials for each hop test on each limb and always performed the first trial on the contralateral limb, and alternated between limbs after each successful trial. A successful trial was defined as the participant maintaining their balance during the hop test and not touching down with the opposite limb. Participants performed a minimum of 3 practice trials followed by 3 maximal effort trials. For the SLHD the average of the 3 successful maximal effort trials were normalized to body height to provide a unit-less measure. THT was recorded as the average time of 3 successful maximal effort trials in seconds.
Patient-reported outcomes: All participants completed the International Knee Documentation Committee (IKDC) [16] to evaluate knee function, Tampa Scale of Kinesiophobia (TSK-11) [17] to assess fear of injury and pain, and the Tegner Activity Scale [18] to measure physical activity levels.
Outcome measures: The primary independent variable included meniscus group (ACLR-only, ACL-resect, ACLR-repair), and predictor variables included age, sex, time post-surgery, and graft type. The primary dependent variables included isokinetic knee extension/flexion peak torque, and secondary analyses involved SLHD, THT, TSK-11, IKDC and Tegner Activity Scale for current activity.
Statistical analysis
Comparison of demographic variables within meniscal procedure groups were assessed with Analysis of Variance Tests (ANOVA) and Chi-square analyses. All analyses were performed for the entire sample and for each subset of graft type. A Multivariate Analysis of Covariance (MANCOVA) was used to compare the effect of meniscal procedure during ACLR on the battery of outcome variables. Covariates include age, sex, time post-surgery, and graft type. For each dependent variable found to be statistically significant, an ANCOVA was performed for each graft type to determine the influence of meniscal procedure within the specific subset. Covariates included age, sex, and time post-surgery.
To assess the pass rate outcomes, a Limb-Symmetry Index (LSI) was calculated for each outcome measure. The LSI is the ratio of the surgical knee’s outcome measure divided by the nonsurgical knee’s outcome measure and normalized to 100%. A LSI value less than 100% indicates that the limb of the surgical knee has a deficit of the outcome score relative to the limb of the nonsurgical knee. For strength and hop tests variables, pass rates were analyzed for LSI>90%. Logistic regression was performed to compare the odds of participants in each meniscal procedure group achieving the pass rate. Age, sex, time post-surgery, and graft type were included as predictor variables in all regression models. If the logistic regression was statistically significant for a given dependent variable, a separate regression analysis was performed for each graft type with meniscal procedure as the independent variable and age, sex and time post-surgery as predictor variables. For all statistical analyses, the level of significance was set at alpha level ≤ 0.05 a priori. All statistical analyses were performed using SAS (version 9.3, SAS Institute, Cary, NC).
The data from the primary dependent variables were confirmed to be from a normal distribution by the Shapiro-Wilk test. All data were expressed as least square means and standard error as these are the data used in the MANCOVA analyses.
Demographics
Three hundred and fourteen participants with a history of ACLR were included in the study. The demographics are presented within the classification of meniscal procedure (Table 2) and subclassified by the graft type (Tables 3 and 4). When considering all graft types, the only difference between meniscal groups was sex (p=.007). Similarly, the participants who received a HT were comparable across all demographic variables except for sex (p=0.02) (Table 3). Within the BTB subgroup, there were no differences in the demographics of the meniscal procedure groups (Table 4).
| ACLR-only | ACLR-resect | ACLR-repair | p | |
|---|---|---|---|---|
| Sex(Male: Female) | 38:70 | 40:29:00 | 68:69 | 0.007 |
| Age | 19.89 + 4.57 | 20.56 + 5.39 | 19.14 + 4.71 | 0.12 |
| Height(cm) | 171.21 + 9.87 | 172.00 + 10.27 | 172.61 + 9.62 | 0.55 |
| Weight(kg) | 70.76 + 13.04 | 75.90 + 18.47 | 75.19 + 19.15 | 0.07 |
| TimePost Surgery (mo) | 6.64 + 1.26 | 6.67 + 1.28 | 6.66 + 1.40 | 0.99 |
Note: cm: centimeters; kg: kilogram; mo: months
Table 2: Participant demographics with all graft types. (Mean ± SD).
| ACLR-only | ACLR-resect | ACLR-repair | p | |
|---|---|---|---|---|
| Sex (Male: Female) | 05:13 | 13:06 | 28:16:00 | 0.02 |
| Age | 21.34 + 6.62 | 22.6 + 7.48 | 20.04 + 6.88 | 0.39 |
| Height (cm) | 169.26 + 9.32 | 173.52 + 12.70 | 171.31 + 10.30 | 0.48 |
| Weight (kg) | 70.62 + 13.95 | 78.50 + 21.16 | 72.11 + 20.21 | 0.39 |
| Time Post Surgery (mo) | 6.51 + 0.832 | 6.57 + 1.33 | 6.61 + 1.26 | 0.96 |
Note: cm: centimeters; kg: kilogram; mo: months
Table 3: Participant demographics with hamstring grafts. (Mean ± SD).
| ACLR-only | ACLR-resect | ACLR-repair | p | |
|---|---|---|---|---|
| Sex (Male: Female) | 33:57:00 | 27:23:00 | 40:53:00 | 0.14 |
| Age | 19.60 + 4.03 | 19.79 + 4.18 | 18.71 + 3.18 | 0.16 |
| Height (cm) | 171.06 + 9.98 | 171.43 + 9.27 | 173.22 + 9.28 | 0.42 |
| Weight (kg) | 70.78 + 12.93 | 74.91 + 17.47 | 76.64 + 18.57 | 0.05 |
| Time Post Surgery (mo) | 6.67 + 1.34 | 6.70 + 1.29 | 6.68 + 1.46 | 0.98 |
Note: cm: centimeters; kg: kilogram; mo: months
Table 4: Participant demographics with BPTB grafts. (Mean ± SD).
MANCOVA results
The MANCOVA revealed that the combined dependent variables were significantly different by levels of meniscal procedures (Wilks lambda=0.91, F (14,458)=1.87, p=.045). Univariate F test demonstrated that knee flexion peak torque and IKDC were significantly affected by meniscal procedure (Table 5). Significant pairwise comparison results are presented in Table 5.
| ACLR-only | ACLR-resect | ACLR-repair | F-Value | p-value | |
|---|---|---|---|---|---|
| Knee flexion peak torque (Nm/kg) | 0.99(0.03) c | 0.93 (0.03) | 0.89 (0.03) a | 3.44 | 0.03 |
| Knee extension peak torque (Nm/kg) | 1.72(0.05) | 1.60(0.06) | 1.67(0.04) | 1.34 | 0.26 |
| SLH (%) | 0.66 (0.02) | 0.67 (0.02) | 0.64 (0.02) | 0.82 | 0.44 |
| THT (sec) | 2.56 (0.07) | 2.52 (0.08) | 2.58 (0.06) | 0.22 | 0.8 |
| TSK-11 | 33.0(0.67) | 33.3(0.75) | 33.4 (0.55) | 0.12 | 0.89 |
| IKDC | 85.4 (1.37) c | 85.2 (1.55) c | 81.1 (1.13) ab | 4.14 | 0.02 |
| Tegner | 6.2 (0.20) | 6.3 (0.23) | 6.0 (0.17) | 0.82 | 0.44 |
Note: a : Statistically different from ACLR-only; b: Statistically different from ACLR-resect; c: Statistically different from ACLR-repair
Table 5: MANCOVA results of dependent outcomes measures for meniscal procedures. Data are reported as least squared means (standard error).
ANCOVA results for each graft type
ANCOVA of knee flexion peak torque for each graft type determined that no differences existed between the meniscal procedures of the HT subset. However, among the BPTB subset, ACLR-only demonstrated significantly greater knee flexion strength compared to the other groups (Figure 1). In contrast, ANCOVA for each graft type revealed that the ACLR-only and ACLR-resect groups scored significantly higher on the IKDC than the ACLR- repair group in the HT subset, but there were no differences within the BPTB group (Figure 2).
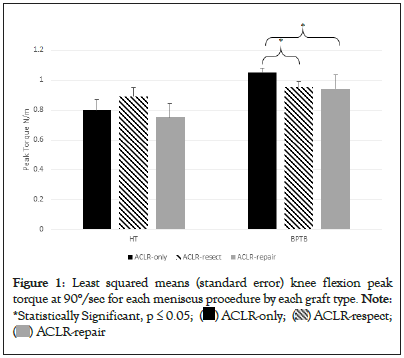
Figure 1: Least squared means (standard error) knee flexion peak
torque at 90°/sec for each meniscus procedure by each graft type.
Note: *Statistically Significant, p ≤ 0.05; ( ) ACLR-only; (
) ACLR-only; ( ) ACLR-respect;
(
) ACLR-respect;
( ) ACLR-repair
) ACLR-repair
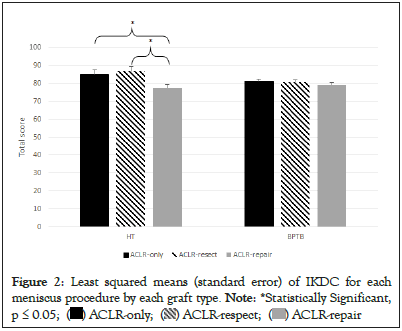
Figure 2: Least squared means (standard error) of IKDC for each
meniscus procedure by each graft type.
Note: *Statistically Significant,
p ≤ 0.05; ( ) ACLR-only; (
) ACLR-only; ( ) ACLR-respect; (
) ACLR-respect; ( ) ACLR-repair
) ACLR-repair
Logistic regression revealed that only knee flexion peak torque was statistically significant (Table 6). Within the BPTB subset, participants in the ACLR-only group had a higher odds of having an LSI>90% compared to the ACLR-resect and ACLR-repair groups. There were no statistical differences in the HT subset (Figure 3).
| Wald Chi-Square | p-value | |
|---|---|---|
| Knee flexion peak torque (Nm/kg) | 6.83 | 0.03* |
| Knee extension peak torque (Nm/kg) | 0.93 | 0.62 |
| SLHT | 0.38 | 0.82 |
| THT | 1.3 | 0.52 |
Note: *Statistically Significant, p ≤ 0.05
Table 6: MANCOVA results of dependent outcomes measures for meniscal procedures. Data are reported as least squared means (standard error).
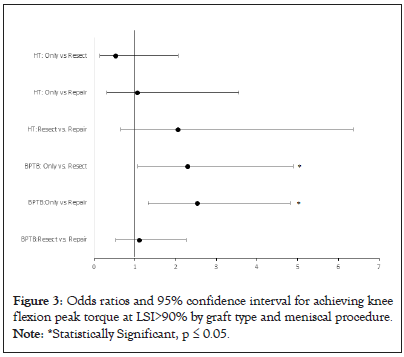
Figure 3: Odds ratios and 95% confidence interval for achieving knee
flexion peak torque at LSI>90% by graft type and meniscal procedure.
Note: *Statistically Significant, p ≤ 0.05.
We hypothesized that regardless of the graft type ACLR-only and ACLR-resect groups would have greater knee extension and flexion strength and perform better on the hop tests and patient-reported outcomes measures than the ACLR-repair group. We found that, only among patients with a BPTB, those in the ACLR-resect and ACLR-repair groups had decreased knee flexion strength compared to the ACLR-only group. If any meniscal procedure accompanies an ACLR with BPTB, there is a lower odd of achieving an LSI of 90% for knee flexion peak torque. Also, among participants with HT, subjective knee function was greater among the ACLR-only and ACLR-resect groups compared to the ACLR-repair group. No other significant differences were identified.
The distinctiveness of these findings lies within the confounding influences of graft choice on muscle strength. The inhibitory effects of the disrupted mechanoreceptors in an injured ACL result in decreased quadriceps activation and strength [19,20]. Furthermore, quadriceps activation appears to be more inhibited with greater structural damage to the knee [21]. Therefore, the margin for identifying a quadriceps strength deficit may be small regardless of the choice of graft material. Additionally, the morbidity of the graft site following BPTB graft can compound quadriceps weakness that may further mask the impact of meniscal repair on knee extension strength testing. These results are in agreement with previous work that reported ACLR-resect and ACLR-repair did not significantly influence quadriceps activation and strength post-ACLR [22-25]. Knee extension strength, therefore, may not be amenable to identifying the additive inhibitory influence of a meniscal procedure.
The influence of a meniscal repair on knee flexion strength may be similarly confounded by the use of HT grafts. It has been well established that using the autogenous semitendinosus as the graft material results in reduced short-term hamstring strength due decreased hamstring muscle volume [19,26,27]. The additional influence of a meniscal repair on hamstring strength among the HT subset, therefore, may not be quantifiable due to the strength deficit resulting from graft site morbidity. Knee flexion strength among patients with BPTB may be the most receptive condition to identify the impact of meniscal procedures on post-operative strength.
While this is not the first study to evaluate the effects of meniscal procedures on recovery from ACLR, this is the first report specifying the graft type. Previous ACLR research has considered the effect of meniscal procedures on hamstring strength only within heterogenous groups relative to graft type. At 6 months post- surgery, no differences in hamstring strength and limb symmetry between ACLR-repair and ACLR-only groups were reported [23-25]. The participants in two of these studies [23,25] were very similar in that greater than 90% of the subjects received a HT autograft. As noted previously, the effect of meniscus repair on knee flexion strength among patients with a hamstring tendon autograft may not be readily identifiable due to confounding factors. Therefore, a sample bias of these studies may have influenced their conclusions that meniscus repair did not influence hamstring strength. In the third study [24], the analyses did not control for the influences of age, sex and time post-surgery, so the impact of the meniscal procedure may have been imperceptible by their confounding effects. In contrast, the results of this study indicate that at least within the BPTB subset of ACLR patients, researchers and clinicians should carefully consider the influence of a meniscus procedure on hamstring function.
The influence of the hamstrings as a dynamic stabilizer to reduce ACL shear forces and injury mechanisms has been long accepted [28-30]. The importance of restoring optimal hamstring strength, in relation to knee extension strength, is essential for minimizing ACL reinjury, especially among athletes [31]. Therefore, the relevance of regaining hamstring strength to achieve biomechanical symmetry of sports movements must be considered for a safe return to full sports participation [32,33]. A previous study identified biomechanical characteristics of unplanned change of direction and double-leg drop jump that ably predict ACL reinjury [34]. Interestingly, within the same patient sample, the pass rate for hamstring strength was the only traditional strength and functional performance measure that was significantly different between the groups [34].
The implications of decreased hamstring strength are appreciated when assessing the muscle group’s activation during dynamic activities among fully rehabilitated ACLR individuals. Patients with significantly reduced biceps femoris activation immediately prior to landing from a dynamic hopping task were more likely to sustain a reinjury to the ipsilateral ACL [35]. Furthermore, during more intense tasks such as running downhill, anterior tibial translation is reported to be significantly greater as long as 2 years after ACLR with a repair of the medial meniscus [36]. In the lens of concomitant meniscal procedures health care providers must emphasize full recovery of hamstring function for a return to high activity levels.
A significant consideration to explain diminished hamstring strength and pass rates following ACLR-repair is the variability of the rehabilitation protocols. Historically, healthcare providers advocated for an accelerated rehabilitation protocol to minimize range of motion complications, muscle atrophy and consequent strength and functional deficits [37-39]. In contrast, following a meniscal repair, there is a lot of variability among rehabilitation protocols due to a concern of reinjuring the meniscus [9,40].
Rehabilitation restrictions that are common following a meniscal repair include the use of a knee brace and range of motion restrictions during the early post-operative period, slower progressions of weight bearing and therapeutic exercise and a more deliberate return to sport timeline [9,40]. As previously noted, our physicians apply the restrictions for brace use, weight bearing, ROM, and early exercise progression following a meniscal repair (Table 1). Intuitively, these restrictions may give rise to a delay, especially in the short- term follow-up period, in developing symmetry in muscle strength and coordination, though the restrictiveness of these protocols do not appear to influence the long-term clinical success rates among subjects who undergo a meniscal repair [9].
The combined rehabilitation restrictions from hamstring tendon graft and meniscal repairs may have resulted in the lower IKDC scores among HT participants with a meniscal repair. The potential for increased muscle atrophy and decreased neuromuscular coordination due to the initial six weeks of limited weight bearing following a meniscus repair may have impeded their functional progression. Furthermore, although there have been no reports of significant difference in IKDC between BPTB and HT [41], when considered in conjunction with a meniscal repair, the accrual of activity restrictions may manipulate the patients’ perceptions of their symptoms and function. Analyzing the IKDC may allow the clinician to identify specific activities or symptoms that the patient determines as difficult or limiting. Individualized rehabilitation programs may address these shortfalls to not only improve the patients’ function but also their confidence. Finally, these findings must be considered with caution because although the differences in scores between groups are statistically significant, the clinical relevance has not been established.
The influence of meniscal repair on short-term clinical outcomes is dependent on the graft choice. Recovery of the quadriceps strength does not appear to be significantly influenced by the addition of a meniscal procedure to ACLR regardless of the graft type. However, to optimize full recovery following ACLR with BPTB and a meniscal procedure, rehabilitation should intensify hamstring strengthening exercises. The influence of activity restrictions from meniscal repair and HT on patients’ subjective knee assessments should be routinely monitored to assist with individualizing their rehabilitation programs.
This study had several limitations. Firstly, athletes and non-athletes were included in the study. Athletes may have different targets and motivational levels during rehabilitation which could have affected the overall outcomes. Secondly, patients did their rehabilitation at different clinics using the rehabilitation protocols as a guide. Differences in the exercise and functional progression, including the home-based therapy, may have influenced the results and resulted in information bias. This study is retrospective analysis of a large database. Therefore, patients were not randomized as to the graft type or meniscal procedure, and this may have resulted in a selection bias. Within the known factors that influence ACLR outcomes, we statistically controlled for the influence of age, sex, and time post-surgery, and subgroup analyses were performed within each graft-type. Additionally, we did not report whether the meniscal procedure was performed on the medial or lateral meniscus, so the influence of laterality was not assessed.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] (All versions) [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Moler C, Cross K, Kaur M, Bruce A, Hart J, Diduch D, et al. (2022) Influence of Graft Type and Meniscal Involvement on Return to Sport Outcomes six Months after Anterior Cruciate Ligament Reconstruction. Int J Phys Med Rehabil.11:657.
Received: 17-Oct-2022, Manuscript No. JPMR-22-19748; Editor assigned: 21-Oct-2022, Pre QC No. JPMR-22-19748 (PQ); Reviewed: 10-Nov-2022, QC No. JPMR-22-19748; Revised: 17-Nov-2022, Manuscript No. JPMR-22-19748 (R); Published: 28-Nov-2022 , DOI: 10.35248/2329-9096.22.11.657
Copyright: © 2022 Moler C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.