International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2020)Volume 8, Issue 1
Background: Extension for Community Healthcare Outcomes (ECHO) is a programme that employs videoconferencing technology to train community-based primary care providers to improve and standardize care across a wide geographical region. This method has not yet been trialled in the UK for improving the capacity of primary care services in managing common musculoskeletal (MSK) complaints.
Aim: The aim was to assess the impact of introducing a year-long MSK ECHO education programme in Northern Ireland for general practitioners (GPs).
Design and setting: Monthly sessions were held consisting of teaching and case based discussions. Each session lasted on average 90 minutes. A ‘hub’ consisting of local GP lead educators, supported by colleagues from secondary care, where linked to GPs around Belfast using video conferencing technology.
Methods: Topics covered were chosen by participants at the start and covered common MSK complaints in primary care. An initial questionnaire was performed at the start and compared to an evaluation questionnaire at the end.
Results: Ten GPs completed the evaluation one year after the project was initiated. The weighted average of the selfconfidence scores in examining a range of individual body parts in general practice increased from a baseline of 3.45 to 4.08. There was an increase in self-assessed ability in diagnosing and treating a number of common MSK complaints and the whole year-long programme was delivered for £ 14,980.
Conclusion: This trial shows how a 12-month ECHO intervention can improve self-efficacy in a number of MSK capacities within GP. These preliminary results suggest that ECHO is an affordable, effective solution for providing postgraduate education to working GPs.
Extension for Community Healthcare Outcomes (ECHO); General practice (GP); Postgraduate medical education
Extension for Community Healthcare Outcomes (ECHO)
ECHO [1] is a tele-mentoring movement that transfers specialist knowledge from secondary and tertiary medical services to primary care and community-based teams. The programme aims to be an affordable but high-impact solution to the increasing demand on secondary and tertiary healthcare services, as well as expanding the capacity of both primary and community care, in keeping with current models of healthcare [2]. The intention is that a more patients will have access to best-practice speciality care, thus reducing the health disparities nationwide and improving patient outcomes. The ECHO model connects an academic ‘hub’ of specialists with numerous multi-disciplinary primary care ‘ spokes ’ ; strengthening communication and relationships between the primary and secondary healthcare services. Key messages are delivered by the specialist practitioners and core learning is illustrated through case-based discussion. ECHO is centered on four key principles: using multipoint video-conferencing technology; employing evidencebased best practice; using case-based learning to enhance speciality training in primary care; and adapting services through monitoring plus evaluating outcomes from the ECHO model.
Current demand for MSK services in the healthcare system
The current demand on both primary and secondary care services for musculoskeletal (MSK)-related conditions is significant. 20% of people consult a general practitioner (GP) regarding an MSK problem every year [3], with one in seven consultations concerning MSK conditions [4] and MSK issues are addressed in 12% of GP appointments [5]. An estimated 17.8 million people live with MSK conditions within the UK, i.e. approximately 28.9% of the total population [6]. Furthermore, MSK conditions contributed 1.36 million admissions to consultant care in England during 2016-17; 8.2% of all admissions to consultant care [7]. The resultant strain on secondary services is evidenced through prolonged waiting times, for example the knee and hip elective replacement waiting times averaged approximately 105 days in England, 2015-two of the five highest average waiting times [8]. Increasing capacity and quality of care in the primary care sector should reduce the demand for secondary care referrals, and thus address these healthcare pressures.
Belfast GP Federation
Belfast GP Federations have proposed the delivery of a community-based elective care service for MSK conditions consisting of two main elements. Firstly, a programme of education (primarily delivered via ECHO), peer review and local guideline implementation for common MSK conditions, with the intention to increase quality and capacity in primary care. Secondly, a programme of building capacity to improve access to services within the community by providing primary care based clinics and a peer support clinical network. Moreover, the ECHO model is in keeping with the “Triple Aim” [9] of a wider health service agenda, highlighted in the Bengoa Report [10] and the Elective Care Plan (Transformation and Reform of Elective Care Services) [11]. In addition to increasing accessibility to care and management of conditions in the primary care setting, ECHO should enable earlier intervention in chronic MSK conditions and thus avoid/delay expensive secondary care referral where it is clinically appropriate to do so.
To date there have been a number of ECHO trials worldwide, though limited research has been performed on musculoskeletal conditions. One paper examining ECHO’s use in chronic pain and opioid stewardship for remote communities within Ontario concluded that ECHO was a promising model for these communities, and that its strengths lie within its simplicity, adaptability, and use of existing telemedicine infrastructure [12]. One systematic review [13] reasoned that project ECHO has the potential to be a cost-effective method to increase primary care knowledge and patient access to healthcare in remote locations, but further research is required to determine its efficacy and potential barriers. Thus far there is a limited evidence base for ECHO within the UK. One UK research group performed a 6- month pilot study on the efficacy of the ECHO model in educating and supporting community hospice nurses. Once again, this trial supports ECHO, stating that the low-cost, highimpact ECHO model provides an affordable solution to addressing growing demands [14]. We therefore wanted to assess the effectiveness of delivering an MSK education programme for GPs within the Belfast area via ECHO.
The aim of this project was to assess the impact of introducing a year-long MSK education programme in Northern Ireland for GPs in terms of increasing MSK knowledge and confidence in managing common MSK conditions in general practice, delivered through an ECHO programme.
The MSK ECHO trial in Northern Ireland ran from January 2018 to January 2019. The 90 minute sessions ran monthly, with the first session focusing on introducing the participants to the protocols, and the final session based on evaluation and reflection. Ethical approval was not required for this study as it was an evaluation of a new method of teaching. The model was delivered across the Belfast ICPs (Integrated Care Partnerships) region, which is essentially all the GP practices within the Belfast area. The range of topics was determined by the participants and included the: knee; shoulder; fibromyalgia; inflammatory arthritis in primary care; radiology in primary care; hand and wrist; foot and ankle; and, the Northern Ireland regional spinal pathway.
The Hub in this ECHO model consisted of the ICP/Federation training HUB leads (two local Belfast GPs,NH and IR) who were supported by colleagues from secondary care, including physiotherapists and consultants from orthopaedics, rheumatology, and radiology. These clinical leads (NH, IR), with input from the secondary care experts, developed plus delivered a skill-sharing service to the local GPs that covered MSK assessments, investigations and management of common primary care MSK conditions. The ‘ Spokes ’ were then individual GPs who formed part of the MSK Primary Care Network and were contracted to deliver primary care MSK services.
One technical barrier anticipated was the lack of equipment capability across participating GP practices. GPs are not permitted to use the GP network Wi-Fi on personal devices, therefore webcams had to be provided to practices without cameras on their health board device- funding for which was included in the application to run this course. Estimated costs calculated prior to the trial were £ 95,760 for the year; split £ 15,120 and £ 80,640 between the Hub and Spoke components. These costs included the lead session training costs (2 leads), ICT requirements, consultant/secondary care colleagues’ time, and the GP ICP/Federation participants (maximum 24 participants).
18 GPs participated in the MSK ECHO trial. Prior to starting, each participant completed a questionnaire covering demographic details, prior MSK experience, confidence in examining, treating and diagnosing various MSK complaints, confidence using the Northern Ireland Spinal Pathway, and confidence injecting common joint areas. They were also asked about their satisfaction with the quantity and quality of MSK education opportunities currently available for GPs. Finally, the participants were asked what they would like addressed during the programme and what they would like to gain from it (see Appendix I for the questionnaire).
Measurable outcomes established prior to the trial included: evidence of a reduction in referrals; patient satisfaction; GP satisfaction; reflection via annual appraisals; weekly surveys from the knowledge exchange to ensure continuous learning; and, overall summative assessment of Knowledge Framework. However, this paper focuses on reporting the questionnaire responses pre- and post-participation in the ECHO teaching programme.
Ten of the original 18 GPs completed the final evaluation questionnaire, giving a response rate of 55.6%. At baseline, the majority were male (77.78%; 14 males, 4 females) and the average age was 49.4 years (range 37-63 years old). All participants were Members of the Royal College of General Practitioners. Other qualifications included: Fellowship of the Faculty of Sport and Exercise Medicine (F.FSEM) (16.67%; 3 participants); Diploma in Sport and Exercise Medicine (16.67%; 3 participants); Orthopaedic/Musculoskeletal Diploma (11.11%; 2 participants); Membership of the Royal College of Physicians (MRCP) (5.56%; 1 participant); and a Master ’ s degree in another relevant area (5.56%; 1 participant). The participants’ average number of years working as a GP and/or GP Partner was 19.8 years (range 8-34 years). Only 70% of those who completed the evaluation, had experience in MSK prior to this ECHO educational programme. Of the final respondents, 20.00% participated in 4-6 ECHO sessions, while the remainder participated in 7-9 sessions. Overall, 11 GPs on average attended each ECHO session, with a total of 16 case presentations discussed.
The participants were asked to rate their confidence out of five on a number of common primary care MSK components both before and after the intervention, with 1 inferring no/little confidence and 5 high confidence. Figure 1 shows that the mean weighted average confidence prior to starting the programme was 3.45 (range 3.29-3.65), and following ECHO was 4.08 (range 3.5-4.3); an improvement of 0.63 (+12.6%).
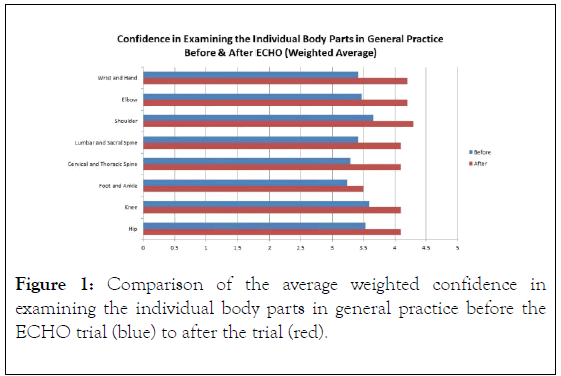
Figure 1. Comparison of the average weighted confidence in examining the individual body parts in general practice before the ECHO trial (blue) to after the trial (red).
Comparing the results before and after the MSK ECHO Network shows that the ECHO programme has helped improve the understanding of common MSK conditions (Figure 2), management of chronic MSK pain in primary care, confidence in undertaking common injections in primary care (Figure 3), and the understanding between primary and secondary care (Figure 4). The participants were also asked their general comments on the course, what they found most useful about the ECHO programme (Table 1) and aspects to improve the ECHO programme in the future (Table 2). The total cost of delivering this year-long education programme was £ 14,980.
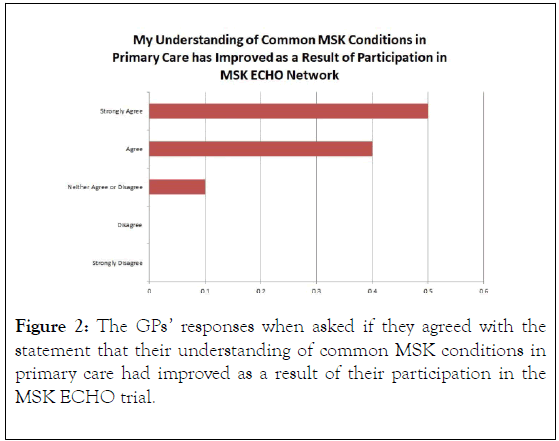
Figure 2. The GPs’ responses when asked if they agreed with the statement that their understanding of common MSK conditions in primary care had improved as a result of their participation in the MSK ECHO trial.
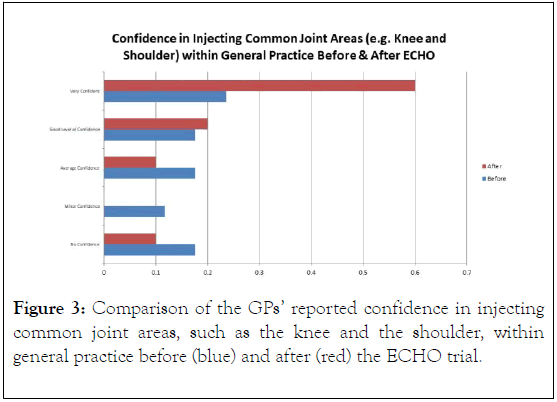
Figure 3. Comparison of the GPs’ reported confidence in injecting common joint areas, such as the knee and the shoulder, within general practice before (blue) and after (red) the ECHO trial.
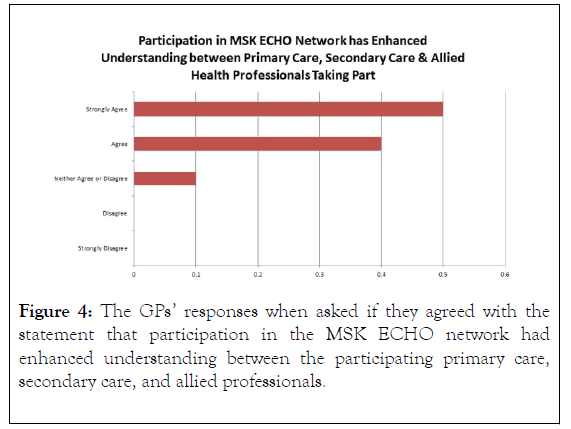
Figure 4. The GPs’ responses when asked if they agreed with the statement that participation in the MSK ECHO network had enhanced understanding between the participating primary care, secondary care, and allied professionals.
| What Aspect of MSK ECHO has been Most Useful? | |
|---|---|
| 1 | Opportunity to discuss with experts. |
| 2 | Good overview with allied health professionals (AHPs) input as well |
| 3 | Really enjoyed the lectures/talks by 'experts' but more importantly, the 2-way dialogue which it then generated. Peer group support with other GPs and secondary care colleagues. |
| 4 | Very useful topics every time, common case studies applicable to everyday scenarios |
| 5 | Consultant input into clinical cases |
| 6 | Contact with other clinicians of similar interest. Seeing the faces of and meeting new consultants |
| 7 | Learning |
| 8 | Specialist presentations (when done well) |
| 9 | Case based discussions with consultant input |
| 10 | I enjoyed the fibromyalgia session and the recent knee session. I also like learning and interacting with peers |
Table 1: The GPs’ written responses when asked what aspects of the MSK ECHO trial had been most useful
| Is There Anything That Could Have Been Done Better or You Would Like To See Included? | |
|---|---|
| 1 | More primary care experts |
| 2 | Sometimes had feeling that we were disengaged from the process |
| 3 | There should be more opportunities to cover other common topics of MSK conditions in primary care. |
| 4 | Maybe doing a session on joint (esp shoulder) examination. Would need a live model at the hub |
| 5 | Maybe practical procedures, attend musculoskeletal clinics, videos of joint injections |
| 6 | It got better as the sessions progressed and they became less hospital orientated |
| 7 | I did not find our own case presentations particularly useful. I would suggest participants submitting cases/questions prior to the session and allowing the "expert" to incorporate these within their presentations-subsequent Q@A could then ensure these areas were fully covered. |
| 8 | Specialist presentations (when done well) |
| 9 | No |
| 10 | Possibly a mix of ECHO and face to face sessions |
Table 2: The GPs’ written responses when asked what could have been done better or what they would have like to see included in the MSK ECHO trial.
Summary
This initial MSK ECHO trial consisted of a number of experienced general practitioners, of which a significant number had noteworthy MSK exposure and/or relevant qualifications. These practitioners (‘spokes’) attended monthly videoconference meetings with secondary care experts (the ‘hub’) to learn and discuss MSK topics and cases over a one year period.
Strengths and limitations
This paper is the first of its kind in assessing MSK teaching delivered via ECHO in the UK and has begun to show the potential benefits of employing an ECHO style model to expand the capacity of primary care in diagnosing and treating common MSK complaints. The results clearly show improvements and warrant further research to continue. The videoconferencing style can access hard-to-reach practices that may be omitted in traditional face-to-face education and thus helps implement standardised care of patients. Griffiths and Miller provide a good summary of the benefits- including overcoming physical and geographical boundaries and reducing feelings of intimidation or discomfort associated with new surroundings, and limitations- such as the dependence on access to the correct software and equipment and reliance on personal motivation, of e-mentoring in medicine [15].
One downfall of the study design was the response rate. Though this trial started with a relatively small cohort of participants (n18), the relatively low response rate of 55.56% may skew the results. Of those GPs who did complete the evaluation session, 20% only participated in 4-6 out of the 10 sessions held. These two factors should be investigated to establish how to increase the compliance to the ECHO schedule and ultimately improve the results.
Comparison with existing literature
Other ECHO trials also generally lasted 1-2 hours but, contrastingly, meetings were held weekly [14,16-18]. The duration of these trials ranged from three 12 week pilots [16] to 172 weekly ECHO sessions [18]. Wood et al. observed positive associations between participants’ length of engagement and the degree to which they felt part of the community of practice [18].
Participants completed an initial questionnaire (n=18) and an evaluation questionnaire (n=10) at the end of the year which equates to a follow-up rate of 55.6%; not dissimilar to other trials [16,18]. Some trials investigated further the main barriers to attendance, for example Johnson et al. performed three 12 week series allowing the programme to be revised to improve the participant experience [16].
Our results show an increase in confidence and understanding of all the MSK conditions that were covered during ECHO. This is in line with other research which primarily used similar self-efficacy and feedback questionnaires/focus groups [14,16-18] and objective measurements of knowledge [14]. Furthermore, there was an increase in confidence in diagnosing and treating almost all commonly presenting MSK conditions, with injecting common joint areas and treating chronic MSK pain showing particular progress. The weighted confidence in examining the individual body parts increased across the board; with the average rising from 3.45 to 4.08 (Figure 1). The greatest improvements were observed in cervical and thoracic spine (+25%), while foot and ankle showed the least (+8%).
In addition, participants had an opportunity to provide written feedback similar to previous research [16,14]. A significant number reported increased confidence in MSK practice as well as improved knowledge and understanding. The case-based learning, specialist presentations, and the two-way discussion with consultant expertise were reported to be some of the more helpful aspects of ECHO. Suggested improvements included involving more primary care experts, reducing the hospitalorientation of the discussions, and the future inclusion of practical sessions such as live models and MSK clinics. Though this latter suggestion may contradict the fundamental basis of ECHO whereby it can be taught at a distance (and thus have a broader inclusion), a mix of traditional ECHO and face-to-face sessions was mentioned relatively frequently.
In line with our results, some previous research highlights the need or analyses the use of distance learning and e-learning methods, such as telemedicine, in postgraduate medical education and practice [15,19-22]. For example, the multiprofessional e-learning package maternity PEARLS was an interactive distance-learning tool that demonstrated significant improvement in skills post-training [19]. Video consultations are already part of the GP education and assessment programme and it has been suggested that this technology could be used to educate both the doctor involved and those actively observing [20].
Implications for research and/or future practice
The actual economic cost tallied £ 14,980-a fraction of the preliminary estimated cost of £ 95,760. Though this particular study was principally subjective in its follow up, future research should focus on ECHO ’s long-term impact on primary care referrals and diagnoses, waiting times for secondary care, and the cost-benefit ratio of implementing the programme on the NHS’s limited budget. As this study has revealed significant benefits of ECHO with only a small financial impact, introducing it into the NHS as part of a wider research programme could be considered in order to start reaping the rewards and reducing the pressure on secondary care services as soon as possible.
How this fits in
Previous research shows that ECHO is a low-budget high-impact method of increasing participant self-efficacy and knowledge over a large geographical area. It is hoped that ECHO will minimise disparities in healthcare across the UK, increase capacity of primary plus community care and thus decrease demand on secondary care services, and have minimal financial implications on the NHS. This research demonstrates that engagement of practitioners in ECHO can increase their understanding and confidence of common MSK complaints in general practice with minimal economic impact.
Comparing the questionnaire results before and after this MSK ECHO trial within primary care has shown that this style of group-based learning centred on case-based discussions can significantly improve primary care practitioners’ confidence and understanding of common MSK complaints. Thus, ECHO shows promise in being a cost-effective solution to the ever increasing demand on secondary care. Though future research is indicated to improve its efficacy and to quantify the cost-benefit of the model, it appears to be in the nations’ interest to start employing an ECHO-style education programme across its primary care services to enhance quality of care and to prevent rising waiting times for secondary care services.
None of the authors have any competing interests to declare.
All data related to this study has been published in this paper.
Citation: Spalding K, Ryans I, Heron N (2020) Improving the Delivery of Musculoskeletal Education in Primary Care Using the Innovative Echo (Extension for Community Healthcare Outcomes) Technology. Int J Phys Med Rehabil 8: 536.
Received: 20-Jan-2020 Accepted: 03-Feb-2020 Published: 10-Feb-2020 , DOI: 10.35248/2329-9096.20.08.536
Copyright: © 2020 Spalding K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.