International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2024)Volume 12, Issue 1
Background: Falls and their consequences are a huge burden for older women living in the community as they are the main cause of loss of autonomy and disability. The most effective intervention to address the problem is based on exercises that target balance. Older women experience falls and the consequences of them more often. It is proven that the best way to adress this problem is with regular and targeted exercise. This is a protocol that investigates the effectiveneess and the compliance of an exercise protocol in a dynamic platform to adress balance disorders. The protocol has been proven to be both effective and have a good compliance, wich makes it an excellent alternative to classical exercise regimens.
Aim: The aim of the study was to analyse the effectiveness and the compliance of a dynamic platform-based protocols, where not much is known, in targeting falls, in older women living in the community.
Design: This was a randomized control trial.
Setting: An outpatient Balance Rehabilitation Clinic in a tertiary University Hospital.
Population: Results from 20 women all of them potential fallers, 10 in the intervention group and 10 in the control group (no intervention), were analyzed.
Methods: Older women with balance disorders were screened for balance disorders with the the mCTSIB test of the dynamic platform, if positive further evaluation was performed with the miniBEST and SPPB test. Based on the miniBEST (less than 18), the women were placed randomly in the intervention or control group. The intervention group completed 36 sessions three times per week for 30 min. The control group did not receive any intervention.
Results: Dynamic platform exercise programs were proven to be effective (mini-BEST, p<0.006; mCTSIB, p<0.02; SPPB, p<0.02) in balance rehabilitation and therefore fall prevention. The results also show that good compliance was achieved with a p<0.001, and the % of patients that adhered to the protocol was up to 96%.
Conclusions: We can conclude that that fall prevention exercises on a dynamic platform are effective and with good compliance. Platform exercise is an ideal start for older community dwellers to find in a protected environment the beginning of the thread that will lead them to a change of lifestyle and, therefore, to long-term health.
Falls; Balance; Exercise; Rehabilitation dynamic platform; Older women; Community dwellers
LL: Latero-Lateral index of stability; AP: Anteroposterior; OIS: Overall Index of Stability; CGA: Comprehensive Geriatric Assessment; ADL: Activities of Daily Living; MNA: Mini Nutritional Assesment; GDS: Geriatic Depression Scale; MMSE: Mini Mental State Evaluation; mCTSIB: modified Clinical Test of Sensory Interaction in Balance; miniBEST: mini Balance Evaluation System Test; SPPB: Short Physical Performance Battery; PMR: Physical Medicine and Rehabilitation
Falls in older people and their consequences are a huge burden for patients and the health care system as they have important economic [1,2], and personal [3], costs. People with fall-related injuries, such as hip fractures, fail (50% of them) at large to regain their previous level of functioning [4] and they also have a high mortality rate, between 8.4% and 36.0% during the first year following hip fracture [5].
In the past decade, research on fall prevention strategies has been extensive. Multicomponent protocols, which address many risk factors for falls, are a more efficient way to address this problem, but if we look at a single strategy, exercise alone is the most efficient way to approach fall prevention in older people [6]. The Cochrane analysis of 2019 [7], clearly demonstrated that to have an effect, the exercise program should absolutely challenge balance. Furthermore, a more recent meta-analysis demonstrated that the duration of this program could not be determined, because all types had a positive impact on fall prevention [8]. All the exercise protocols analyzed in these reviews were group or individual exercise programs performed by instructors.
However, little is known about the effectiveness and compliance of dynamic platforms, which are increasingly used to assess balance, in the implementation of exercise protocols to improve balance in older people.
This was a study on a fall prevention dynamic platform exercise protocol for older women living in the community. With this protocol, we wanted to assess whether a dynamic platform could be an alternative to group exercise or individual programs, the advantages and disadvantages, and compliance of the patients to the protocol.
Population
This is a Randomized Control Trial, Twenty-two women with balance disorders, aged 65-85 years of age, were randomly selected to either participate in the balance rehabilitation program (intervention group) or to be part of the control group. The randomization used was for every second person in the control group (no intervention).
The inclusion criteria were age >65 years, community dwelling, balance disorder, good understanding of the Greek language, and willingness to participate in the study. Exclusion criteria were respiratory or cardiac failure, active cancer, inability to maintain the upright position with or without technical aids, severe dementia, hospitalization or major operation in the last 6 months, major neurological disease (stroke, extrapyramidal syndrome, or polyneuropathy), and leg length discrepancy of >2 cm. Figure 1 shows the CONSORT diagram.
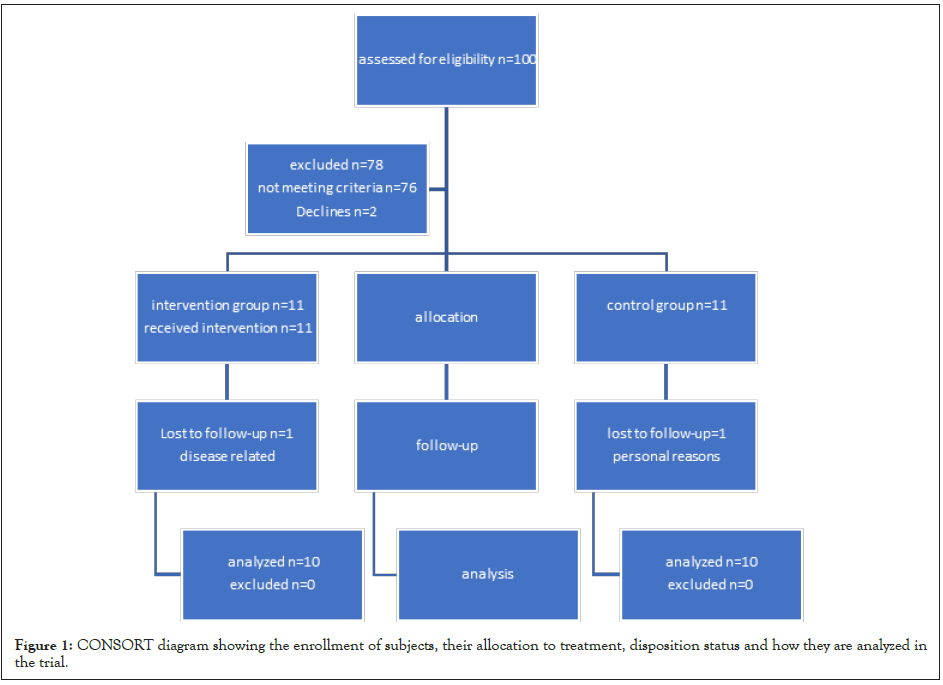
Figure 1: CONSORT diagram showing the enrollment of subjects, their allocation to treatment, disposition status and how they are analyzed in the trial.
Setting
The protocol was performed at the outpatient Balance Rehabilitation Clinic of a tertiary University Hospital. The equipment used was a Biodex Balance System (Biodex Balace System SD (BBS) System™ SD-Static and Dynamic Balance Assessment, Static and Dynamic Training. Biodex Medical Systems, Inc. 20 Ramsey Road Shirley, NY 11967-4704 U.S.A.) (Biodex Manual). This is a circular dynamic platform that measures the degree of tilting around each axon. It uses sensors to detect body tilting and can be regulated in a way that impedes motion (static mode), or it can tilt (dynamic mode) and provoke the patient further. The patient’s body position was measured and recorded on a screen. Data from each session were gathered and stored for further analysis. The platform tilts up to 20 in every direction with 12 (12 more stable to 1 less stable) a level of stability according to the resistance of the string, and every resistance lasts for 3,75 seconds. The calculations of the Latero- Lateral index of stability (LL) and Antero Posterior (AP) index of stability and, accordingly, the Overall Index of Stability (OIS) comes from the combined degrees of tilting around the AP and LL axes.
Protocol
All the women enrolled in the study were community dwellers. They were referred to the outpatient clinic of balance rehabilitation for evaluation. The evaluation protocol was based on the Comprehensive Geriatric Assessment (CGA) [9], and the domains were physical functioning, nutrition, polypharmacy, depression, fear of falling, depression, and cognitive decline, which are closely related to falls. Upon evaluation, all fall- related conditions, such as polypharmacy, were managed (like polypharmacy etc.). A thorough clinical examination that could reveal a pathological entity related to falls was performed based on which more diagnostic procedures could be performed. Finally, laboratory analysis was performed to identify whether electrolyte, nutritional, or vitamin deficiency was present. In particular, the vitamin D level that is closely related to falls was always evaluated, and if there was any deficiency, it was always addressed before any further intervention, as lack of vitamin D (less than 20 ng/dl) is closely related to falls [10].
In particularly the CGA for fall evaluation included the following tools, the START-STOPP tool [11], for inadequate prescription, the Fried criteria [12], for the diagnosis of frailty, the Mini Nutritional Assessment [13], for nutritional assessment, the SARC-F tool [14], for sarcopenia, the Mini Mental State Evaluation (MMSE) [15], for cognitive impairments, the Geriatric Depression Scale (GDS) [16], the evaluation of Activities of Daily Living (ADLs) with the Katz scale [17], the Instrumental Activities of daily Living (IADLS) with the Lawton Brody index [18], the Short Physical Performance Battery (SPPB) [19], for motor functioning, and the Fear of falls with the FES-1 (Fear of Falling I) [20].
In particular, the evaluation of balance was performed with the mCTSIB (modified Clinical Test on Sensory Interaction on Balance) of the dynamic platform and miniBEST (mini Balance Evaluation System Test). The mCTSIB of the BIODEX BBS has proven reliability and validity in measuring balance in older women living in the community [21]. We performed the Mini- BEST if the results were not within the normal range. This test is considered the most comprehensive tool for balance evaluation in older adults living in the community [22]. We used the Greek translation of Lampropoulou, et al., with proven intercultural adaptation [23]. As reported by Godi, et al., a score of 18 was used as a baseline to separate women with a higher (less than 18) and lower (>18) risk of falls [24]. Women with a score less than 18 were randomly assigned (every second woman to the control group) to be in the control or interventional group, and the allocation was made by the physician who did not perform any of the balance tests.
Both groups were evaluated at the beginning and end of the study. The balance rehabilitation program consisted of 3 sessions per week, with duration of 30 min per session, for a total of 36 sessions. In compiling our own protocol, we relied on meta- analyses that proved that balance exercises should have adequate dosage and duration, challenge balance, and recommended for 3 hours per week as ideal [25]. The program was very demanding, and the 3 hours session was not well tolerated in the short pilot we ran before; thus, we decided to use a 30 min session with a total of 90 minutes per week.
The same physical therapist delivered the protocol through the dynamic platform in the same way, meaning that in each session, the patient was exposed to all diverse types of exercises generated by the software so that each one had another way to challenge balance. The patient would start with the easiest level and proceed to the more difficult one. The patient was also instructed to use the handrail whenever she experienced an impending fall. All progress was noted, as well as compliance in every session and the use of handrails.
The primary outcome after the intervention was the possible gain in balance with the mCTSIB and Mini BEST test. The secondary outcome was compliance during the intervention period.
Statistical analysis
All score variables were found to be non-parametric according to the Shapiro-Wilk test for composite normality. Therefore, descriptive statistics were provided in the form of medians (Q1- Q3), and non-parametric tests were applied. Specifically, controls and cases were compared using Wilcoxon’s rank-sum test, while pre versus post-comparisons were performed using Wilcoxon’s signed- rank test. The overall comparison of case versus control post-scores with their pre-scores as covariates was assessed using non-parametric Analysis of Covariance (ANCOVA). Finally, the compliance ratios of our study and those of other studies were compared using the binomial z-test for proportion. All statistical tests were two-sided, and statistical significance was set at p<0.05. Statistical analysis was performed using the R project for statistical computing and R-Studio IDE, two well-known open-source products.
Table 1 summarizes the outcomes of the statistical analyses. The significant outcomes were as follows: The intervention was from 1/01/2018 to 9/2019, and stopped because of lack of funding.
| Variable | Control vs. Case pre | P-value | Control vs. Case post | P-value | Post minus pre in control | P-value | Post minus pre in case | P-value | Non-parametric ancova p-value |
|---|---|---|---|---|---|---|---|---|---|
| HG max | 20.6 (19.12-22.58) vs. 17.1 (14.7-20.1) | 0.089 | 19.75 (18.62-23) vs. 18.8 (16.1-21.3) | 0.57 | 0.25 (-1.9-1.4) | 1 | 0.9 (-0.58-3.32) | 0.153 | 0.825 |
| velocity | 0.78 (0.64-1.07) vs. 0.68 (0.58-0.76) | 0.14 | 0.85 (0.65-0.97) vs. 0.71 (0.67-0.87) | 0.935 | -0.01 (-0.03-0.02) | 0.678 | 0.11 (-0.03-0.25) | 0.25 | 0.085 |
| MNA | 10.5 (9-13.75) vs. 10.5 (9-11.75) | 0.669 | 11.5 (9.25-14) vs. 10.5 (10-12) | 0.786 | 0 (0-1) | 0.41 | 0.5 (0-1) | 0.12 | 0.422 |
| MMSE | 26.5 (23.5-27.75) vs. 28 (27.25-29) | 0.071 | 27.5 (23.75-28.75) vs. 28.5 (26-29) | 0.281 | 0 (0-1) | 0.203 | 0.5 (-0.75-1.75) | 0.724 | 0.851 |
| GDS | 5 (2-7.75) vs. 3 (2-4) | 0.237 | 5 (2.25-8) vs. 4 (2.25-5) | 0.515 | 0 (0-0) | 1 | 1 (-0.75-2) | 0.28 | 1 |
| TUG | 11.25 (10.02-12.75) vs. 15.25 (13.51-16.7) | 0.035 | 11.98 (10.85-13.88) vs. 12.28 (10.58-15.86) | 0.739 | 0.21 (-0.01-1.67) | 0.554 | -1.95 (-3.03--0.95) | 0.084 | 0.409 |
| miniBEST | 14.5 (12.25-16) vs. 13.5 (11.5-15.75) | 0.703 | 14 (12-16.75) vs. 16.5 (16-17.75) | 0.061 | 0 (-0.75-0) | 0.572 | 3 (3-5.5) | 0.006 | 0.039 |
| miniBEST domain1 | 3.5 (3-4) vs. 3 (2-3.75) | 0.328 | 3 (3-3.75) vs. 3.5 (3-4) | 0.398 | 0 (-0.75-0) | 0.424 | 0.5 (0-1) | 0.053 | 0.357 |
| miniBEST domain2 | 3 (2-3.75) vs. 3 (2.25-4) | 0.507 | 3 (2.25-3.75) vs. 4 (3-4) | 0.06 | 0 (0-0) | 0.773 | 1 (0-1) | 0.066 | 0.095 |
| miniBEST domain3 | 3.5 (2-4.75) vs. 3 (2-3.75) | 0.428 | 3 (3-4.75) vs. 4 (3-4) | 0.407 | 0 (0-0.75) | 0.424 | 1 (1-1.75) | 0.012 | 0.113 |
| miniBEST domain4 | 4.5 (4-5) vs. 5 (4.25-5.75) | 0.477 | 5 (3.25-5) vs. 6.5 (5-7) | 0.034 | 0 (0-0) | 0.586 | 2 (0-2) | 0.028 | 0.359 |
| SPPB | 8 (5.25-9.75) vs. 5.5 (4.25-6) | 0.078 | 7.5 (6.25-9) vs. 7 (6-8.75) | 0.702 | 0 (-1-1.5) | 1 | 1.5 (1-2.75) | 0.02 | 0.17 |
| SPPB domain1 | 3 (2-4) vs. 2 (1.25-2) | 0.084 | 2.5 (2-4) vs. 3 (2-3.75) | 0.872 | 0 (-0.75-0.75) | 1 | 1 (0-2) | 0.031 | 0.587 |
| SPPB domain2 | 2.5 (2-3) vs. 2 (1.25-2) | 0.23 | 3 (2-3) vs. 2 (2-2.75) | 0.404 | 0 (-0.75-0.75) | 1 | 0 (-0.75-1) | 0.792 | 0.857 |
| SPPB domain3 | 2 (2-3) vs. 2 (1-2) | 0.358 | 2 (2-3) vs. 2 (1.25-2.75) | 0.719 | 0 (0-0) | 0.773 | 0 (0-1) | 0.233 | 0.319 |
| FES | 39 (30-44.5) vs. 33 (27.75-39.5) | 0.762 | 35 (32.25-39) vs. 34 (24.5-40.25) | 0.94 | 0 (-2.25-1.5) | 0.528 | 0 (-1.5-1.75) | 1 | 0.722 |
| IADL | 7 (6.25-8) vs. 7 (6.25-7) | 0.721 | 7 (6-8) vs. 6.5 (6-7) | 0.491 | 0 (0-0) | 0.586 | 0 (0-0) | 0.773 | 1 |
| mCTSIB | 1.7 (1.5-1.79) vs. 1.59 (1.46-2.11) | 0.705 | 1.53 (1.43-1.77) vs. 1.4 (1.32-1.69) | 0.472 | -0.26 (-0.33-0.02) | 0.103 | -0.2 (-0.48--0.09) | 0.027 | 0.781 |
| EOFS | 0.62 (0.45-0.66) vs. 0.66 (0.59-0.73) | 0.121 | 0.64 (0.52-0.69) vs. 0.46 (0.35-0.59) | 0.031 | 0.03 (-0.06-0.11) | 0.557 | -0.24 (-0.44--0.09) | 0.01 | 0.225 |
| ECFS | 1.39 (0.97-2) vs. 1.34 (1.13-1.73) | 0.853 | 1.3 (0.9-1.57) vs. 1.01 (0.78-1.18) | 0.326 | -0.06 (-0.21-0.28) | 0.646 | -0.53 (-0.71-0.08) | 0.064 | 0.59 |
| EOFoS | 1.36 (1-1.69) vs. 1.52 (1.21-1.69) | 0.472 | 1.1 (0.95-1.35) vs. 1.2 (1.02-1.39) | 0.57 | -0.19 (-0.39--0.04) | 0.092 | -0.31 (-0.42--0.07) | 0.024 | 0.473 |
| ECFoS | 3.63 (3.12-3.83) vs. 3.52 (2.96-4.38) | 1 | 3.06 (2.67-3.97) vs. 3.04 (2.88-3.69) | 0.791 | -0.6 (-1.06-0.12) | 0.193 | -0.73 (-1-0.28) | 0.557 | 1 |
| Katz | 6 (5-6) vs. 6 (5.25-6) | 0.558 | 5 (5-6) vs. 6 (6-6) | 0.13 | 0 (0-0) | 1 | 0 (0-0) | 1 | 0.373 |
Table 1: The main statistical table of the analysis outcomes, depicting comparisons between controls vs. cases pre and post, as well as paired comparisons between post vs. pre in controls and cases separately. An ANCOVA procedure testing either confirms the outcomes or not. Significant p-values are depicted as bold.
miniBEST
Pre-scores were not found to be statistically significantly different between the control and case: 14.5 (12.25-16) vs. 13.5 (11.5- 15.75), respectively (p=0.703). The same also holds for the post- scores: 14 (12-16.75) vs. 16.5 (16–17.75), respectively (p=0.061). The paired analysis did not reveal a statistically significant difference in control between pre-vs. Post-intervention, with a post-pre difference of 0 (-0.75-0), and p=0.572, but did reveal a difference in case: 3 (3-5.5), p=0.006. A non-parametric Analysis of Covariance (ANCOVA) confirm a statistically significantly difference for the whole procedure (p=0.039). The results show a statistically significant difference in the case group before and after the intervention, (Figure 2). The domain 4 of the mini- BEST which corresponds to the dynamic gait is the one with more impact from the protocol in control vs. case comparison with a p=0.034.
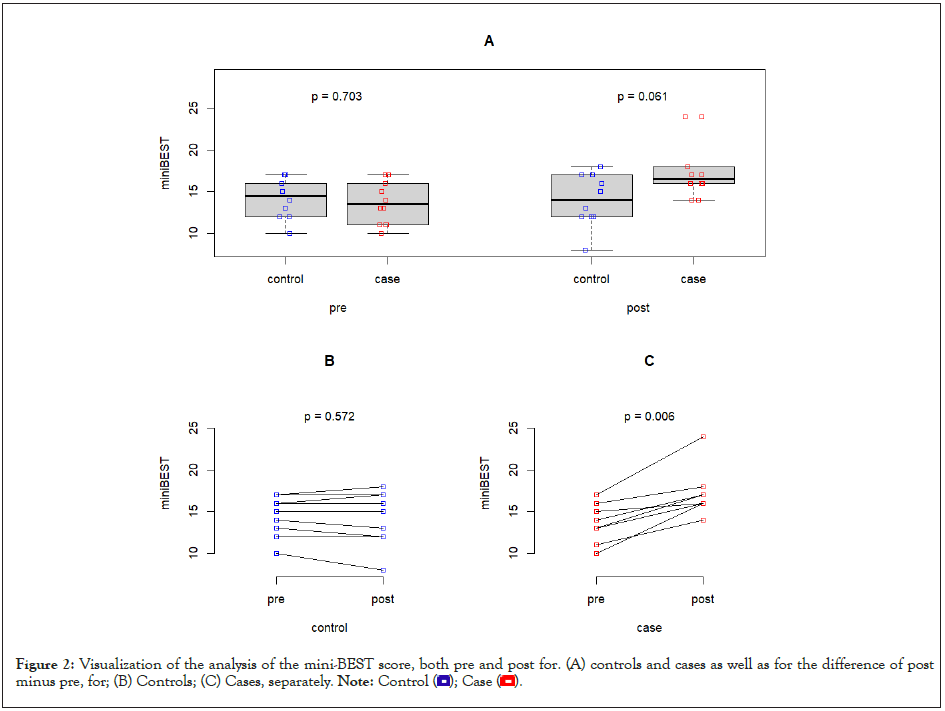
Figure 2: Visualization of the analysis of the mini-BEST score, both pre and post for. (A) controls and cases as well as for the difference of post
minus pre, for; (B) Controls; (C) Cases, separately. Note: Control 
Short Physical Performance Battery (SPPB)
Pre-scores were not found to be statistically significantly different in control vs. case: 8 (5.25-9.75) vs. 5.5 (4.25-6), respectively (p=0.078). The same holds for post-scores: 7.5 (6.25-9) vs. 7 (6- 8.75), respectively (p=0.702). Paired analysis did not disclose a statistically significantly difference in control between pre vs. post, with a post-pre difference of 0 (-1-1.5), p=1, but did reveal a difference in case: 1 (0-2), p=0.031. Non-parametric Analysis of Covariance (ANCOVA) did not confirm statistically significantly difference for the whole procedure (p=0.857). The results show a statistically significant difference in the case group before and after the intervention, p=0.02, (Figure 3), with the first task that evaluates balance to be the most impacted with a p=0.031.
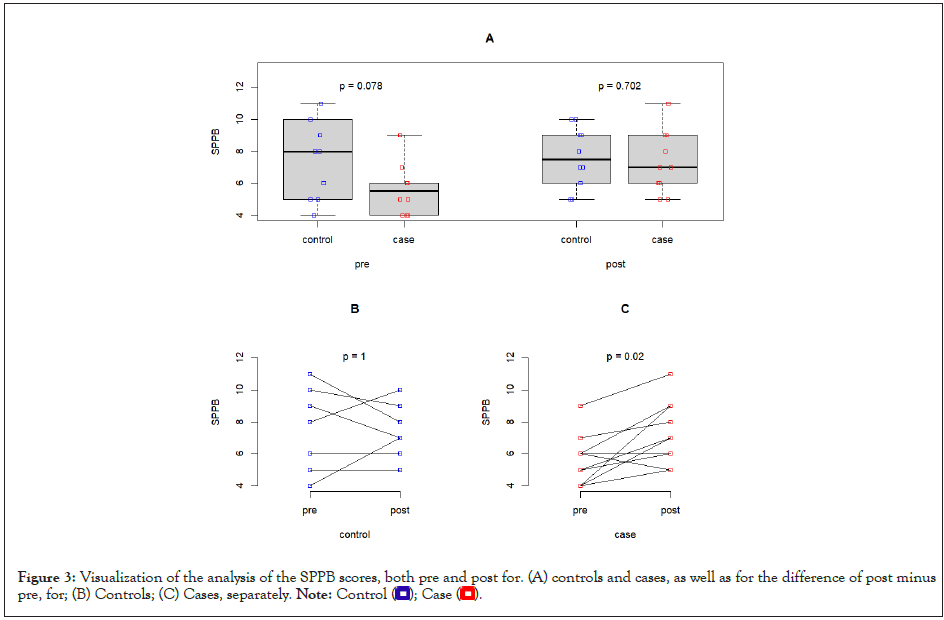
Figure 3: Visualization of the analysis of the SPPB scores, both pre and post for. (A) controls and cases, as well as for the difference of post minus
pre, for; (B) Controls; (C) Cases, separately. Note: Control 
mCTSIB
Pre-scores were not found to be statistically significantly different in control vs. case: 1.7 (1.5-1.79) vs. 1.59 (1.46-2.11), respectively (p=0.705). The same holds for post-scores: 1.53 (1.43-1.77) vs. 1.4 (1.32-1.69), respectively (p=0.472). Paired analysis did not disclose a statistically significantly difference in control between pre vs. post, with a post-pre difference of -0.26 (-0.33 -0.02), =0.103, but did reveal a difference in case: -0.2 (-0.48 -0.09), p=0.027. Non- parametric Analysis of Covariance (ANCOVA) did not confirm a statistically significant difference for the whole procedure (p=0.225). The results show a statistically significant difference in the case group before and after the intervention (Figure 4). The 2 open Eyes tasks whether in Firm (EOFS) or in Foam Surface (EOFoS) where mainly impacted by the protocol p=0.01 and p=0.024.
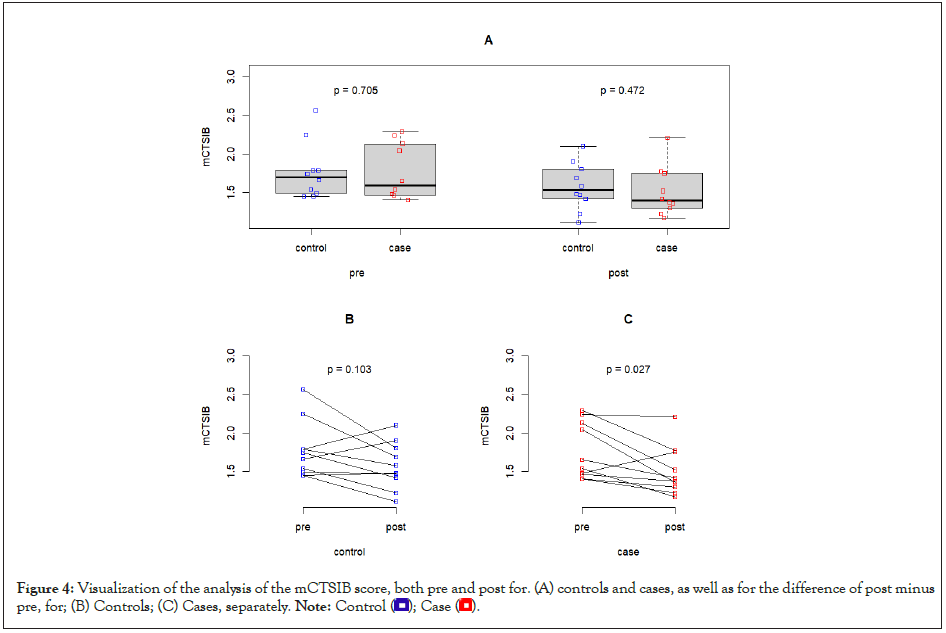
Figure 4: Visualization of the analysis of the mCTSIB score, both pre and post for. (A) controls and cases, as well as for the difference of post minus
pre, for; (B) Controls; (C) Cases, separately. Note: Control 
The other parameters, Hand grip, ADL’s, gait speed, MMSE, GDS, MNA, (p=0.825, p=1,00, p=0.085, p=0.422, p=0.851, p=1,000, and p=0.409, respectively) showed no statistical difference.
Compliance
A statistically significant difference (p<0.001) showed that compliance was achieved. The % of patients that adhered to the protocol was 96%.
This was a Randomized Controlled Trial (RCT) study regarding the effectiveness of an exercise protocol for fall prevention in elderly women living in a community with a dynamic platform. Based on the results of our study, we can conclude that dynamic platform exercise programs are effective (mini-BEST, p<0.006; mCTSIB, p<0.02; SPPB, p<0.02) in balance rehabilitation for falls. The tests used in our study to evaluate balance demonstrated a statistically significant difference pre and post-intervention. Among the four known domains of the mini-BEST (Anticipatory, Reactive Postural Control, Sensory Orientation, and Dynamic Gait), Sensory orientation and dynamic gait showed statistically significant results (p=0.012 and p=0.028, respectively). We can hypothesize that sensory adaptations and dynamic components are the first to respond to the challenge; anticipatory and postural responses need more time to be affected. We believe that time is probably the variable because the platform specifically addresses anticipatory responses and postural control reactions. The SPPB, which evaluates overall motor function, was also positively impacted, mostly in the subdomain of balance (p=0.03), as expected. The mCTSIB a sensory tool that evaluates balance was also positively impacted by the intervention and mainly the 2 domains with open eyes whether in firm or in foam surface (p=0.01 and p=0.024), the explanation could be that the closed eyes domains are more difficult tasks for older women to be impacted in such a short time.
This conclusion is also consistent with a recent meta-analysis of 2021 that evaluated fall prevention strategies and concluded that exercise in a single intervention was most strongly associated with a reduction in fall rate, with a reduction in the number of fallrelated fractures [26]. The exercise protocols used in this metaanalysis did not incorporate platform protocols.
The second critical point that emerged from this study was very good compliance. Of the patients who started the protocol, only two did not continue (p<0.001, 96%). The first was due to a health problem that required immediate treatment, and the second stopped for personal reasons for a brief time and came back. Excellent compliance with platform exercises is not always observed in other exercise programs Hanley [27], (reported compliance 60%), while 78.5%, 95% CI: 72.8%-84.2% came from the meta-analysis of Zhao [8]. We cannot determine the exact reasons for these favorable results, but we can hypothesize that 2 was the main reason. One is motivation built by immediate feedback from the program when achieving a goal and progressing to a more difficult level. The second is the personalized approach, the relaxing and intimate environment with the presence of only the therapist to ensure safety and comfort. In the population studied the majority of participants were of the more aged and vulnerable group of over 75, they are the group that falls more often, and they are the ones with the lowest compliance. Enrolling them in exercise group programs was always difficult because they felt ashamed of their performance (as stated by them), and the alternative of an individualized supervised program was very appealing to them.
There is not much in the literature concerning exercises in BIODEX dynamic platforms. We found only the following programs.
• A sample of 18 seniors living in the community in a Pakistani region through a Randomized Controlled Trial (RCT) included nine in the intervention group and nine in the control group. The elderly received 8 weeks of treatment three times a week for 30-45 min. The age group ranged from 50 to 85 years. The programs included weight-shift training and stability limits. The results showed a statistically significant improvement in the intervention group (p<0.001), whereas no improvement was observed in the control group (p>0.05). The population studied showed differences in the Berg Balance test, Biodex Fall Risk Score, and Timed Up and Go test. There was a difference in the Timed Up and go test between the groups before the intervention, while in all the tests after the intervention, there was improvement in the intervention team [26].
• An RCT study in children 5-8 years with diplegia of both sexes. The protocol consisted of 12 sessions three times a week. The results showed a statistically significant improvement in the intervention group (p<0.05), which, in addition to classical physiotherapy, also performed a program on the BBS platform, whereas the control group only performed classical physiotherapy [28].
• In elderly patients with diabetic polyneuropathy, an RCT was performed with 34 patients in the intervention and control groups. Both groups were measured at the beginning of the study using the Berg Balance Test, Timed Up and Go test, and Fall Risk Test. The intervention group 30 min three times a week for 10 sessions with the protocol “Stability Training in Standing Position”. The results of TUG p=0.01; Berg Balance=0.04; Fall Risk Test p=0.002 in the intervention group the control group did not show a significant difference [29].
• RCT in multiple sclerosis. Thirty patients with multiple sclerosis or secondary progression were recruited into two groups. Strength and balance measurements were performed with Manual Muscular Testing, Timed up and go, modified as worth, Romberg, and Berg Balance Test. The intervention team after 24 sessions of 2 times a week for 12 weeks in standing stability training. No significant difference was found in the intervention group (TUG=0.003 BBS, p>0.05) [30].
• Older adults living in institutional structures were divided into two groups of 20 people each. Measurements were made before and after the intervention, which was the FES-I (Fear of Falling) and dynamic balance test on the platform (Fall Risk Test). The intervention team held 2 sessions on the platform for 12 weeks. In the intervention group, there was an improvement in dynamic balance, as shown by the Fall Risk Test, and a moderate difference with the control group in Fes-I (8 points) [31].
The programs used in these studies were extremely variable; however, they used a way to challenge balance and measured the effects with well-established balance evaluation scales. All but the MS protocol showed statistically significant differences in the intervention group. Only the protocol was clearly addressed to older people living in the community, but they had sexes, fewer participants, and a shorter period of time, but a greater time per session. They used only two modalities of the dynamic platform: Weight-shifting and limits of stability. They found a statistically significant difference between the intervention and control groups before and after intervention. All the other protocols involved patients of other age groups or with diverse diagnoses, and the last protocol of Gusi, et al. involved older people but was institutionalized [31].
Regarding adverse effects, only one patient reported a fall during the exercise period. This very low fall rate is in accordance with the meta-analysis by Zhao, et al., [8]. We also had no accidental falls during the sessions, and the patients reported that the presence of a therapist throughout the program and the ability to grasp the platform in case of loss of balance was reassuring.
We have also noted, along with physical improvement, that there was an improvement in the patients’ self-confidence. This qualitative data is difficult to measure with a valid scale; it was what the patients shared with us in everyday life. The only objective scale for qualitative data was the fear of falling FES scale, which showed no significant difference but measured fear and not confidence.
We also wanted to see if exercise in such a short period could affect all other components of the CGA, such as hand grip, ADL, IADL’s usual gait speed, MMSE, GDS, and MNA scores (p=0.153, p=1,00, p=0.773, p=0.25, p=0.724, p=0.28, p=0.12). The analysis showed no difference before and after the exercise protocol in the other components, and no difference was expected, as the program was not aimed at any of those. This finding reinforces the already proven concept that, to have an impact in any domain, the intervention must be focused on a particular domain.
As for the limitations of this study, gender differences were not addressed, and we have demonstrated the validity and reliability of the test in the elderly female population living in the community, and we do not know if this can be applied to the male. In addition, the population came from a single center that makes it a convenience sample, and further studies are needed to assess the elderly living in shelter structures or nursing homes. However, as an added value to this study, the population studied was well defined and had no mixed institutionalized and not older adults, which is of added value.
Regarding the device, there are two limiting factors for its extensive use. One is the acquisition cost, which limits the availability. Attitude analysis systems are fast, standard, and do not require experience in operation; however, this entails a cost that clinical trials performed with little or no equipment do not have. There were also no reference values or normal limits of the device protocols for the correct reporting of the findings. However, they can be used in more vulnerable groups of the elderly owing to their safety and personalized approach. We conclude that fall prevention exercises on a dynamic platform are effective and have good compliance. Platform exercise is an ideal start for older community dwellers to find in a protected environment the beginning of the thread that will lead them to a change of lifestyle and, therefore, to long-term health.
The ethical committee of the University Hospital approved the protocol (no. 621/15-12-17) for the enrolment of a patient in the study, and written consent was necessary after a detailed explanation of the procedures and the probable harm.
The data associated with the paper are not publicly available but are available from the corresponding author upon reasonable request.
No conflict of interest.
Funding was received from the ELKE (SPECIAL RESEARCH FUNDS ACCOUNT) of the University.
Author 1, Author 1,3,4 have provided substantial contributions to the conception or design of the manuscript and to the acquisition and interpretation of the data. Author 2, Analysis of the data and interpretation.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Antoniadou E, Lakoumentas J, Panagiotopoulos E, Zampakis P (2024) Improving Compliance and Effectiveness in Fall’s Prevention, using a Dynamic Balance Training Platform: A Randomized Control Trial-A Feasibility Study. Int J Phys Med Rehabil. 12:716.
Received: 16-Jan-2024, Manuscript No. JPMR-23-29179; Editor assigned: 18-Jan-2024, Pre QC No. JPMR-23-29179 (PQ); Reviewed: 02-Feb-2024, QC No. JPMR-23-29179; Revised: 12-Feb-2024, Manuscript No. JPMR-23-29179 (R); Published: 20-Feb-2024 , DOI: 10.35248/2329-9096.24.12.716
Copyright: © 2024 Antoniadou E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.