International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2022)
Dressing ability is important to maintain a satisfactory standard of living. There is a high probability that dressing ability becomes impaired in stroke patients and the effects are quite serious. Approximately 49% of stroke patients are reported to be unable to independently put on their clothes within 3 weeks after the onset of stroke. When the dressing ability is impaired, restoration of this ability becomes a critical issue. Dressing support is time consuming and often causes physical fatigue of the support person. Occupational therapists usually spend a great deal of time performing interventions to improve patient’s dressing ability. For effective restoration of dressing ability, setting a reliable and practical target representing the dressing ability is very important for stroke patients in occupational therapy.
Stroke patients; Physical fatigue; Occupational therapy; Rehabilitation
To evaluate dressing ability, the barthel index, which is used to measure the assistance level required for patients, or the functional independence measure has been used as the evaluation index. However, a previous study indicates that some stroke patients do not want to dress themselves even if they can do so by themselves. Another survey shows the gaps between dressing capability and Activities of Daily Living (ADL) performance for stroke patients. Many hospitalised patients put on clothes with assistance from others to save time, even though they can wear them independently if time permits. Despite the useful scales of the barthel index and functional independence measure, patient’s willingness, caregiver’s attitude, and the situation can cause a discrepancy between the potential dressing ability and actual dressing behaviour. Thus, previous evaluation indices of dressing ability are not always useful in setting the target for restoration of dressing ability. If the time required for the patient to dress independently as an ADL and the timing of caregiver assistance in patient dressing are identified, we can use them as useful targets for occupational therapy. In fact, a report of elderly people in a long-term health care facility in Japan points out that dressing time is an important factor in the evaluation of dressing behaviour [1]. Previous studies indicate that dressing time can be an important evaluation index if it is measured adequately. On the other hand, according to a study on the skills required for an actual situation, practical ability can be achieved with fluency training. This suggests that fluency training toward a target time can be effective in the restoration of dressing ability.
From the findings of previous studies in dressing after stroke, we hypothesised that the dressing time is correlated with difficulty in dressing recognised by patients, and there is a difference between the time required for patient to dress independently as an ADL and timing of caregiver assistance in patient dressing [2]. Based on these assumptions, our study aimed to identify the following target times: The time for dressing-dependent patients to recover their dressing ability and the time for the patients to be free from the caregiver’s intervention.
Study design, participants
We conducted cross-sectional studies to identify the time required for patient’s independent dressing and timing of caregiver assistance. Thus, our study has two parts. The first part was conducted to identify the time required for stroke patients to dress themselves independently. The second part was conducted to identify the timing of assistance by caregivers. The eligibility criteria were stroke, ability of putting on a buttoned shirt independently, the ability to sit with a backrest on a wheelchair or chair for more than 20 min, 2 months or less since the stroke event, and a desire to participate in this study. Nurses were selected as caregivers in this study because they have more frequent contact with the patients than occupational therapists.
Time required for dressing
Patients were classified dichotomously into an independent group or dependent group by judging their actual dressing ability in the hospital ward. For this judgement, the occupational therapist in charge interviewed both the nurse in charge and the patient about the patient’s dressing ability. If both the nurse and the patient stated that the patient could put on the shirt independently, the patient was categorised as independent. If either or both of them stated that assistance was required in dressing, the patient was categorised as dependent. The reason for interviewing the nurse and the patient was to avoid excessive influence on the judgement from the caregiver side. We chose the buttoned shirt for this study because it is one of the common and standard clothes for stroke patients in the hospital.
Dressing time was measured using a stopwatch. As reported in our previous study, our measurement method had high inter- and intra-rater reliability and validity. The time required to dress was measured once for each patient. All patients sat on a wheelchair or chair during the test. We instructed the patients to put on a buttoned shirt as they would normally do. The time from handing the shirt to the patient to the instance when all buttons were closed was measured with an accuracy of 0.01 seconds. Rounded- off values were used for data analysis.
The time required for dressing and independence of dressing were the primary outcomes of this study. After measuring the dressing time, difficulty in dressing was evaluated by patient interviews using a Visual Analogue Scale (VAS). The VAS ranged from 0 (no difficulty) to 100 (maximum difficulty) and involved a 100-mm straight horizontal line. The patients marked the point that they felt their current ability to dress on this line. The VAS score was determined by measuring from the left end of the line to the marked point (in mm).
Physical and cognitive functions
Patient characteristics were collected in the first part of study, including age, sex, clinical categories, glasgow coma scale score, range of motion disturbance, motor palsy, sensory disturbance, grip strength on the non-paretic side, mini-mental examination score, aphasia, apraxia, attention disorder, and unilateral spatial neglect [3-7]. The severity of motor palsy was assessed using the Brunnstrom motor recovery stage. This scale uses seven motor recovery stages (stage 1, flaccidity; stage 2, spasticity appears; stage 3, increased spasticity; stage 4, decreased spasticity; stage 5, complex movement combinations; stage 6, spasticity disappears; stage 7, normal function returns).
We further categorised the patients into the following four groups: Brunnstrom motor recovery stages 1 and 2, severe; stages 3 and 4, moderate; stages 5 and 6, mild; and stage 7, normal. Sensory disturbance was assessed based on the presence or absence of deep and tactile sensations. The mini-mental examination was used as a screening tool for global cognitive functioning. The resulting score (30, maximum score; <24, impaired) was determined using a questionnaire with 11 items. A two-step ordinal scale (0-1) was applied to each item, and a higher score indicated better cognitive function. The presence of aphasia was assessed using the standard language test of aphasia. The scale involved the standardised test battery commonly used for Japanese patients with stroke and consisted of 26 items (6-point scale), and aphasia severity was rated based on 11 stages (0, most severe; 10, normal). The presence of apraxia was evaluated using the apraxia subtest of the Japanese version of the western aphasia battery [8]. This scale consists of 20 items (3-point scale), and a higher score indicated better function. A cancellation task was used to examine the presence of attention disorder. This test has 60 targets and 360 randomly arranged shapes. The presence of unilateral spatial neglect was assessed by Albert’s test [9]. This test involves a widely used scale for assessing the presence of unilateral spatial neglect and has 40 targets (36, maximum score; <33, impaired).
Timing of caregiver assistance
Assessment of the timing of assistance had two steps. First, we used a video camera to record 6 stroke patients dressing. Second, the nurses as the ratters viewed the videos and determined the time when they would have assisted the patient. The patients were seated facing the camera and 2 m away from the camera (CANON IXY190). The video camera was mounted on a tripod. We instructed the patients to put on a buttoned shirt as usual. The buttoned shirt commonly used by all patients in the hospital was used. The patients in our study wore the same type of garments [10]. We instructed the nurses to stop the stopwatch when they would start to provide assistance for the dressing patient. Twenty- two nurses viewed the videos of stroke patients dressing, and for each patient, we measured the start time of assistance twice using a stopwatch (Seiko S056 100 lap memory stopwatch). The time elapsed from the moment the patient received the shirt to the start of nurse assistance was measured with an accuracy of 0.01 seconds. Rounded values were used for data analysis. The start time of assistance was measured sequentially for each nurse. When the nurses decided to assist before completion of dressing, we asked them about the reason why they decided to assist the patient.
Data analysis
Differences in the time required for putting on and buttoning a shirt were analysed by the t-test. We used a Receiver-Operating Characteristic (ROC) curve to examine whether the time to complete dressing was a good predictor of independence [11]. The area under the receiver operating characteristic curve was calculated to assess the clinical utility of the dressing time as a predictor of patient independence. The cut-off point for prediction of independence and nurse assistance was defined as the best balance between positive and negative predictive values. Furthermore, the correlation between the duration required to dress and the VAS score of stroke patients was examined using Spearman’s rank correlation co-efficient (r) to assess the relationship between dressing time and perception of difficulty in dressing.
In addition, we analysed the data as to why the nurses would assist in dressing the patient before the patient would have finished doing so independently. Data were analysed using text mining. First, words were extracted from the entire description; specific words that were used many times were automatically selected. Second, similar patterns of words were examined using the hierarchical cluster analysis. We grouped similar and frequently used keywords using cluster analysis and selected the keywords that were significantly used in a provided cluster. Kruskal-Wallis tests were used to compare the start time of intervention with each cluster. Analyses were performed using SPSS (version 17; IBM Corp., Armonk, NY, USA). p<0.05 was considered statistically significant. We used the free software KH Coder (version 2.Beta.31d) to calculate the frequency of words in the data.
In the first part of the study performed between April 1, 2011, and April 1, 2013, 328 consecutive inpatients with stroke from our hospital were recruited to investigate a target dressing time for independent dressing. Of the 483 consecutive stroke patients who were initially recruited, 317 were excluded for the following reasons: Inability to dress (n=155), inability to comprehend instructions for dressing (n=138), and missing data (n=24). As a result, 166 patients with stroke were deemed eligible to participate in this cross-sectional study (Figure 1).
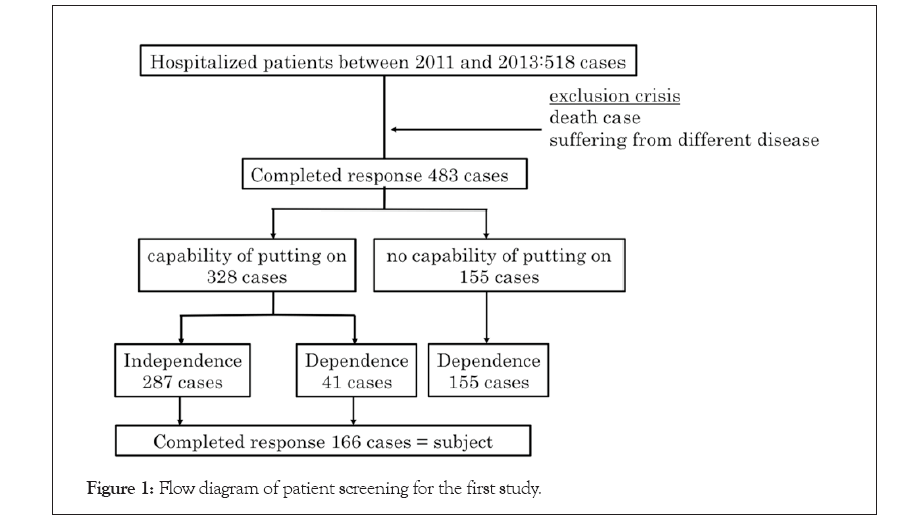
Figure 1: Flow diagram of patient screening for the first study.
Among them, 132 (79.5%) patients were classified as independent and 34 (20.5%) patients were classified as dependent. Note that 34 of 166 (20.5%) patients classified as dependent in this study had the potential ability to dress independently. The characteristics of the 166 participants are summarised in Table 1. There were 69 women and 97 men, and the mean age was 67.7 ± 11.9 years. Among the 166 participants, 118 patients had cerebral infarction, 24 had cerebral haemorrhage, 24 had subarachnoid haemorrhage, 27 had right hemiplegia, and 36 had left hemiplegia. The average time since the stroke event was 27.8 ± 38.1 days. Gender, clinical categories, and presence of range of motion disturbance were similar between the two groups; however, age, the Glasgow Coma Scale score, Brunnstrom motor recovery stage, tactile and deep sense, grip on the non-paretic side, Mini-Mental Examination score, aphasia, apraxia, attention disorder, and unilateral spatial neglect were significantly different between the independent and dependent patient groups (p ≤ 0.001). The time required to dress was significantly shorter for independent patients (median 31.4 seconds; interquartile range 24.6-43.2 seconds) than for dependent patients (median 226.0 seconds; interquartile range 191.6-523.5 seconds) (p<0.05).
| Characteristic | Independent group | Dependent group | P-value |
|---|---|---|---|
| Patients | 132 | 34 | |
| Age (y) | 66.3 ± 11.2 | 74.6 ± 12.1 | <0.001 |
| Gender: Male/female | 79/53 | 18/16 | 0.833 |
| Clinical categories | |||
| Infarction/cerebral hemorrhage/subarachnoid hemorrhage | 97/19/16 | Â 21/5/8 | 0.079 |
| Glasgow coma scale (points) | 14.9 ± 0.4 | 14.0 ± 1.2 | <0.001 |
| Brunnstrom motor recovery stage | |||
| Arm, severe/moderate/mild/normal | 3/1/48/80 | Â 4/3/14/13 | <0.001 |
| Finger, severe/moderate/mild/normal | 3/2/47/80 | Â 4/1/16/13 | 0.001 |
| Sensory disturbance | |||
| Tactile sensory, present/absent/difficult exact examination | 17/115/0 | Â 7/24/3 | 0.002 |
| Deep sensory, present/absent/difficult exact examination | 8/124/0 | Â 5/26/3 | <0.001 |
| Grip strength (non-paretic side) (kg) | 27.5 ± 12.1 | 13.8 ± 8.4 | <0.001 |
| Mini-mental examination (points) | 28.1 ± 10.4 |  17.0 ± 7.0 | <0.001 |
| Aphasia, present/absent/difficult exact examination | 17/115/0 | 7/26/1 | <0.001 |
| Apraxia, present/absent/difficult exact examination | 1/130/1 | Â 3/30/1 | <0.001 |
| Attention disorder, present/absent/difficult exact examination | 33/98/1 | Â 29/4/1 | <0.001 |
| Unilateral spatial neglect, present/absent/difficult exact examination | 5/126/1 | Â 7/26/1 | <0.001 |
Table 1: Characteristics of the patients in the first part of study.
The second part of the study was performed to study the timing of nurse assistance in patient dressing. We used video data of six patients who showed different disability levels to clarify the timing of nurse assistance when the stroke patients put on a buttoned shirt. Table 2 shows the characteristics of the 6 patients. Two patients (33.3%) were regarded as independent and four patients (66.7%) were dependent in performing ADL. The median age of participants was 72.5 (interquartile range, 69.8-75.3) years. There were three patients with cerebral infarction, three patients with cerebral haemorrhage, two patients with right hemiplegia, and two patients with left hemiplegia. The median elapsed time since stroke onset was 19.5 (15.0-22.5) days. Raters of video analysis were 22 nurses who worked in the hospital. The median age of raters was 28.0 (25.8-29.3) years. Their mean number of years of experience in the nursing field was 4.5 (3.8-7.5) years.
| Participant | Age (y) | Gender | Clinical categories | Time since onset, (days) | Brunnstrom motor recovery stage (arm-finger) | Sensory disturbance | Attention disorder | Unilateral spatial neglect | MMSE | FIM (upper dressing) | Time required to put on clothes (sec) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41 | M | Infarction | 14 | V-II | Absent | Absent | Absent | 28 | 7 | 22.4 |
| 2 | 69 | M | Infarction | 11 | VI-VI | Absent | Absent | Absent | 23 | 6 | 58.5 |
| 3 | 76 | M | Infarction | 26 | II-I | Absent | Absent | Absent | 27 | 4 | 118.4 |
| 4 | 73 | F | Cerebral haemorrhage | 21 | V-II | Absent | Present | Absent | 22 | 3 | 148.4 |
| 5 | 84 | M | Cerebral haemorrhage | 18 | II-II | Absent | Present | Absent | 15 | 3 | 188.5 |
| 6 | 72 | F | Cerebral haemorrhage | 23 | V-II | Absent | Present | Absent | 12 | 1 | 255.5 |
Table 2: Characteristics of the patients in the second part of study.
Time required for dressing
Dressing time data were plotted as a ROC curve, and the calculated area under the ROC curve was 0.96 (Figure 2). The highest positive predictive value was 59.3 seconds in dressing time (positive predictive value=0.54, negative predictive value=0.71, sensitivity=0.91, specificity=0.85). The highest negative predictive value was 29.9 seconds in dressing time (positive predictive value=0.52, negative predictive value=0.81, sensitivity=0.97, specificity=0.47). A cut-off value of 177.0 seconds to dress showed the best balance of the positive and negative predictive values and showed good accuracy (86.0%) for the stroke patients (Figure 3). The sensitivity and specificity were 0.828 and 1.000, respectively. Patients from both the independent (n=132) and dependent (n=6) groups completed dressing within 177.0 seconds (n=138); however, patients who required more than 177.0 seconds to dress were all from the dependent group (n=28). The six dependent patients who dressed within 177.0 seconds had attention disorders and were commonly observed to demonstrate risky behaviours in the ward (as noted in their medical records).
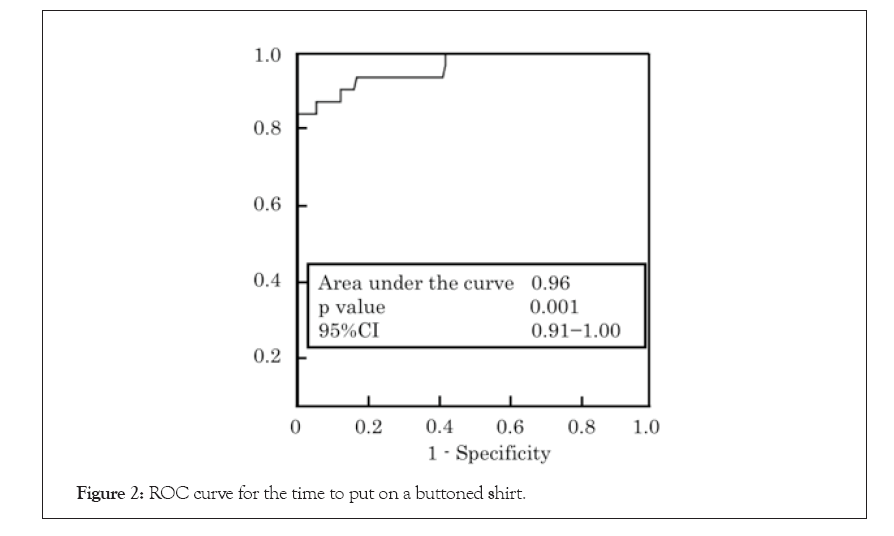
Figure 2: ROC curve for the time to put on a buttoned shirt.
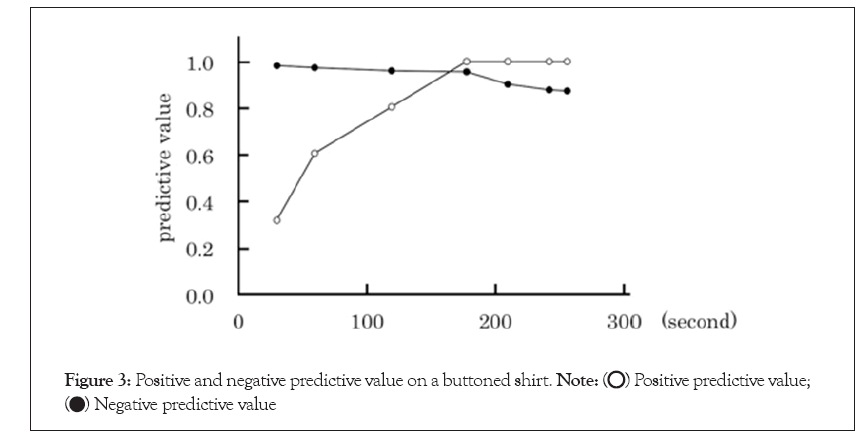
Figure 3: Positive and negative predictive value on a buttoned shirt.
The correlation coefficient for dressing duration and VAS score was high (r=0.78, p<0.001). Further, the median VAS score for difficulty in dressing was significantly lower in patients who could dress within 177.0 seconds than in patients who required more than 177.0 seconds (p<0.05) (Figure 4).
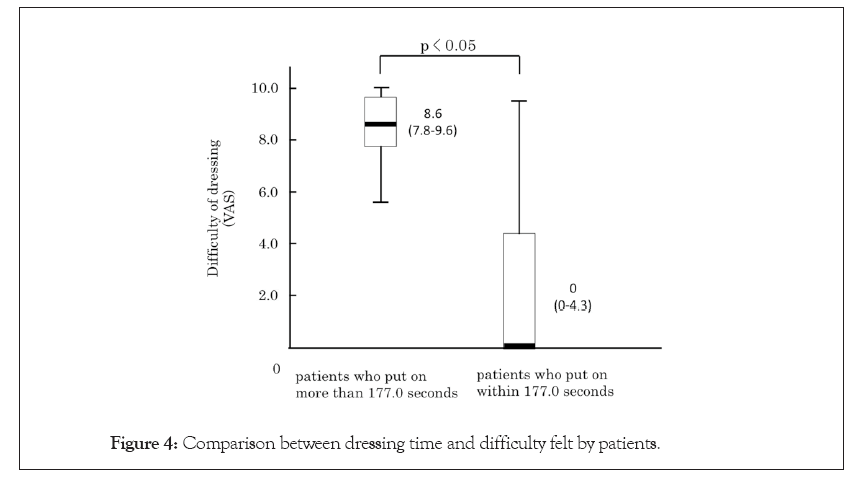
Figure 4: Comparison between dressing time and difficulty felt by patients.
Timing of caregiver assistance
The time required for the six stroke patients to put on the buttoned shirt was 22.4, 58.5, 118.4, 148.4, 188.5 and 255.5 seconds. All nurses did not assist the patients with dressing time of 22.4 or 58.5 seconds. On the other hand, all nurses assisted the patients with dressing time of 188.5 and 255.5 seconds. The median times for the starts of assistance were 26.5 (range, 21.5-30.8) seconds for the patient with a dressing time of 188.5 seconds and 25.0 (range, 22.4-31.0) seconds for the patient with a dressing time of 255.5 seconds. Some nurses provided assistance to patients with dressing times of 118.4 and 148.4 seconds. The median times for the start of assistance was 38.4 (range, 23.4-44.4) seconds for the patient with a dressing time of 118.4 seconds and 23.4 (range, 17.5-28.4) seconds for the patient with a dressing time of 148.4 seconds. The Intra-Class Correlation coefficients (ICC) of the start time of assistance were ICC (1,1) 0.88 and ICC (1,2) 0.94. The ROC curve was illustrated for the time required to dress as an indicator of patient’s independence according to the caregiver’s view point. A cut-off value of 88.5 seconds shows good accuracy (98.4%). The sensitivity and specificity were 1.000 and 0.898, respectively. A cut-off value of 88.5 seconds to dress showed the best balance of the positive and negative predictive values (Figure 5).
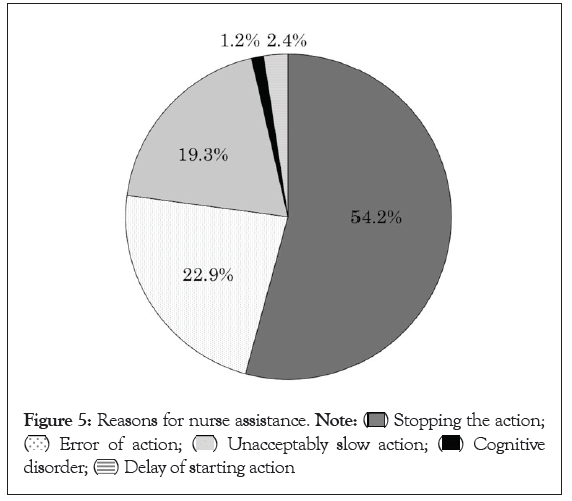
Figure 5: Reasons for nurse assistance. 


We analysed the reasons reported by the 22 nurses regarding why they started assistance before completion of the dressing activity. Text mining software KH Coder extracted 488 words of 27 types. Five major behaviours were extracted using hierarchical cluster analysis. The clusters were ‘stopping the action’, ‘error of action’, ‘unacceptably slow action’, ‘action influenced by cognitive disorder’, and ‘delay of starting action’ (Figure 5). We found no significant correlation between the dressing time and assistance start time (p>0.05).
We have studied the relationship between the dressing time and patient independence and the relationship between the dressing time and caregiver assistance start time. Our study has shown that the dressing time is correlated with difficulty in dressing recognised by the patient and the caregivers intervene in patient dressing well before the time when the patients start to recognise significant difficulty in dressing [12]. In this study, we have identified two useful targets in dressing time for stroke patient rehabilitation from standpoints of the patient and caregiver.
In the relationship between dressing time and patient independence, the dressing time was significantly shorter for independent patients than for dependent patients [13]. This result is consistent with the result of a previous study reporting that patients with motor function disorder require much more dressing time than those without the disorder.
We used ROC curve analysis to confirm that the time required to dress can be a good predictor of the level of dependence in stroke patients. The calculated AUC for the ROC curve was 0.96 for stroke patients dressing and 0.98 for caregivers’ assistance [14-19]. The approach recommended by Swets is used to evaluate AUC values, with an excellent AUC value being >0.90. According to the Swets criteria, the time required to dress (defined in this study as putting on and buttoning a shirt) can be a helpful predictor of independence in stroke patients. This is a new observation of our study, showing a clear relationship between the dressing time and patient independence from the standpoints of both the stroke patient and caregiver.
With regard to stroke patients, all patients with a time of putting and buttoning a shirt of more than 180 seconds (round number of 177.0 seconds) required assistance in dressing. On the contrary, about 95% of patients with the time of putting and buttoning a shirt of less than 180 seconds can independently dress themselves. Therefore, a cut-off value of 180 seconds can be an important criterion to judge the level of independence of stroke patients.
The time required for putting on and buttoning a shirt is correlated with the difficulty in dressing recognised by patients. The median score for dressing difficulty was significantly higher for patients who required more than 180 seconds than that for patients who required 180 seconds or less. This means that the dressing time is a good indicator of difficulty in dressing and 180 seconds in dressing time can be a target time for dependent patients in rehabilitation [20]. Kenna has shown that stroke patients usually spend their time in basic ADL (2.9 h/day) and spend significantly less time in sleep and instrumental ADL than the sample without stroke. Spending a lot of time for ADL may cause reduction of the time for instrumental ADL. Thus, efficient rehabilitation for independent dressing is highly required in medical practices. Setting a target time in patients dressing can contribute to an efficient rehabilitation.
Considering the caregiver’s assistance, positive and negative predictive values indicated that cut-off value of 90.0 seconds (round number of 88.5 seconds) was the allowable time that the caregivers could refrain from assisting stroke patients in putting and buttoning a shirt. Our results indicated that caregiver assistance was correlated to the time required for the patients to put on the buttoned shirt. The majority of the caregivers intervened when the time of putting and buttoning a shirt was more than 90 seconds [21-24]. This suggests that there is little possibility for patients with dressing time more than 90 seconds to acquire dressing independence. Several studies reported that serious functional dependence of stroke survivors often adds to the caregiver’s burden. Independence in dressing can significantly reduce caregivers’ burden. Therefore, 90 seconds to put on a buttoned shirt can be another target for independence of stroke patients from the caregiver’s perspective.
Reasons for caregivers’ assistance were categorised into five clusters, ‘stopping the action’, ‘error of action’, ‘unacceptably slow action’, ‘action influenced by cognitive disorder’, and ‘delay of starting action’, in this study. According to behaviour-analytic research, fluency was defined as a combination of accuracy and speed that characterises competent performance. Following this definition, ‘stopping the action’, ‘unacceptably slow action’, and ‘delay of starting action’ are related to the fluency of the action. Our study indicates that lack of fluency in dressing is a major factor for caregiver’s intervention. In other words, if fluency in dressing is improved, the caregivers can wait longer before intervention and the target time in dressing from the caregiver’s perspective can be longer [25]. Our result showing the importance of fluency is consistent with those of some previous studies. Fluency has been assessed important for performance of target behaviour. A report on a young man (at age 25 and 27 years) with cerebropathy due to prenatal and perinatal causes shows that intervention for fluent dressing is effective for independence. Moreover, 90 seconds is half the target time (180 seconds) for dependent patients to achieve independent dressing ability. In some way, the timing of caregivers’ assistance is considered too early and prevents patients’ proactive efforts to achieve independent dressing ability. In this sense, the caregivers should allow more time to the patient before providing assistance.
Our study provides useful and practical targets for restoration of dressing ability, but has some limitations. Our data were from a single hospitalisation. Independence in dressing can be affected by hospital functions, environments, and locations. Larger sample size for caregivers is needed for better statistical evaluations [26-29]. To increase the applicability of our findings, further studies involving a larger number of patients, nurses and hospitals are necessary.
Dressing time has a close relationship with patient independence. For stroke patients, when putting on and buttoning a shirt, 180 seconds is the first target time of dependent patients to overcome the dressing difficulties and obtain confidence to dress independently. 90 seconds is the second target time of patients to achieve dressing independence, i.e., free from the caregiver’s intervention, or to obtain independence in dressing in daily hospital life. In another aspect of the second target, caregivers are advised to wait some more time before providing assistance for developing their ability to dress themselves in ADL.
This work was supported by a Grant-in-Aid for JSPS KAKENHI 18H03133 to Makoto Suzuki.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Sasaki S, Sugimura S, Suzuki M, Omori Y, Sakakibara Y, Sashima T (2022) Impairment of Dressing Ability in Stroke Patients: An Experimental Study. Int J Phys Med Rehabil. 10:650.
Received: 25-Nov-2019, Manuscript No. JPMR-19-4986; Editor assigned: 28-Nov-2019, Pre QC No. JPMR-19-4986; Reviewed: 12-Dec-2019, QC No. JPMR-19-4986; Revised: 15-Sep-2022, Manuscript No. JPMR-19-4986; Published: 13-Oct-2022 , DOI: 10.35248/2329- 9096.22.S18.005
Copyright: © 2022 Sasaki S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited